Skin Care Encounter Form
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Diagnostic Approach to Pruritus
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by DigitalCommons@University of Nebraska University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln U.S. Air Force Research U.S. Department of Defense 2011 A Diagnostic Approach to Pruritus Brian V. Reamy Christopher W. Bunt Stacy Fletcher Follow this and additional works at: https://digitalcommons.unl.edu/usafresearch This Article is brought to you for free and open access by the U.S. Department of Defense at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in U.S. Air Force Research by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. A Diagnostic Approach to Pruritus BRIAN V. REAMY, MD, Uniformed Services University of the Health Sciences, Bethesda, Maryland CHRISTOPHER W. BUNT, MAJ, USAF, MC, and STACY FLETCHER, CAPT, USAF, MC Ehrling Bergquist Family Medicine Residency Program, Offutt Air Force Base, Nebraska, and the University of Nebraska Medical Center, Omaha, Nebraska Pruritus can be a symptom of a distinct dermatologic condition or of an occult underlying systemic disease. Of the patients referred to a dermatologist for generalized pruritus with no apparent primary cutaneous cause, 14 to 24 percent have a systemic etiology. In the absence of a primary skin lesion, the review of systems should include evaluation for thyroid disorders, lymphoma, kidney and liver diseases, and diabetes mellitus. Findings suggestive of less seri- ous etiologies include younger age, localized symptoms, acute onset, involvement limited to exposed areas, and a clear association with a sick contact or recent travel. Chronic or general- ized pruritus, older age, and abnormal physical findings should increase concern for underly- ing systemic conditions. -

3628-3641-Pruritus in Selected Dermatoses
Eur opean Rev iew for Med ical and Pharmacol ogical Sci ences 2016; 20: 3628-3641 Pruritus in selected dermatoses K. OLEK-HRAB 1, M. HRAB 2, J. SZYFTER-HARRIS 1, Z. ADAMSKI 1 1Department of Dermatology, University of Medical Sciences, Poznan, Poland 2Department of Urology, University of Medical Sciences, Poznan, Poland Abstract. – Pruritus is a natural defence mech - logical self-defence mechanism similar to other anism of the body and creates the scratch reflex skin sensations, such as touch, pain, vibration, as a defensive reaction to potentially dangerous cold or heat, enabling the protection of the skin environmental factors. Together with pain, pruritus from external factors. Pruritus is a frequent is a type of superficial sensory experience. Pruri - symptom associated with dermatoses and various tus is a symptom often experienced both in 1 healthy subjects and in those who have symptoms systemic diseases . Acute pruritus often develops of a disease. In dermatology, pruritus is a frequent simultaneously with urticarial symptoms or as an symptom associated with a number of dermatoses acute undesirable reaction to drugs. The treat - and is sometimes an auxiliary factor in the diag - ment of this form of pruritus is much easier. nostic process. Apart from histamine, the most The chronic pruritus that often develops in pa - popular pruritus mediators include tryptase, en - tients with cholestasis, kidney diseases or skin dothelins, substance P, bradykinin, prostaglandins diseases (e.g. atopic dermatitis) is often more dif - and acetylcholine. The group of atopic diseases is 2,3 characterized by the presence of very persistent ficult to treat . Persistent rubbing, scratching or pruritus. -
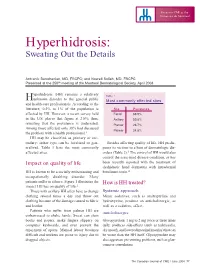
Hyperhidrosis: Sweating out the Details
Focus on CME at the Université de Montréal Hyperhidrosis: Sweating Out the Details Antranik Benohanian, MD, FRCPC; and Nowell Solish, MD, FRCPC Presented at the 250th meeting of the Montreal Dermatological Society, April 2003 yperhidrosis (HH) remains a relatively Table 1 Hunknown disorder to the general public Most commonly affected sites and health-care professionals. According to the literature, 0.5% to 1% of the population is Site Prevalence affected by HH. However, a recent survey held Facial 68.9% in the U.S. places that figure at 2.8%; thus, Axillary 50.8% revealing that the prevalence is underrated. Plantar 28.7% Among those affected, only 38% had discussed Palmar 24.8% the problem with a health professional.1 HH may be classified as primary or sec- ondary; either type can be localized or gen- Besides affecting quality of life, HH predis- eralized. Table 1 lists the most commonly poses its victims to a host of dermatologic dis- affected sites. orders (Table 2).3 The control of HH would also control the associated disease condition, as has Impact on quality of life been recently reported with the treatment of dyshidrotic hand dermatitis with intradermal HH is known to be a socially embarrassing and botulinum toxin.4 occupationally disabling disorder. Many patients suffer in silence. Figure 1 illustrates the How is HH treated? impact HH has on quality of life.2 Those with axillary HH often have to change Systemic approach clothing several times a day and throw out Minor sedatives, such as amitriptyline and clothing because of the damage caused to fabric hydroxyzine, produce an anticholinergic, as and leather. -

Red, Weeping and Oozing P.51 6
DERM CASE Test your knowledge with multiple-choice cases This month–9 cases: 1. Red, Weeping and Oozing p.51 6. A Chronic Condition p.56 2. A Rough Forehead p.52 7. “Why am I losing hair?” p.57 3. A Flat Papule p.53 8. Bothersome Bites p.58 4. Itchy Arms p.54 9. Ring-like Rashes p.59 5. A Patchy Neck p.55 on © buti t ri , h ist oad rig D wnl Case 1 y al n do p ci ca use o er sers nal C m d u rso m rise r pe o utho y fo C d. A cop or bite ngle Red, Weleepirnohig a sind Oozing a se p rint r S ed u nd p o oris w a t f uth , vie o Una lay AN12-year-old boy dpriesspents with a generalized, itchy rash over his body. The rash has been present for two years. Initially, the lesions were red, weeping and oozing. In the past year, the lesions became thickened, dry and scaly. What is your diagnosis? a. Psoriasis b. Pityriasis rosea c. Seborrheic dermatitis d. Atopic dermatitis (eczema) Answer Atopic dermatitis (eczema) (answer d) is a chroni - cally relapsing dermatosis characterized by pruritus, later by a widespread, symmetrical eruption in erythema, vesiculation, papulation, oozing, crust - which the long axes of the rash extend along skin ing, scaling and, in chronic cases, lichenification. tension lines and give rise to a “Christmas tree” Associated findings can include xerosis, hyperlin - appearance. Seborrheic dermatitis is characterized earity of the palms, double skin creases under the by a greasy, scaly, non-itchy, erythematous rash, lower eyelids (Dennie-Morgan folds), keratosis which might be patchy and focal and might spread pilaris and pityriasis alba. -

Photodermatoses Update Knowledge and Treatment of Photodermatoses Discuss Vitamin D Levels in Photodermatoses
Ashley Feneran, DO Jenifer Lloyd, DO University Hospitals Regional Hospitals AMERICAN OSTEOPATHIC COLLEGE OF DERMATOLOGY Objectives Review key points of several photodermatoses Update knowledge and treatment of photodermatoses Discuss vitamin D levels in photodermatoses Types of photodermatoses Immunologically mediated disorders Defective DNA repair disorders Photoaggravated dermatoses Chemical- and drug-induced photosensitivity Types of photodermatoses Immunologically mediated disorders Polymorphous light eruption Actinic prurigo Hydroa vacciniforme Chronic actinic dermatitis Solar urticaria Polymorphous light eruption (PMLE) Most common form of idiopathic photodermatitis Possibly due to delayed-type hypersensitivity reaction to an endogenous cutaneous photo- induced antigen Presents within minutes to hours of UV exposure and lasts several days Pathology Superficial and deep lymphocytic infiltrate Marked papillary dermal edema PMLE Treatment Topical or oral corticosteroids High SPF Restriction of UV exposure Hardening – natural, NBUVB, PUVA Antimalarial PMLE updates Study suggests topical vitamin D analogue used prophylactically may provide therapeutic benefit in PMLE Gruber-Wackernagel A, Bambach FJ, Legat A, et al. Br J Dermatol, 2011. PMLE updates Study seeks to further elucidate the pathogenesis of PMLE Found a decrease in Langerhans cells and an increase in mast cell density in lesional skin Wolf P, Gruber-Wackernagel A, Bambach I, et al. Exp Dermatol, 2014. Actinic prurigo Similar to PMLE Common in native -

Patch Testing in Adverse Drug Reactions Has Not Always Been Appreciated, but There Is Growing a Interest in This Field
24_401_412 05.11.2005 10:37 Uhr Seite 401 Chapter 24 Patch Testing 24 in Adverse Drug Reactions Derk P.Bruynzeel, Margarida Gonçalo Contents Core Message 24.1 Introduction . 401 24.2 Pathomechanisms . 403 í A drug eruption is an adverse skin reaction 24.3 Patch Test Indications . 404 caused by a drug used in normal doses 24.4 Technique and Test Materials . 406 and presents a wide variety of cutaneous reactions. 24.5 Relevance and Consequences . 407 References . 408 24.1 Introduction A drug eruption is an adverse skin reaction caused by a drug used in normal doses. Systemic exposure to drugs can lead to a wide variety of cutaneous reac- tions, ranging from erythema, maculopapular erup- tions (the most frequent reaction pattern), acrovesic- ular dermatitis, localized fixed drug eruptions, to toxic epidermal necrolysis and from urticaria to anaphylaxis (Figs. 1, 2). The incidence of these erup- tions is not exactly known; 2%–5% of inpatients ex- perience such a reaction and it is a frequent cause of consultation in dermatology [1–3]. Topically applied drugs may cause contact dermatitis reactions. Topi- cal sensitization and subsequent systemic exposure may induce dermatological patterns similar to drug eruptions or patterns more typical of a systemic con- tact dermatitis, like the “baboon syndrome” (Chap. 16). It is clear that, in these situations, patch testing can be of great help as a diagnostic tool [4]. In patients with drug eruptions without previous contact sensitization, patch testing seems less logical, but is still a strong possibility, as systemic exposure of drugs may also lead to T-cell sensitization and to delayed type IV hypersensitivity reactions [5–8]. -

Fundamentals of Dermatology Describing Rashes and Lesions
Dermatology for the Non-Dermatologist May 30 – June 3, 2018 - 1 - Fundamentals of Dermatology Describing Rashes and Lesions History remains ESSENTIAL to establish diagnosis – duration, treatments, prior history of skin conditions, drug use, systemic illness, etc., etc. Historical characteristics of lesions and rashes are also key elements of the description. Painful vs. painless? Pruritic? Burning sensation? Key descriptive elements – 1- definition and morphology of the lesion, 2- location and the extent of the disease. DEFINITIONS: Atrophy: Thinning of the epidermis and/or dermis causing a shiny appearance or fine wrinkling and/or depression of the skin (common causes: steroids, sudden weight gain, “stretch marks”) Bulla: Circumscribed superficial collection of fluid below or within the epidermis > 5mm (if <5mm vesicle), may be formed by the coalescence of vesicles (blister) Burrow: A linear, “threadlike” elevation of the skin, typically a few millimeters long. (scabies) Comedo: A plugged sebaceous follicle, such as closed (whitehead) & open comedones (blackhead) in acne Crust: Dried residue of serum, blood or pus (scab) Cyst: A circumscribed, usually slightly compressible, round, walled lesion, below the epidermis, may be filled with fluid or semi-solid material (sebaceous cyst, cystic acne) Dermatitis: nonspecific term for inflammation of the skin (many possible causes); may be a specific condition, e.g. atopic dermatitis Eczema: a generic term for acute or chronic inflammatory conditions of the skin. Typically appears erythematous, -

Frontiers in Dermatology and Venereology - a Series of Theme Issues in Relation to the 100-Year Anniversary of Actadv
ISSN 0001-5555 ActaDV Volume 100 2020 Theme issue ADVANCES IN DERMATOLOGY AND VENEREOLOGY A Non-profit International Journal for Interdisciplinary Skin Research, Clinical and Experimental Dermatology and Sexually Transmitted Diseases Frontiers in Dermatology and Venereology - A series of theme issues in relation to the 100-year anniversary of ActaDV Official Journal of - European Society for Dermatology and Psychiatry Affiliated with - The International Forum for the Study of Itch Immediate Open Access Acta Dermato-Venereologica www.medicaljournals.se/adv ACTA DERMATO-VENEREOLOGICA The journal was founded in 1920 by Professor Johan Almkvist. Since 1969 ownership has been vested in the Society for Publication of Acta Dermato-Venereologica, a non-profit organization. Since 2006 the journal is published online, independently without a commercial publisher. (For further information please see the journal’s website https://www. medicaljournals.se/acta) ActaDV is a journal for clinical and experimental research in the field of dermatology and venereology and publishes high- quality papers in English dealing with new observations on basic dermatological and venereological research, as well as clinical investigations. Each volume also features a number of review articles in special areas, as well as Correspondence to the Editor to stimulate debate. New books are also reviewed. The journal has rapid publication times. Editor-in-Chief: Olle Larkö, MD, PhD, Gothenburg Former Editors: Johan Almkvist 1920–1935 Deputy Editors: Sven Hellerström 1935–1969 -

Dermatological Disorders in Tuvalu Between 2009 and 2012
MOLECULAR MEDICINE REPORTS 12: 3629-3631, 2015 Dermatological disorders in Tuvalu between 2009 and 2012 LI-JUNG LAN1,2, YING-SHUANG LIEN2,3, SHAO-CHUAN WANG2,4, NESE ITUASO-CONWAY5, MING-CHE TSAI2,6, PAO-YING TSENG6, YU-LIN YEH1, CHUN-TZU CHEN7, KO‑HUANG LUE2,8, JING-GUNG CHUNG9,10 and YU-PING HSIAO1,2 1Department of Dermatology, Chung Shan Medical University Hospital, Taichung 40201; 2Institute of Medicine, School of Medicine, Chung Shan Medical University, Taichung 40201; Departments of 3Obstetrics and Gynecology, and 4Urology, Chung Shan Medical University Hospital, Taichung 40201; 5Public Health, Princess Margaret Hospital, Ministry of Health, Funafuti, Tuvalu; 6International Medical Service Center, Chung Shan Medical University Hospital, Taichung 40201; Departments of 7Chief Secretary Group and 8Pediatrics, Chung Shan Medical University Hospital, Taichung 40201; 9Department of Biological Science and Technology, China Medical University, Taichung 40201; 10Department of Biotechnology, Asia University, Taichung 41354, Taiwan, R.O.C. Received July 1, 2014; Accepted September 18, 2014 DOI: 10.3892/mmr.2015.3806 Abstract. There is a distinct lack of knowledge on the land area of Tuvalu is only 25.9 km2, and the highest point does prevalence of skin disorders in Tuvalu. The aim of the current not exceed 4 m above sea level (1). Currently, an estimated study was to assess the prevalence of cutaneous diseases and 11,000 people live in Tuvalu (1). The Taiwan International to evaluate access dermatological care in Tuvalu. Cutaneous Cooperation and Development Fund (Taiwan ICDF) has disorders in the people of Tuvalu between 2009 and 2012 coordinated the medical resources of Taiwanese hospitals in were examined. -
Practical Dermatology Methodical Recommendations
Vitebsk State Medical University Practical Dermatology Methodical recommendations Adaskevich UP, Valles - Kazlouskaya VV, Katina MA VSMU Publishing 2006 616.5 удк-б-1^«адл»-2о -6Sl«Sr83p3»+4£*łp30 А28 Reviewers: professor Myadeletz OD, head of the department of histology, cytology and embryology in VSMU: professor Upatov Gl, head of the department of internal diseases in VSMU Adaskevich IIP, Valles-Kazlouskaya VV, Katina МЛ. A28 Practical dermatology: methodical recommendations / Adaskevich UP, Valles-Kazlouskaya VV, Katina MA. - Vitebsk: VSMU, 2006,- 135 p. Methodical recommendations “Practical dermatology” were designed for the international students and based on the typical program in dermatology. Recommendations include tests, clinical tasks and practical skills in dermatology that arc used as during practical classes as at the examination. УДК 616.5:37.022.=20 ББК 55.83p30+55.81 p30 C Adaskev ich UP, Valles-Ka/.louskaya VV, Katina MA. 2006 OVitebsk State Medical University. 2006 Content 1. Practical skills.......................................................................................................5 > 1.1. Observation of the patient's skin (scheme of the case history).........................5 1.2. The determination of skin moislness, greasiness, dryness and turgor.......... 12 1.3. Dermographism determination.........................................................................12 1.4. A method of the arrangement of dropping and compressive allergic skin tests and their interpretation........................................................................................................ -

“The Red Face” and More Clinical Pearls
“The Red Face” and More Clinical Pearls Courtney R. Schadt, MD, FAAD Assistant Professor Residency Program Director University of Louisville Associates in Dermatology I have no disclosures or conflicts of interest Part 1: The Red Face: Objectives • Distinguish and diagnose common eruptions of the face • Recognize those with potential implications for internal disease • Learn basic treatment options Which patient(s) has an increased risk of hypertension and hyperlipidemia? A B C Which patient(s) has an increased risk of hypertension and hyperlipidemia? A Seborrheic Dermatitis B C Psoriasis Seborrheic Dermatitis Goodheart HP. Goodheart's photoguide of common skin disorders, 2nd ed, Lippincott Williams & Wilkins, Philadelphia 2003. Copyright © 2003 Lippincott Williams & Wilkins. Seborrheic Dermatitis • Erythematous scaly eruption • Infants= “Cradle Cap” • Reappear in adolescence or later in life • Chronic, remissions and flares; worse with stress, cold weather • Occurs on areas of body with increased sebaceous glands • Unclear role of Malassezia; could be immune response; no evidence of overgrowth Seborrheic Dermatitis Severe Seb Derm: THINK: • HIV (can also be more diffuse on trunk) • Parkinson’s (seb derm improves with L-dopa therapy) • Other neurologic disorders • Neuroleptic agents • Unclear etiology 5MinuteClinicalConsult Clinical Exam • Erythema/fine scale • Scalp • Ears • Nasolabial folds • Beard/hair bearing areas Goodheart HP. Goodheart's photoguide of common skin disorders, 2nd ed, Lippincott • Ill-defined Williams & Wilkins, Philadelphia -

Therapies for Common Cutaneous Fungal Infections
MedicineToday 2014; 15(6): 35-47 PEER REVIEWED FEATURE 2 CPD POINTS Therapies for common cutaneous fungal infections KENG-EE THAI MB BS(Hons), BMedSci(Hons), FACD Key points A practical approach to the diagnosis and treatment of common fungal • Fungal infection should infections of the skin and hair is provided. Topical antifungal therapies always be in the differential are effective and usually used as first-line therapy, with oral antifungals diagnosis of any scaly rash. being saved for recalcitrant infections. Treatment should be for several • Topical antifungal agents are typically adequate treatment weeks at least. for simple tinea. • Oral antifungal therapy may inea and yeast infections are among the dermatophytoses (tinea) and yeast infections be required for extensive most common diagnoses found in general and their differential diagnoses and treatments disease, fungal folliculitis and practice and dermatology. Although are then discussed (Table). tinea involving the face, hair- antifungal therapies are effective in these bearing areas, palms and T infections, an accurate diagnosis is required to ANTIFUNGAL THERAPIES soles. avoid misuse of these or other topical agents. Topical antifungal preparations are the most • Tinea should be suspected if Furthermore, subsequent active prevention is commonly prescribed agents for dermatomy- there is unilateral hand just as important as the initial treatment of the coses, with systemic agents being used for dermatitis and rash on both fungal infection. complex, widespread tinea or when topical agents feet – ‘one hand and two feet’ This article provides a practical approach fail for tinea or yeast infections. The pharmacol- involvement. to antifungal therapy for common fungal infec- ogy of the systemic agents is discussed first here.