Our Annual Engagement Review for 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mira Technology Park
MIRA TECHNOLOGY PARK Transport Assessment April 2011 MIRA TECHNOLOGY PARK Transport Assessment April 2011 ATC Ref: 10/014‐A Produced by Advance Transportation Consulting Sandy Farm Business Centre The Sands Farnham Surrey GU10 1PX Tel: 01252 782237 Email: [email protected] MIRA Technology Park Transport Assessment CONTENTS 1. INTRODUCTION & SCOPE OF DOCUMENT ................................................................................... 1 Overview ............................................................................................................................................. 1 Transportation Assessment Structure ................................................................................................ 3 2. POLICY CONTEXT ........................................................................................................................ 6 National Planning Policy ..................................................................................................................... 6 Local Plan/Local Development Framework ........................................................................................ 9 Local Transport Plan (LTP 3) .............................................................................................................. 11 3. SITE DESCRIPTION AND EXISTING TRAFFIC AND TRANSPORT CONDITIONS ................................ 14 Development Site Location and Description .................................................................................... 14 MIRA Development Site Access and -

Bibliography19802017v2.Pdf
A LIST OF PUBLICATIONS ON THE HISTORY OF WARWICKSHIRE, PUBLISHED 1980–2017 An amalgamation of annual bibliographies compiled by R.J. Chamberlaine-Brothers and published in Warwickshire History since 1980, with additions from readers. Please send details of any corrections or omissions to [email protected] The earlier material in this list was compiled from the holdings of the Warwickshire County Record Office (WCRO). Warwickshire Library and Information Service (WLIS) have supplied us with information about additions to their Local Studies material from 2013. We are very grateful to WLIS for their help, especially Ms. L. Essex and her colleagues. Please visit the WLIS local studies web pages for more detailed information about the variety of sources held: www.warwickshire.gov.uk/localstudies A separate page at the end of this list gives the history of the Library collection, parts of which are over 100 years old. Copies of most of these published works are available at WCRO or through the WLIS. The Shakespeare Birthplace Trust also holds a substantial local history library searchable at http://collections.shakespeare.org.uk/. The unpublished typescripts listed below are available at WCRO. A ABBOTT, Dorothea: Librarian in the Land Army. Privately published by the author, 1984. 70pp. Illus. ABBOTT, John: Exploring Stratford-upon-Avon: Historical Strolls Around the Town. Sigma Leisure, 1997. ACKROYD, Michael J.M.: A Guide and History of the Church of Saint Editha, Amington. Privately published by the author, 2007. 91pp. Illus. ADAMS, A.F.: see RYLATT, M., and A.F. Adams: A Harvest of History. The Life and Work of J.B. -

48A Bus Time Schedule & Line Route
48A bus time schedule & line map 48A Atherstone View In Website Mode The 48A bus line (Atherstone) has 2 routes. For regular weekdays, their operation hours are: (1) Atherstone: 6:28 AM - 9:24 PM (2) Nuneaton: 6:56 AM - 9:47 PM Use the Moovit App to ƒnd the closest 48A bus station near you and ƒnd out when is the next 48A bus arriving. Direction: Atherstone 48A bus Time Schedule 32 stops Atherstone Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 6:28 AM - 9:24 PM Bus Station, Nuneaton Hareƒeld Road, Nuneaton Tuesday 6:28 AM - 9:24 PM Fire Station, Nuneaton Wednesday 6:28 AM - 9:24 PM Newtown Road, Nuneaton Thursday 6:28 AM - 9:24 PM Manor Court Road, Nuneaton Friday 6:28 AM - 9:24 PM Stanley Road, Nuneaton Saturday 6:36 AM - 9:24 PM Charles Street, Nuneaton Arrow Road, Nuneaton Queen Elizabeth Road, Nuneaton 48A bus Info Direction: Atherstone Holly Stitches Road, Nuneaton Stops: 32 Trip Duration: 25 min Walnut Close, Nuneaton Line Summary: Bus Station, Nuneaton, Fire Station, Nuneaton, Manor Court Road, Nuneaton, Stanley Tuttle Hill, Nuneaton Road, Nuneaton, Arrow Road, Nuneaton, Queen Camp Hill Road, Nuneaton Elizabeth Road, Nuneaton, Holly Stitches Road, Nuneaton, Walnut Close, Nuneaton, Tuttle Hill, Arlon Avenue, Nuneaton Nuneaton, Arlon Avenue, Nuneaton, Craddock Drive, Nuneaton, St Annes Rc Church, Nuneaton, Victoria Craddock Drive, Nuneaton Road, Nuneaton, School Hill, Hartshill, Post O∆ce, Hartshill, Michael Drayton Junior School, Hartshill, St Annes Rc Church, Nuneaton Oldbury View, Hartshill, Green, Hartshill, -

Nuneaton Town Centre
DESIGN PRINCIPLES FOR NUNEATON TOWN CENTRE BASED ON VICARAGE STREET SITE DEVELOPMENT Leicester 30 mins Warwickshire Boulevard treatment St Nicolas Parish Church Justice Centre to Vicarage Street Birmingham 30 mins Possible hotel sites Housing overlooking 7 the park London 60 mins Coventry 7 15 mins 3 t e e r t S h c ur 1 Ch Realigned Wheat Street 6 with street trees running 3 George Eliot down to the riverfront Gardens NUNEATON 5 2 1 4 6 The town centre opportunity Church Street and Bond Gate you have been waiting for reinforced as a new North/ 6 South spine between church 6 and railway station 2 4 OUR PARTNERSHIP 5 OFFER 6 5 What we will do to What we’re looking for 2 transform Nuneaton: in potential partners: • Work proactively with • Your ideas on generating Reconfigured offices as partners to develop our value in the town centre apartments overlooking town centre assets 5 river and park • Creative approaches to • Use our land to leverage in land use mix, delivery, further investment finance and management • Work to ensure emerging policy supports delivery River Anker waterfront opened up Bridge physically and New residential units over Boardwalk squares with • Retain a long term interest to form a new mixed use, leisure visually opened up to the town centre shopping cafes, restaurants and to sustain the value in the and residential offer riverfront wine bars site • Manage development directly where appropriate VICARAGE STREET 4. Creating new, and reinforcing existing, pedestrian 1. Introducing a new high quality mixed use and cycle-friendly routes through the town centre development in the heart of the town centre OPPORTUNITY 5. -

Summer 2017 Issue 2
Summer 2017 Issue 2 Escape 20th Birthday Celebrations July marked a very special time for the charity. Escape originated from two voluntary organisations which were both founded in 1997 by Artistic Directors Robin Wade and Karen Williams. Robin established the Escape project in her front room, supporting adults through weekly ceramic workshops and Karen Williams established Community Art in Action: creative workshops supporting adults with learning disabilities. Both of these groups still flourish today,Stratford Escape every Wednesday and Paper Moon every Tuesday. The 20th Birthday celebration resulted in a three day exhibition involving Escape work from across all the project venues and activities. It was attended by over 2000 people and was a great opportunity to bring the Escape family of staff, volunteers and participants all together. Leading up to the celebrations, Escape ran a competition to ‘Name The Steer’ the fantastic sculpture created by Rachel Higgins which now resides outside the Slaughterhouse. The winning entry was ‘Metallic Moo’ won by Oliver Hughes from The Willows Primary School. Robin Wade Retirement At this time we say a fond farewell to Robin, who after 20 years of passion and dedication is now retiring. Robin speaks fondly about Escape: “Many changes have taken place for Escape over the past twenty years and so many creative talents have been realised. From small beginnings Escape has grown through the decades and we have all had an extraordinary journey. Timing has been everything; receiving funding through Big Lottery, the Town Trust Challenge and the Arts Council gave us the opportunity to build on all our previous work within the community and allow as many people as possible to share in what we do. -

Industrial/ Open Storage Land 2 Acres (8,100 Sq.M) to LET Haunchwood Park, Bermuda Road, Nuneaton, CV10 7QG
Industrial/ Open Storage Land 2 Acres (8,100 sq.m) TO LET Haunchwood Park, Bermuda Road, Nuneaton, CV10 7QG PROPERTY HIGHLIGHTS • 2 acres storage to let • Secure palisade fence • Sub divisible from 1 acre • Close to motorway network • Flexible lease options available • Design and build option may be available LOCATION BERMUDA CONNECTION Nuneaton oers a strategic location for distribution Bermuda Connection is a proposed scheme focused occupiers in the West Midlands being conveniently on tackling congestion in and around West Nuneaton located some four miles North of the M6 motorway. The by creating a direct 1.3mile highway link between West M6 can be accessed by the A444 at Junction 3 of the Nuneaton and Griff Roundabout.More details available M6. Alternatively, the M69 motorway at Hinckley can be at www.warwickshire.gov.uk/bermudaconnection. accessed at Junction 1 for access to the motorway At the time of publication of these particulars a final network in a northerly direction. decision has yet to be taken regarding the implementation of the Bermuda Connection scheme DESCRIPTION This 2 acre site consist of cleared open storage land with a concrete base to part and a secure palisade fence. B U L L HEATH END ROAD R IN RENT G B E R M £60,000 per annum U D A R GEORGE ELIOT O HOSPITAL A SERVICES D A444 All mains services connected. TENURE The site is available on a new lease on flexible terms as whole or from 1 acre. Alternatively design and build proposals available on request. A444 M42 A444 A38 J8 A5 Nuneaton M6 BIRMINGHAM M69 M1 J7 Bedworth M6 A5 J6 A45 J2 A34 A41 M6 Solihull COVENTRY A435 J19 A452 A45 Rugby M1 M42 A46 A45 J3a A445 M45 M40 J17 A429 Redditch A423 Leamington Spa A45 A435 Warwick Daventry J15 VAT ROAD LINKS Bromwich Hardy stipulate that prices are quoted M6 Junction 3 5.1 miles exclusive of V.A.T. -

Revised Plan May 2017 White
www.warwickshirewildlifetrust.org.uk ACTION for WILDLIFE Warwickshire, Coventry and Solihull Local Biodiversity Action Plan REVISED PLAN MAY 2017 WHITE-CLAWED CRAYFISH Austropotamobius pallipes 1. INTRODUCTION The white-clawed crayfish (also known as the Atlantic stream crayfish) is the only native species of freshwater crayfish in the UK. It lives in a variety of aquatic habitats that include streams, rivers, lakes, canals, reservoirs and water-filled quarries, preferring those without too much sediment and minimal pollution. Good refuges and cover, e.g. rocks, stones, aquatic vegetation, tree roots and bank cavities are important for its survival and lifecycle. © Tracey Doherty It is generally nocturnal, feeding on a range of vegetation, animal matter and detritus. Young crayfish are predated on by fish; larger crayfish are taken by birds, especially Grey Heron (Ardea cinerea), as well as mammals such as rat (Rattus norvegicus), mink (Neovison vison) and otter (Lutra lutra). The young can also fall prey to predatory insects such as dragonfly nymphs and diving beetle larvae. Maturation takes 3-4 years, with adults rarely exceeding 10cm in body length. For identification purposes, it is worth noting that at least six further species of crayfish have been introduced into Britain, with the American signal crayfish (Pacifastacus leniusculus) now accounting for an increasingly high proportion of crayfish records in the sub-region. Other non-native species include the noble (Astacus astacus), red swamp (Procambarus clarkii), spiny-cheeked (Orconectes limosus), virile (Orconectes virilis), and Turkish narrow-clawed crayfish (Astacus leptodactylus), some of which are recorded within the Severn and Humber River Basins. The introduction and spread of these non-native species has impacted the survival of white clawed crayfish, which is out-competed for food and habitat by these more aggressive species. -

Warwickshire Guide Adult Care and Support Services 2018/19
Warwickshire Guide Adult Care and Support Services 2018/19 The essential guide to choosing and paying for care and support Home support | Specialist care | Useful contacts | Care homes In association with www.carechoices.co.uk Why make a WCS care home Every day well lived your new home? Personal, high quality care Dedicated and friendly staff Homely feel with a family atmosphere Appetising home-cooked meals Daily activities led by enthusiastic Lifestyle Coaches No hidden charges Life doesn’t end when you move to a care home, in fact for some people who’ve been living on their own, it’s the start of a brand new adventure, and we’re thrilled to be a part of it. We have 10 homes in Warwickshire for older people and people with dementia, and two homes for people with physical disabilities and long-term conditions. And for relatives we have a relatives’ gateway, offering online access 24/7 to care notes and photos of loved ones, providing reassurance and contact whether they can visit in person or not. Find out more about us and our homes New home Visit www.wcs-care.co.uk opening in Warwick in @WCS_Care Email [email protected] facebook.com/wcscare Call 01926 864 242 2019! Registered charity number 1012788 Contents Welcome from Warwickshire County Council 4 Choices if you need accommodation with support 22 Areas covered by this guide 5 Extra care housing 22 Supported living for people with disabilities 22 Support for carers 5 Care homes 23 Young carers 5 Residential care home checklist 24 Getting out and staying active 6 Finding care in your -
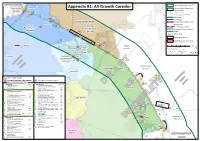
Appendix B1: A5 Growth Corridor
5km Distance buffer from A5 STAFFORDSHIREA 1 5 1 Polesworth Tamworth Appendix B1: A5 Growth Corridor Areas of Recent Major Road Improvements: Borough 2 A A5 / A444 / A47 - MIRA 4 2 47 A B M1 / M6 / A14 - Catthorpe Interchange (to be completed Autumn 2016) 69 3 4 M 5 4 4 4,5 A Motorways Trunk Roads 3 7 8 ! 42 Current Railway Stations and M LEICESTERSHIRE Atherstone Earl Shilton Railway Lines North 6 7 Hinckley 69 ! Warwickshire 6 A5 M Future Railway Stations and Bosworth HS2 Route (Phases 1 and 2) Borough A47 Borough Canals 21 25 Urban Areas A M 1 County Boundaries 8 A 22 Hinckley 11 District/Borough Boundaries 25 (Coloured administrative areas show "LEP City Deal" areas.) 13,14,15,16 23 10 9 A47 0 1 2 3 4 5 1:55,000 9 24 (When printed at 10 12 Blaby A1 paper size.) SOLIHULL 11 Kilometres Nuneaton District This map is for illustrative purposes only. ´ 12 © Crown Copyright and database right 2015. Ordnance Survey 100019520. 4 Produced by the WCC Corporate 4 4 GIS Team, A 13 69 25 June, 2015. M 15 14 Coleshill Nuneaton 16 and Bedworth A 1 17 5 M Borough Harborough WARWICKSHIRE District Bedworth 26 M6 28 D Current Employment Sites 29 D Future Employment Sites / Major Expansion 8 Future Major Housing Developments Lutterworth Red text signifies those sites without full planning permission 9 6 M Future Employment Staffordshire: Figures: Warwickshire: Housing Units: 27 Tamworth Borough: = Development Site North Warwickshire Borough: Rugby A45 * in Warwickshire 1 Relay Park - 1 Land on South Side of Grendon Road 143 2 Centurion Park 421 * 2 Orchard, Dordon 360 Borough 3 Dairy House Farm, Spon Lane 85 Warwickshire: 4 Land at Old Holly Lane including Durno's 620 A 4 North Warwickshire Borough: Nurseries 4 3 Kingsbury Link - 5 Rowland Way 88 4 4 Hall End Farm 750 6 Britannia Works, Coleshill Road 54 5 Birch Coppice (Phases 1-3) (inc. -

Kings Orchard Day Hire Insert
SpRiNgWoOd HaVeN 2022 Holiday Information ABC BOAT HIRE DIRECTIONS Snarestone BY ROAD From South A5 • Leave the M6 at J3 and turn right at the roundabout onto the A444. • Con�nue, passing over one roundabout and take the 2nd exit at the next roundabout to remain on the A444. • Con�nue, taking the 2nd exit at the next roundabout. B4111 • At the next roundabout take the 1st exit onto College Street. • At the roundabout take the 2nd exit onto Greenmoor Road. • Turn right onto Cro� Road. • At the roundabout con�nue straight to Manor Ct Road. • Turn le� onto Midland Road (B4144). A444 • A�er crossing over the Coventry canal, take the next right turn, B4111 then take the first exit (le�) at the roundabout. • Follow the road to the end, turn right, and then take the next 2 le� turns. BY ROAD From North (A444 & A5) • Leave the A444 turning onto Old Forge Road. • Turn right onto Drayton Lane. • Turn le� onto Watling Street (A5). • Exit the A5 onto Woodford Lane. Coventry • Turn le� onto Nuneaton Road (B4111). • Con�nue for 1.4 miles. • Next le� a�er the Windmill Sports & Social Club. • Take the next 2 le� turns. FROM AIRPORTS TRAVEL & PLANNING The closest airport to the marina is Birmingham Interna�onal Airport which is a 30 minute drive away LOCAL ACCOMMODATION (approximately 19 miles). Please check www.airbnb.co.uk or www.laterooms.com From London Airports: Make your way via the London for local availability. Underground, bus or taxi to London Euston train sta�on. From there take a train to Nuneaton which is 2 LOCAL TAXI COMPANIES miles from the marina. -

Guide to Adult and Community Learning in Nuneaton, Bedworth and North Warwickshire AUTUMN 2019
Adult and Community Learning Service Guide to Adult and Community Learning in Nuneaton, Bedworth and North Warwickshire AUTUMN 2019 Enrolments take place at the following times: Classes in Nuneaton: enrol at Camp Hill Early Years Centre, CV10 9QA English and ESOL daytime classes - Tuesday 3rd September, 9.30am - 4.00pm All evening classes - Tuesday 3rd September, 6.00 - 8.00pm All other daytime classes - Wednesday 4th September, 9.30am - 4.00pm Classes in Atherstone: enrol at Ratcliffe Centre, CV9 1LF Thursday 12th September, 9.30am - 2.00pm Classes in Bedworth: enrol at Bedworth Civic Hall, CV12 8NF Wednesday 11th September, 9.30am - 2.00pm For full details of enrolment and what to bring, see the back page. www.warwickshire.gov.uk/adultlearning European Union European Social Fund Investing in jobs and skills Course Information For more detailed information on any of our courses, please visit www.warwickshire.gov.uk/adultlearning email [email protected] or call us on 024 7635 3065. Cost Start Course Venue Day Time Weeks A B C Date English, Maths, ESOL (English for Speakers of Other Languages) courses Daytime classes take place at Camp Hill, Hatters Space and Stockingford: These courses take place across a range of days and times during the week. If you wish to join a course, please come to an enrolment/assessment session and we will agree an appropriate class for you to join. English* Camp Hill Early Years Centre FREE (exam fees may apply Maths* Hatters Space for ESOL courses) ESOL* Stockingford Early Years Centre Evening classes -

K. Test List of Streets Aug 2017
NUNEATON AND BEDWORTH BOROUGH COUNCIL ROAD KNOWLEDGE TEST The test will consist of four questions asking you to describe the shortest route between two given points which will be taken from this alphabetical list. Acorn Pub, Nuneaton George Eliot Hospital Ambleside Way, Nuneaton Gipsy Lane, Nuneaton Ambleside Road, Bedworth Golf Drive, Nuneaton Ansley Road, Nuneaton Goodyers End Lane, Bedworth Arbury Road, Nuneaton Greenmoor Road, Nuneaton ASDA, Nuneaton Haunchwood Road, Nuneaton Attleborough Road, Nuneaton Hayes Lane, Exhall Avenue Road, Nuneaton Heath End Road, Nuneaton Beefeater Griff House, Nuneaton Heath Road, Bedworth Bedworth Lane, Bedworth Hickman Road, Nuneaton Bedworth Leisure Centre Higham Lane, Nuneaton Bedworth Railway Station Hilary Road, Nuneaton Bermuda Road, Nuneaton Hinckley Road, Nuneaton Blackatree Road, Nuneaton Holiday Inn Express, Nuneaton Blackhorse Road, Exhall Horiba Mira, Nuneaton Bond Gate, Nuneaton Hospital Lane, Bedworth Bowling Green Lane, Exhall Jubilee Sports Centre, Nuneaton Bracebridge Street, Nuneaton Justice Centre, Nuneaton Bucks Hill, Nuneaton King Edward VI College. Nuneaton Bulkington Lane, Nuneaton Kingswood Road, Nuneaton Bulkington Road, Bedworth Kingsbridge Road, Nuneaton Cambourne Drive, Nuneaton Leicester Road, Bedworth Camp Hill Road, Nuneaton Long Shoot Hotel, Chase Hotel, Nuneaton Longford Road, Exhall Cedar Road, Nuneaton Lutterworth Road, Nuneaton Chesterton Drive, Nuneaton Manor Court Road, Nuneaton Chetwynd Drive, Nuneaton Marston Lane, Bedworth Civic Hall, Bedworth Marston Lane, Nuneaton,