Pruritus: Scratching the Surface
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) Patent Application Publication (10) Pub. No.: US 2008/0317805 A1 Mckay Et Al
US 20080317805A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2008/0317805 A1 McKay et al. (43) Pub. Date: Dec. 25, 2008 (54) LOCALLY ADMINISTRATED LOW DOSES Publication Classification OF CORTICOSTEROIDS (51) Int. Cl. A6II 3/566 (2006.01) (76) Inventors: William F. McKay, Memphis, TN A6II 3/56 (2006.01) (US); John Myers Zanella, A6IR 9/00 (2006.01) Cordova, TN (US); Christopher M. A6IP 25/04 (2006.01) Hobot, Tonka Bay, MN (US) (52) U.S. Cl. .......... 424/422:514/169; 514/179; 514/180 (57) ABSTRACT Correspondence Address: This invention provides for using a locally delivered low dose Medtronic Spinal and Biologics of a corticosteroid to treat pain caused by any inflammatory Attn: Noreen Johnson - IP Legal Department disease including sciatica, herniated disc, Stenosis, mylopa 2600 Sofamor Danek Drive thy, low back pain, facet pain, osteoarthritis, rheumatoid Memphis, TN38132 (US) arthritis, osteolysis, tendonitis, carpal tunnel syndrome, or tarsal tunnel syndrome. More specifically, a locally delivered low dose of a corticosteroid can be released into the epidural (21) Appl. No.: 11/765,040 space, perineural space, or the foramenal space at or near the site of a patient's pain by a drug pump or a biodegradable drug (22) Filed: Jun. 19, 2007 depot. E Day 7 8 Day 14 El Day 21 3OO 2OO OO OO Control Dexamethasone DexamethasOne Dexamethasone Fuocinolone Fluocinolone Fuocinolone 2.0 ng/hr 1Ong/hr 50 ng/hr 0.0032ng/hr 0.016 ng/hr 0.08 ng/hr Patent Application Publication Dec. 25, 2008 Sheet 1 of 2 US 2008/0317805 A1 900 ----------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------- 80.0 - 7OO – 6OO - 5OO - E Day 7 EDay 14 40.0 - : El Day 21 2OO - OO = OO – Dexamethasone Dexamethasone Dexamethasone Fuocinolone Fluocinolone Fuocinolone 2.0 ng/hr 1Ong/hr 50 ng/hr O.OO32ng/hr O.016 ng/hr 0.08 nghr Patent Application Publication Dec. -

Obstetrics and Gynecology Pretest® Self-Assessment and Review 10412 Wylen Fm.£.Qxd 6/18/03 10:55 AM Page Ii
10412_Wylen_fm.£.qxd 6/18/03 10:55 AM Page i PRE ® TEST Obstetrics and Gynecology PreTest® Self-Assessment and Review 10412_Wylen_fm.£.qxd 6/18/03 10:55 AM Page ii Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the information contained herein with other sources. For example and in particular, readers are advised to check the prod- uct information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. 10412_Wylen_fm.£.qxd 6/18/03 10:55 AM Page iii PRE ® TEST Obstetrics and Gynecology PreTest® Self-Assessment and Review Tenth Edition Michele Wylen, M.D. -

3628-3641-Pruritus in Selected Dermatoses
Eur opean Rev iew for Med ical and Pharmacol ogical Sci ences 2016; 20: 3628-3641 Pruritus in selected dermatoses K. OLEK-HRAB 1, M. HRAB 2, J. SZYFTER-HARRIS 1, Z. ADAMSKI 1 1Department of Dermatology, University of Medical Sciences, Poznan, Poland 2Department of Urology, University of Medical Sciences, Poznan, Poland Abstract. – Pruritus is a natural defence mech - logical self-defence mechanism similar to other anism of the body and creates the scratch reflex skin sensations, such as touch, pain, vibration, as a defensive reaction to potentially dangerous cold or heat, enabling the protection of the skin environmental factors. Together with pain, pruritus from external factors. Pruritus is a frequent is a type of superficial sensory experience. Pruri - symptom associated with dermatoses and various tus is a symptom often experienced both in 1 healthy subjects and in those who have symptoms systemic diseases . Acute pruritus often develops of a disease. In dermatology, pruritus is a frequent simultaneously with urticarial symptoms or as an symptom associated with a number of dermatoses acute undesirable reaction to drugs. The treat - and is sometimes an auxiliary factor in the diag - ment of this form of pruritus is much easier. nostic process. Apart from histamine, the most The chronic pruritus that often develops in pa - popular pruritus mediators include tryptase, en - tients with cholestasis, kidney diseases or skin dothelins, substance P, bradykinin, prostaglandins diseases (e.g. atopic dermatitis) is often more dif - and acetylcholine. The group of atopic diseases is 2,3 characterized by the presence of very persistent ficult to treat . Persistent rubbing, scratching or pruritus. -

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

European Guideline Chronic Pruritus Final Version
EDF-Guidelines for Chronic Pruritus In cooperation with the European Academy of Dermatology and Venereology (EADV) and the Union Européenne des Médecins Spécialistes (UEMS) E Weisshaar1, JC Szepietowski2, U Darsow3, L Misery4, J Wallengren5, T Mettang6, U Gieler7, T Lotti8, J Lambert9, P Maisel10, M Streit11, M Greaves12, A Carmichael13, E Tschachler14, J Ring3, S Ständer15 University Hospital Heidelberg, Clinical Social Medicine, Environmental and Occupational Dermatology, Germany1, Department of Dermatology, Venereology and Allergology, Wroclaw Medical University, Poland2, Department of Dermatology and Allergy Biederstein, Technical University Munich, Germany3, Department of Dermatology, University Hospital Brest, France4, Department of Dermatology, Lund University, Sweden5, German Clinic for Diagnostics, Nephrology, Wiesbaden, Germany6, Department of Psychosomatic Dermatology, Clinic for Psychosomatic Medicine, University of Giessen, Germany7, Department of Dermatology, University of Florence, Italy8, Department of Dermatology, University of Antwerpen, Belgium9, Department of General Medicine, University Hospital Muenster, Germany10, Department of Dermatology, Kantonsspital Aarau, Switzerland11, Department of Dermatology, St. Thomas Hospital Lambeth, London, UK12, Department of Dermatology, James Cook University Hospital Middlesbrough, UK13, Department of Dermatology, Medical University Vienna, Austria14, Department of Dermatology, Competence Center for Pruritus, University Hospital Muenster, Germany15 Corresponding author: Elke Weisshaar -

Management of Cutaneous Hemangiomas in Pediatric Patients
PEDIATRIC DERMATOLOGY Series Editor: Camila K. Janniger, MD Management of Cutaneous Hemangiomas in Pediatric Patients Maria Letizia Musumeci, MD, PhD; Karina Schlecht, MD, PhD; Rosario Perrotta, MD; Robert A. Schwartz, MD, MPH; Giuseppe Micali, MD Cutaneous hemangiomas (CHs) are common benign during the first year of life and slow involution that vascular tumors of childhood. Clinically, they are usually is completed by 5 to 10 years of age.1 For characterized by a typical evolution profile, consist- this reason, no treatment is necessary in most cases. ing of a rapid proliferation during the first year of However, when CHs are located in areas at risk for life and slow involution that usually is completed functional complications; are of considerable size; or by 5 to 10 years of age. In most cases, no treat- repeatedly undergo bleeding, ulceration, or superin- ment is necessary. However, when CHs are located fection, a prompt and adequate treatment approach in areas at risk for functional complications; are of is required.2 considerable size; or repeatedly undergo bleeding, ulceration, or superinfection, a prompt and adequate Epidemiology treatment approach is required. First-line approaches CHs are present in 1.0% to 2.6% of neonates and in include topical, intralesional, and systemic corti- 10% to 12% of infants by 12 months of age.3 Thirty costeroids. Second-line options include interferon percent of CHs are first evident at birth; the remain- alfa-2a and -2b, laser therapy, and surgical therapy. der appear during the second month of life. The Third-line approaches include cytotoxins, emboliza- frequency of these benign tumors increases in pre- tion, and angiogenesis inhibitors. -

Skin Eruptions Specific to Pregnancy: an Overview
DOI: 10.1111/tog.12051 Review The Obstetrician & Gynaecologist http://onlinetog.org Skin eruptions specific to pregnancy: an overview a, b Ajaya Maharajan MBBS DGO MRCOG, * Christina Aye BMBCh MA Hons MRCOG, c d Ravi Ratnavel DM(Oxon) FRCP(UK), Ekaterina Burova FRCP CMSc (equ. PhD) aConsultant in Obstetrics and Gynaecology, Luton and Dunstable University Hospital, Lewsey Road, Luton, Bedfordshire LU4 0DZ, UK bST5 in Obstetrics and Gynaecology, John Radcliffe Hospital, Headley Way, Headington, Oxford OX3 9DU, UK cConsultant Dermatologist, Buckinghamshire Health Care, Mandeville Road, Aylesbury, Buckinghamshire HP21 8AL, UK dConsultant Dermatologist, Skin Cancer Lead for Bedford Hospital, Bedford Hospital NHS Trust, South Wing, Kempston Road, Bedford MK42 9DJ, UK *Correspondence: Ajaya Maharajan. Email: [email protected] Accepted on 31 January 2013 Key content Learning objectives Pregnancy results in various physiological skin changes. To understand the physiological skin changes in pregnancy. As a consequence, some common dermatoses can present more To identify the skin conditions that require appropriate referral. frequently in pregnant women. In addition, there are a number To be able to take a history, to diagnose the skin eruptions unique to of skin eruptions unique to pregnancy. pregnancy, undertake appropriate investigations and first-line The aetiology of physiological skin changes in pregnancy is management, and understand the criteria for referral to a uncertain but is thought to be due to hormonal and physical dermatologist. changes of pregnancy. Keywords: atopic eruption of pregnancy / intrahepatic cholestasis The four dermatoses of pregnancy are: atopic eruption of pregnancy / pemphigoid gestastionis / polymorphic eruption of of pregnancy, pemphigoid gestationis, polymorphic pregnancy / skin eruptions eruption of pregnancy and intrahepatic cholestasis of pregnancy. -

Update of the Guideline on Chronic Pruritus
Update of the Guideline on Chronic Pruritus Developed by the Guideline Subcommittee “Chronic Pruritus” of the European Dermatology Forum Subcommittee Members: Prof. Dr. Elke Weisshaar, Heidelberg (Germany) Prof. Dr. Sonja Ständer, Münster (Germany) Prof. Dr. Erwin Tschachler, Wien (Austria) Prof. Dr. Torello Lotti, Florence (Italy) Prof. Dr. Johannes Ring, Munich (Germany) Prof. Dr. Laurent Misery, Brest (France) Dr. Markus Streit, Aarau (Switzerland) Prof. Dr. Thomas Mettang, Wiesbaden (Germany) Prof. Dr. Jacek Szepietowski, Wroclaw (Poland) Prof. Dr. Joanna Wallengren, Lund (Sweden) Dr. Peter Maisel, Münster (Germany) Prof. Dr. Uwe Gieler, Gießen (Germany) Prof. Dr. Malcolm Greaves (Singapore) Prof. Dr. Ulf Darsow, Munich (Germany) Prof. Dr. Julien Lambert, Antwerp (Belgium) Members of EDF Guideline Committee: Prof. Dr. Werner Aberer, Graz (Austria) Prof. Dr. Dieter Metze, Münster (Germany) Prof. Dr. Martine Bagot, Paris (France) Dr. Kai Munte, Rotterdam (Netherlands) Prof. Dr. Nicole Basset-Seguin, Paris (France) Prof. Dr. Gilian Murphy, Dublin (Ireland) Prof. Dr. Ulrike Blume-Peytavi, Berlin (Germany) Prof. Dr. Martino Neumann, Rotterdam (Netherlands) Prof. Dr. Lasse Braathen, Bern (Switzerland) Prof. Dr. Tony Ormerod, Aberdeen (UK) Prof. Dr. Sergio Chimenti, Rome (Italy) Prof. Dr. Mauro Picardo, Rome (Italy) Prof. Dr. Alexander Enk, Heidelberg (Germany) Prof. Dr. Johannes Ring, Munich (Germany) Prof. Dr. Claudio Feliciani, Rome (Italy) Prof. Dr. Annamari Ranki, Helsinki (Finland) Prof. Dr. Claus Garbe, Tübingen (Germany) Prof. Dr. Berthold Rzany, Berlin (Germany) Prof. Dr. Harald Gollnick, Magdeburg (Germany) Prof. Dr. Rudolf Stadler, Minden (Germany) Prof. Dr. Gerd Gross, Rostock (Germany) Prof. Dr. Sonja Ständer, Münster (Germany) Prof. Dr. Vladimir Hegyi, Bratislava (Slovakia) Prof. Dr. Eggert Stockfleth, Berlin (Germany) Prof. Dr. -
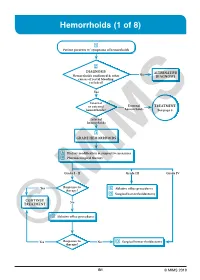
Hemorrhoids (1 of 8)
Hemorrhoids (1 of 8) 1 Patient presents w/ symptoms of hemorrhoids 2 DIAGNOSIS No ALTERNATIVE Hemorrhoids confi rmed & other DIAGNOSIS causes of rectal bleeding excluded? Yes Internal or external External TREATMENT hemorrhoids? hemorrhoids See page 3 Internal hemorrhoids 3 GRADE HEMORRHOIDS A Dietary modifi cation & supportive measures B Pharmacological therapy Grade I - II Grade III Grade IV Yes Response to C Ablative offi ce procedures therapy? D Surgical hemorrhoidectomy CONTINUE No TREATMENT C Ablative offi ce procedures Yes Response to No D Surgical hemorrhoidectomy ©therapy? MIMS B1 © MIMS 2019 Hemorrhoids (2 of 8) 1 SYMPTOMS ATTRIBUTED TO HEMORRHOIDS • Rectal bleeding - Most common presenting symptom - Bright red blood which may drip or squirt into the toilet bowl or scanty amounts may be seen on toilet tissue • Discomfort due to rectal protrusion or lump • Anal pain • HEMORRHOIDS Anal itching 2 DIAGNOSIS Medical History • Assess nature, duration & severity of symptoms - Ask about bleeding, its amount & frequency - Ask about presence of prolapsing tissue, its timing & reproducibility • Elicit possible risk factors for development of hemorrhoidal symptoms - Low-fi ber diets cause small-caliber stools, resulting in straining during defecation & engorgement of hemorrhoids - Prolonged sitting on a toilet which may cause a problem in the venous return in the perianal area - Pregnancy - Advanced age • Th e signs & symptoms of hemorrhoids are not specifi c to the disease, so care must be taken to avoid missing other causes of pathology • Obtain -

Treatment Options for Atopic Dermatitis LUCINDA M
Treatment Options for Atopic Dermatitis LUCINDA M. BUYS, PHARM.D., B.C.P.S., Siouxland Medical Education Foundation, Sioux City, Iowa Atopic dermatitis is a common inflammatory skin condition that usually affects children. It is a chronic disease, with periods of remission and flare-ups, that adversely affects the quality of life of patients and their families. Aggressive therapy with emollients is an important intervention for patients with atopic dermatitis. Patients should avoid individual disease triggers and aller- gens. Topical corticosteroids are the mainstay of treatment for flare-ups and are the standard to which other treatments are compared. Topical calcineurin inhibitors should not be used in patients younger than two years or in those who are immunosuppressed, and should be second- line therapies in other patients. Rarely, systemic agents (e.g., cyclosporine, interferon gamma-1b, oral corticosteroids) may be considered in adults. (Am Fam Physician 2007;75:523-8, 530. Copy- right © 2007 American Academy of Family Physicians.) T Patient information: A handout on atopic topic dermatitis is the most com- T-helper type 2 cells, leading to increased dermatitis, written by the mon childhood skin disorder in interleukin-4 production, which promotes author of this article, is developed countries.1 The prev- IgE production. provided on page 530. alence of atopic dermatitis has Atopic dermatitis can have a significant Aincreased two- to threefold in the last three impact on morbidity and quality of life. Chil- decades, affecting 15 to 20 percent of young dren may be affected by itching and associ- children.2 Clinical findings of atopic derma- ated sleep disturbance, the social stigma of titis are variable but can be categorized into a visible skin condition, and the need for three groups of diagnostic features: essential, frequent application of topical medications important, and associated (Table 1).3 Atopic and physician visits. -

Effect of Intra-Articular Triamcinolone Vs Saline on Knee
Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021 Downloaded From: https://jamanetwork.com/ on 09/28/2021