Renal Autotransplantation– Past, Present and Future
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urology Services in the ASC
Urology Services in the ASC Brad D. Lerner, MD, FACS, CASC Medical Director Summit ASC President of Chesapeake Urology Associates Chief of Urology Union Memorial Hospital Urologic Consultant NFL Baltimore Ravens Learning Objectives: Describe the numerous basic and advanced urology cases/lines of service that can be provided in an ASC setting Discuss various opportunities regarding clinical, operational and financial aspects of urology lines of service in an ASC setting Why Offer Urology Services in Your ASC? Majority of urologic surgical services are already outpatient Many urologic procedures are high volume, short duration and low cost Increasing emphasis on movement of site of service for surgical cases from hospitals and insurance carriers to ASCs There are still some case types where patients are traditionally admitted or placed in extended recovery status that can be converted to strictly outpatient status and would be suitable for an ASC Potential core of fee-for-service case types (microsurgery, aesthetics, prosthetics, etc.) Increasing Population of Those Aged 65 and Over As of 2018, it was estimated that there were 51 million persons aged 65 and over (15.63% of total population) By 2030, it is expected that there will be 72.1 million persons aged 65 and over National ASC Statistics - 2017 Urology cases represented 6% of total case mix for ASCs Urology cases were 4th in median net revenue per case (approximately $2,400) – behind Orthopedics, ENT and Podiatry Urology comprised 3% of single specialty ASCs (5th behind -

History of Lung Transplantation Akciğer Transplantasyonu Tarihçesi
REVIEW History of Lung Transplantation Akciğer Transplantasyonu Tarihçesi Gül Dabak Unit of Pulmonology, Kartal Kosuyolu Yüksek Ihtisas Teaching Hospital for Cardiovascular Diseases and Surgery, İstanbul ABSTRACT ÖZET History of lung transplantation in the world dates back to the early 20 Dünyada akciğer transplantasyonu tarihçesi, deneysel çalışmala- th century, continues to the first clinical transplantation performed rın yapılmaya başlandığı 20. yüzyılın ilk yıllarından itibaren Ja- by James Hardy in the United States of America in 1963 and comes mes Hardy’ nin Amerika Birleşik Devletleri’nde 1963’te yaptığı to the present with increased frequency. Over 40.000 heart-lung ilk klinik transplantasyona uzanır ve hızlanarak günümüze gelir. and lung transplantations were carried out in the world up to 2011 yılına kadar dünyada 40,000’in üzerinde kalp-akciğer ve 2011. The number of transplant centers and patients is flourishing akciğer transplantasyonu yapılmıştır. Transplantasyon alanındaki in accordance with the increasing demand and success rate in that artan ihtiyaca ve başarılara paralel olarak transplant merkezleri arena. Lung transplantations that started in Turkey at Sureyyapasa ve hasta sayıları da giderek artmaktadır. Türkiye’de 2009 yılında Teaching Hospital for Pulmonary Diseases and Thoracic Surgery Süreyyapaşa Göğüs Hastalıkları ve Cerrahisi Eğitim ve Araştırma in 2009 are being performed at two centers actively to date. This Hastanesi’ nde başlayan akciğer transplantasyonları günümüzde review covers a general outlook on lung transplantations both in iki merkezde aktif olarak yapılmaktadır. Bu derlemede, ülkemiz- the world and in Turkey with details of the first successful lung deki ilk başarılı akciğer transplantasyonu detaylandırılarak dün- transplantation in our country. yada ve ülkemizdeki akciğer transplantasyonu tarihçesi gözden Keywords: Lung transplantation, heart-lung transplantation, his- geçirilmektedir. -
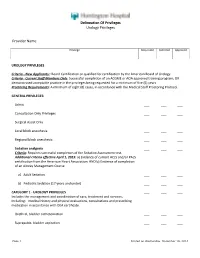
Delineation of Privileges Urology Privileges Provider Name
Delineation Of Privileges Urology Privileges Provider Name: Privilege Requested Deferred Approved UROLOGY PRIVILEGES Criteria - New Applicants:: Board Certification or qualified for certification by the American Board of Urology. Criteria - Current Staff Members Only: Successful completion of an ACGME or AOA approved training program; OR demonstrated acceptable practice in the privileges being requested for a minimum of five (5) years. Proctoring Requirements: A minimum of eight (8) cases, in accordance with the Medical Staff Proctoring Protocol. GENERAL PRIVILEGES: Admit ___ ___ ___ Consultation Only Privileges ___ ___ ___ Surgical Assist Only ___ ___ ___ Local block anesthesia ___ ___ ___ Regional block anesthesia ___ ___ ___ Sedation analgesia ___ ___ ___ Criteria: Requires successful completion of the Sedation Assessment test. Additional criteria effective April 1, 2015: a) Evidence of current ACLS and/or PALS certification from the American Heart Association; AND b) Evidence of completion of an Airway Management Course a) Adult Sedation ___ ___ ___ b) Pediatric Sedation (17 years and under) ___ ___ ___ CATEGORY 1 - UROLOGY PRIVILEGES ___ ___ ___ Includes the management and coordination of care, treatment and services, including: medical history and physical evaluations, consultations and prescribing medication in accordance with DEA certificate. Urethral, bladder catheterization ___ ___ ___ Suprapubic, bladder aspiration ___ ___ ___ Page 1 Printed on Wednesday, December 10, 2014 Delineation Of Privileges Urology Privileges Provider -

Time Course of Immune Recovery and Viral Reactivation Following Hematopoietic Stem Cell Transplantation
CLINICAL ARTICLES Cellular Therapy and Transplantation (CTT). Vol.5, No.4 (17), 2016 doi: 10.18620/ctt-1866-8836-2016-5-4-32-43 Submitted:02 November 2016, accepted: 09 December 2016 Time course of immune recovery and viral reactivation following hematopoietic stem cell transplantation 1Olga S. Pankratova, 2Alexei B. Chukhlovin 1Tampere University Hospital, Tampere, Finland 2R. Gorbacheva Memorial Research Institute of Children Oncology, Hematology and Transplantation, The St. Petersburg State I. Pavlov Medical University CD8+ cells specific for cytomegalovirus (CMV), or Ep- Summary stein-Barr virus (EBV) rapidly expand in cases of CMV or EBV activation. Total depletion of innate and adaptive immune cell pop- ulations occurs after intensive chemotherapy and he- Despite recovery of absolute B-cell counts by day 30 matopoietic stem cell transplantation (HSCT) then fol- post-HSCT, their functions, i.e., antigen-specific anti- lowed by gradual recovery of immune populations, due body production, are reduced for months and years after to progenitors derived from donor hematopoietic cells HSCT, due to slow restoration of mature immune cell which differentiate to myeloid and lymphoid lineages. populations, thus resemling normal evolution of B cell Time dynamics of immune reconstitution and differen- hierarchy in human organism. tial maturation of distinct immune populations is only partially evaluated, especially, at early terms post-trans- Reactivation of herpesviruses (mostly, CMV, EBV and plant. E.g., innate immunity is restored within 1st month Herpes Simplex) is a known feature of immune de- after HSCT, due to rapid reconstitution of granulocytes, ficiency. Timing of maximal herpesvirus incidence monocytes, and natural killer (NK) cells. -

Chapter 118: Transplantation-Related Malignancies
CHAPTER 118 — REFERENCES 1. Bhatia S, Ramsay NK, Steinbuch M, et al. Malignant neoplasms following 30. Ellis NA, Huo D, Yildiz O, et al. MDM2 SNP309 and TP53 Arg72Pro in- bone marrow transplantation. Blood 1996;87:3633–3639. teract to alter therapy-related acute myeloid leukemia susceptibility. Blood 2. Witherspoon RP, Fisher LD, Schoch G, et al. Secondary cancers after bone 2008;112:741–749. marrow transplantation for leukemia or aplastic anemia. N Engl J Med 31. Casorelli I, Offman J, Mele L, et al. Drug treatment in the development 1989;321:784–789. of mismatch repair defective acute leukemia and myelodysplastic syndrome. 3. Curtis RE, Rowlings PA, Deeg HJ, et al. Solid cancers after bone marrow DNA Repair (Amst) 2003;2:547–559. transplantation. N Engl J Med 1997;336:897–904. 32. Seedhouse CH, Das-Gupta EP, Russell NH. Methylation of the hMLH1 4. Krishnan A, Bhatia S, Slovak ML, et al. Predictors of therapy-related leuke- promoter and its association with microsatellite instability in acute myeloid mia and myelodysplasia following autologous transplantation for lymphoma: leukemia. Leukemia 2003;17:83–88. an assessment of risk factors. Blood 2000;95:1588–1593. 33. Seedhouse C, Faulkner R, Ashraf N, et al. Polymorphisms in genes involved 5. Rowlings PA, Curtis RE, Passweg JR, et al. Increased incidence of Hodg- in homologous recombination repair interact to increase the risk of develop- kin’s disease after allogeneic bone marrow transplantation. J Clin Oncol ing acute myeloid leukemia. Clin Cancer Res 2004;10:2675–2680. 1999;17:3122–3127. 34. Matullo G, Palli D, Peluso M, et al. -

Autotransplantation of the Third Molar: a Therapeutic Alternative to the Rehabilitation of a Missing Tooth: a Scoping Review
bioengineering Review Autotransplantation of the Third Molar: A Therapeutic Alternative to the Rehabilitation of a Missing Tooth: A Scoping Review Mario Dioguardi 1,* , Cristian Quarta 1 , Diego Sovereto 1, Giuseppe Troiano 1 , Michele Melillo 1, Michele Di Cosola 1, Angela Pia Cazzolla 1 , Luigi Laino 2 and Lorenzo Lo Muzio 1 1 Department of Clinical and Experimental Medicine, University of Foggia, Via Rovelli 50, 71122 Foggia, Italy; [email protected] (C.Q.); [email protected] (D.S.); [email protected] (G.T.); [email protected] (M.M.); [email protected] (M.D.C.); [email protected] (A.P.C.); [email protected] (L.L.M.) 2 Multidisciplinary Department of Medical-Surgical and Odontostomatological Specialties, University of Campania “Luigi Vanvitelli”, 80121 Naples, Italy; [email protected] * Correspondence: [email protected] Abstract: Introduction: Tooth autotransplantation is the repositioning of an erupted, partially erupted, or non-erupted autologous tooth from one site to another within the same individual. Several factors influence the success rate of the autotransplant, such as the stage of root development, the morphology of the tooth, the surgical procedure selected, the extraoral time, the shape of the recipient socket, the vascularity of the recipient bed, and the vitality of the cells of the periodontal ligament. The aim of this scoping review was to provide the most up-to-date information and data on the clinical principles of the third-molar autograft and thus provide clinical considerations for its success. Citation: Dioguardi, M.; Quarta, C.; Materials and methods: This review was conducted based on PRISMA-ScR (Preferred Reporting Sovereto, D.; Troiano, G.; Melillo, M.; Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews). -

Public Use Data File Documentation
Public Use Data File Documentation Part III - Medical Coding Manual and Short Index National Health Interview Survey, 1995 From the CENTERSFOR DISEASECONTROL AND PREVENTION/NationalCenter for Health Statistics U.S. DEPARTMENTOF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics CDCCENTERS FOR DlSEASE CONTROL AND PREVENTlON Public Use Data File Documentation Part Ill - Medical Coding Manual and Short Index National Health Interview Survey, 1995 U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics Hyattsville, Maryland October 1997 TABLE OF CONTENTS Page SECTION I. INTRODUCTION AND ORIENTATION GUIDES A. Brief Description of the Health Interview Survey ............. .............. 1 B. Importance of the Medical Coding ...................... .............. 1 C. Codes Used (described briefly) ......................... .............. 2 D. Appendix III ...................................... .............. 2 E, The Short Index .................................... .............. 2 F. Abbreviations and References ......................... .............. 3 G. Training Preliminary to Coding ......................... .............. 4 SECTION II. CLASSES OF CHRONIC AND ACUTE CONDITIONS A. General Rules ................................................... 6 B. When to Assign “1” (Chronic) ........................................ 6 C. Selected Conditions Coded ” 1” Regardless of Onset ......................... 7 D. When to Assign -

A Nationwide Analysis of Kidney Autotransplantation
A Nationwide Analysis of Kidney Autotransplantation ZHOBIN MOGHADAMYEGHANEH, M.D., MARK H. HANNA, M.D., REZA FAZLALIZADEH, M.D., YOSHITSUGU OBI, M.D., PH.D., CLARENCE E. FOSTER, M.D., MICHAEL J. STAMOS, M.D., HIROHITO ICHII, M.D., PH.D. From the Department of Surgery, University of California, Irvine, School of Medicine, Orange, California There are limited data regarding outcomes of patients underwent kidney autotransplantation. This study aims to investigate outcomes of such patients. The nationwide inpatient sample database was used to identify patients underwent kidney autotransplantation during 2002 to 2012. Multivariate analyses using logistic regression were performed to investigate morbidity predictors. A total of 817 patients underwent kidney autotransplantation from 2002 to 2012. The most common indication of surgery was renal artery pathology (22.7%) followed by ureter pathology (17%). Overall, 97.7 per cent of operations were performed in urban teaching hospitals. The number of procedures from 2008 to 2012 were significantly higher compared with the number of them from 2002 to 2007 (473 vs 345, P < 0.01). The overall mortality and morbidity of patients were 1.3 and 46.2 per cent, respectively. The most common postoperative complications were transplanted kidney failure (10.7%) followed by hemorrhagic complications (9.7%). Obesity [adjusted odds ratio (AOR): 9.62, P < 0.01], fluid and electrolyte disorders (AOR: 3.67, P < 0.01), and preoperative chronic kidney disease (AOR: 1.80, P 5 0.03) were predictors of morbidity in patients. In conclusion, Kidney autotransplantation is associated with low mortality but a high morbidity rate. The most common indications of kidney autotransplantation are renal artery and ureter pathologies, respectively. -

Ureteroscopic Treatment of Larger Renal Calculi (>2 Cm)
Thomas Jefferson University Jefferson Digital Commons Department of Urology Faculty Papers Department of Urology 9-1-2012 Ureteroscopic treatment of larger renal calculi (>2 cm). Demetrius H. Bagley Thomas Jefferson University Kelly A. Healy Thomas Jefferson University Nir Kleinmann Thomas Jefferson University Follow this and additional works at: https://jdc.jefferson.edu/urologyfp Part of the Urology Commons Let us know how access to this document benefits ouy Recommended Citation Bagley, Demetrius H.; Healy, Kelly A.; and Kleinmann, Nir, "Ureteroscopic treatment of larger renal calculi (>2 cm)." (2012). Department of Urology Faculty Papers. Paper 45. https://jdc.jefferson.edu/urologyfp/45 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in Department of Urology Faculty Papers by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Arab Journal of Urology (2012) 10, 296–300 Arab Journal of Urology (Official Journal of the Arab -

Outpatient Immunosuppressive Drugs Under Medicare
Outpatient Immunosuppressive Drugs Under Medicare July 1991 OTA-H-452 NTIS order #PB92-117720 Recommended Citation: U.S. Congress, Office of Technology Assessment, Outpatient Immunosuppressive Drugs Under Medicare, OTA-H-452 (Washington, DC: U.S. Government Printing Office, Septem- ber 1991). For sale by the U.S. Government Printing Office Superintendent of Documents, Mail Stop: SSOP, Washington, DC 20402-9328” ISBN 0-16 -035315-7 Foreword Of all the astonishing achievements of modern medicine, the ability to successfully transplant a living organ from one human being to another is perhaps one of the most awesome. Immunosuppressive drugs are one of the spectrum of technological advances that have made organ transplants an everyday phenomenon. At the same time, however, transplant recipients’ needs for these drugs have presented Medicare with a continuing policy dilemma, because Medicare does not usually pay for outpatient prescription drugs. In 1984, the year after cyclosporine made its debut onto the health care market, OTA reported to Congress on the likely benefits of the drug for Medicare kidney transplant recipients. The present report, requested by the Senate Committee on Finance in the wake of the repeal of the Medicare Catastrophic Coverage Act, examines Medicare’s current immunosuppressive drug coverage dilemma and the policy tradeoffs it entails for the 1990s. OTA reports would not be possible without the assistance and input of a wide variety of individuals from both the public and the private sectors. OTA staff and contractors gratefully acknowledge the contributions of the many people who provided data, clarified facts, presented views, and reviewed the drafts of this report. -

Xenotransplantation of Ovarian Tissue Into Male
XENOTRANSPLANTATION OF OVARIAN TISSUE INTO MALE IMMUNODEFICIENT MICE by HUGO JOSE HERNANDEZ FONSECA (Under the direction of BENJAMÍN G. BRACKETT) ABSTRACT A male immunodeficient mouse model for transplantation of ovarian tissue was investigated. Bovine and human ovarian tissues were surgically placed either under the kidney capsule or in the subcutaneous spaces of male non obese diabetic (NOD) severe combined immunodeficient (SCID) mice. Time intervals required for development of growing follicles were determined for neonatal and adult bovine ovarian tissue grafts. This interval was much shorter (P <0.01) in adult tissue than in one-week-old calf tissue, i.e. 55 vs 124 days. The increase in the proportion of growing follicles was coincidental with a decrease in the proportion of resting follicles. This increment in the growing follicle populations took place abruptly and was significant by 55 days and by 124 days after transplantation in the adult cow and calf ovarian grafts, respectively. Recovery of oocytes from bovine ovarian grafts was successful. Several immature oocytes were recovered and evidence of maturation in one oocyte was obtained after 24 hours of in vitro maturation. Treatment of host mice with an FSH:LH preparation increased follicular development but did not enhance oocyte recovery rates. Human ovarian tissue grafted under the kidney capsule of intact male NOD SCID mice showed a greater proportion of growing follicles than similar grafts transplanted to the kidney of castrated hosts and to the subcutaneous space of intact hosts. However, no differences in follicular growth and development were detected between the intact/ kidney capsule and the castrated / subcutaneous groups. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular