Hurricane Katrina: Health Outcomes and the from Selected Official Documents Purpose of the Project
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

GAO-08-1120 Disaster Recovery: Past Experiences Offer Insights For
United States Government Accountability Office Report to the Committee on Homeland GAO Security and Governmental Affairs, U.S. Senate September 2008 DISASTER RECOVERY Past Experiences Offer Insights for Recovering from Hurricanes Ike and Gustav and Other Recent Natural Disasters GAO-08-1120 September 2008 DISASTER RECOVERY Accountability Integrity Reliability Past Experiences Offer Insights for Recovering from Highlights Hurricanes Ike and Gustav and Other Recent Natural Highlights of GAO-08-1120, a report to the Disasters Committee on Homeland Security and Governmental Affairs, U.S. Senate Why GAO Did This Study What GAO Found This month, Hurricanes Ike and While the federal government provides significant financial assistance after Gustav struck the Gulf Coast major disasters, state and local governments play the lead role in disaster producing widespread damage and recovery. As affected jurisdictions recover from the recent hurricanes and leading to federal major disaster floods, experiences from past disasters can provide insights into potential declarations. Earlier this year, good practices. Drawing on experiences from six major disasters that heavy flooding resulted in similar declarations in seven Midwest occurred from 1989 to 2005, GAO identified the following selected insights: states. In response, federal agencies have provided millions of • Create a clear, implementable, and timely recovery plan. Effective dollars in assistance to help with recovery plans provide a road map for recovery. For example, within short- and long-term recovery. 6 months of the 1995 earthquake in Japan, the city of Kobe created a State and local governments bear recovery plan that identified detailed goals which facilitated coordination the primary responsibility for among recovery stakeholders. -

Resilience Potential: Assessing Jamaica's “Bounce-Back” from Hurricane Dean
Resilience Potential: Assessing Jamaica’s “Bounce-Back” from Hurricane Dean CaPRI is a Caribbean think tank that promotes evidence- based policymaking in the region. CaPRI espouses a methodology which is built on the values of multi- disciplinary work, team work and the utilization of the diaspora in our search for evidence. Committed to the region’s development, CaPRI has strong linkages with the academic community, the private sector and civil society. For information and feedback, please contact: Caribbean Policy Research Institute GUANGO TREE HOUSE, 29 MUNROE ROAD, KINGSTON 6 JAMAICA, W.I. TEL: (876) 970-3447 (876) 970-2910 FAX: (876) 970-4544 E-mail: [email protected] WEBSITE: http://www.takingresponsibility.org 2 Table of Contents Pages List of Figures, Tables and Boxes .............................................................4 Preface......................................................................................................5 Executive Summary .................................................................................6-7 Introduction: Resilience Potential ...........................................................8-9 1. Natural Disasters: The Global Context................................................10-13 2. Natural Disasters in the Caribbean .....................................................14-18 3. Changing Practices in Disaster Management…………………………19-20 4. Disaster Management in Jamaica .....................................................21 4.1 National Disaster Plan…………………………………………….21 -

Teaching the Levees
Teaching The Levees 7 Times-Picayune staff graphic by Emmett Mayer III; staff photos by Ellis Lucia, Alex Brandon, and Devaunshi Mahadevia Teaching The Levees A Curriculum for Democratic Dialogue and Civic Engagement 7 MARGARET SMITH CROCCO, Editor Teachers College Columbia University New York R This work is dedicated to the residents of the Gulf States, who survived the ravages of Hurricane Katrina by helping one another, and to those who died so tragically. R Published by Teachers College Press, 1234 Amsterdam Avenue, New York, NY 10027 Copyright © 2007 Teachers College, Columbia University. All rights reserved. This publication was made possible by a grant from the Rockefeller Foundation. Grateful acknowledgment is made to the following sources for permission to use their materials: Afro-American Newspapers Archives and Research Center for excerpt The Opportunity Agenda for reprinting of “The Opportunity from “Spike Lee captures pain, hope of Hurricane Katrina Agenda’s six core values” survivors,” by Zenitha Prince (August 26, 2006) Pew Research Center for reprinting of “Katrina has only modest AlterNet for excerpt from “Media hurricane is so much hot air,” by impact on basic public values” (September 22, 2005) Rory O’Connor (September 14, 2005) The Poynter Institute for excerpts from “Best practices: Images of The American Conservative for an excerpt from “The emperor’s new disaster and how they were captured,” by David Frank consensus,” by Scott McConnell (October 10, 2005) (September 3, 2005), and from “Katrina photos: A gallery & notes Associated Press for excerpts from “For now the offi cial Hurricane from photo editors,” by Kenny Irby (September 4, 2005) Katrina death toll stands at 1,697” (October 29, 2006) and from Reuters News Service for excerpt from “US censoring Katrina “Up to 35,000 kids still having major Katrina problems,” by Janet coverage,” by Deborah Zabarenko (September 8, 2005) McConnaughey (February 2, 2007) Joni Seager for excerpt from “Natural disasters expose gender divide,” Philip S. -
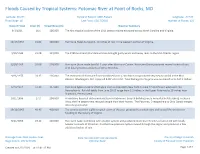
Floods Caused by Tropical Systems: Potomac River at Point of Rocks, MD
Floods Caused by Tropical Systems: Potomac River at Point of Rocks, MD Latitude: 39.274 Period of Record: 1889-Present Longitude: -77.543 Flood Stage: 16 Last Flood: 12/17/2018 Number of Floods: 121 Date of Flood Crest (ft) Streamflow (cfs) Weather Summary 9/1/1911 16.1 106,000 The first tropical cyclone of the 1911 season moved eastward across North Carolina and Virginia. 10/17/1954 21.02 130,000 Hurricane Hazel dumped 6- 10 inches of rain in the western portion of Virginia. 9/20/1945 21.98 139,000 The 1945 Southeast Florida Hurricane brought gusty winds and heavy rains to the Mid-Atlantic region. 8/20/1955 29.08 214,000 Hurricane Diane made landfall 5 days after Hurricane Connie. Hurricane Diane produced several inches of rain with locally heavier amounts of 10 to 20 inches. 9/26/1975 24.35 126,000 The remnants of Hurricane Eloise combined with a cold front and produced very heavy rainfall in the Mid- Atlantic. Washington, D.C. reported 9.08" of rainfall. Total damage for Virginia was estimated to be $17.2 million. 6/23/1972 37.43 347,000 Hurricane Agnes made landfall again over southeastern New York on June 22 and moved westward into Pennsylvania. Rainfall totals from June 20-25 range from 2-3 inches in the Upper Potomac to 18 inches near Shamokin, Pennsylvania. 10/1/1896 27.2 204,000 A hurricane knocked out communication in Richmond. Several buildings were unroofed in Petersburg. In Buena Vista, the fire department rescued people from their homes. -

FEMA FOIA Log – 2018
Mirandra Abrams, Monique any and all records concerning clients. Kindly provide our office with 10/4/2017 Sambursky a complete copy of clients entire file as it pertains as it pertains to Slone Sklarin Inquiry Number (b) (6) ; Voucher Number (b) (6) ; Payee Verveniotis Reference Number (b) (6) in your possession. 2017-FEFO-02138 - Masters, Mark all contract documents related to temporary staffing services 10/5/2017 contracts for emergency call center support for FEMA in the last five 2017-FEFO-02177 (5) years 2017-FEFO-02187 - (b) (6) all files, correspondence, or other records concerning yourself 10/6/2017 Dallas News Benning, Tom 1) All active FEMA contracts for manufactured housing units. 2) All 10/13/2017 active FEMA individual assistance/technical assistance contracts (IATACs). 3) All pre-event contracts for debris removal that are overseen by FEMA Region 6. 4) All pre-event contracts for housing assistance that are overseen by FEMA Region 6. 5) All noncompetitive disaster relief contracts approved by FEMA since August 14, 2017. 6) All non-local disaster relief contracts approved by FEMA since August 14, 2017, including the written justification 2017-FEFO-02214 for choosing a non-local vendor. FCI Keys, Clay a copy of any and all records related to [FEMA's] response to 10/23/2017 SEAGOVILLE hurricane Katrina, including all memoranda, communications and records of any kind and from any source from August 29, 2005 to 2012. (Date Range for Record Search: From 8/29/2005 To 2017-FEFO-02239 12/1/2012) - (b) (6) Any files related to yourself (Date Range for Record Search: From 10/24/2017 2017-FEFO-02240 1/1/2000 To 9/11/2017) - McClain, Don every individual who has requested assistance by FEMA from both 10/31/2017 Hurricane Irma and Harvey. -

Hurricane and Tropical Storm
State of New Jersey 2014 Hazard Mitigation Plan Section 5. Risk Assessment 5.8 Hurricane and Tropical Storm 2014 Plan Update Changes The 2014 Plan Update includes tropical storms, hurricanes and storm surge in this hazard profile. In the 2011 HMP, storm surge was included in the flood hazard. The hazard profile has been significantly enhanced to include a detailed hazard description, location, extent, previous occurrences, probability of future occurrence, severity, warning time and secondary impacts. New and updated data and figures from ONJSC are incorporated. New and updated figures from other federal and state agencies are incorporated. Potential change in climate and its impacts on the flood hazard are discussed. The vulnerability assessment now directly follows the hazard profile. An exposure analysis of the population, general building stock, State-owned and leased buildings, critical facilities and infrastructure was conducted using best available SLOSH and storm surge data. Environmental impacts is a new subsection. 5.8.1 Profile Hazard Description A tropical cyclone is a rotating, organized system of clouds and thunderstorms that originates over tropical or sub-tropical waters and has a closed low-level circulation. Tropical depressions, tropical storms, and hurricanes are all considered tropical cyclones. These storms rotate counterclockwise in the northern hemisphere around the center and are accompanied by heavy rain and strong winds (National Oceanic and Atmospheric Administration [NOAA] 2013a). Almost all tropical storms and hurricanes in the Atlantic basin (which includes the Gulf of Mexico and Caribbean Sea) form between June 1 and November 30 (hurricane season). August and September are peak months for hurricane development. -

Lessons Learned from Hurricane Sandy and Recommendations for Improved Healthcare and Public Health Response and Recovery for Future Catastrophic Events
Lessons Learned from Hurricane Sandy and Recommendations for Improved Healthcare and Public Health Response and Recovery for Future Catastrophic Events Final Report December 22, 2015 Lessons Learned from Hurricane Sandy and Recommendations for Improved Healthcare and Public Health Response and Recovery for Future Catastrophic Events BACKGROUND A “classic late-season…extraordinarily large hurricane,” 1 Sandy was the 18th named tropical cyclone of the 2012 Atlantic hurricane season. It made landfall along the mid-Atlantic coast near Atlantic City, NJ about 6:30 pm on October 29, 2012 as a Category 1 hurricane with 80- mph maximum sustained winds. But due to its extensive breadth (winds above 40 mph (tropical storm force) stretched 900 miles), Sandy’s real damage was done by a calamitous storm surge that merged with a high tide to produce a storm surge, primarily pounding the New Jersey, New York, and Connecticut coastlines (Figure 1). The United States Geological Survey measured water levels on Staten Island, New York at almost eight feet above ground level. Even after the storm moved on, it impacted inland states, including Ohio, West Virginia, and Indiana, with high winds, soaking rains, and even heavy snow in the Appalachians. 2,3 Very High: > 10,000 people exposed to surge High: 500 – 10,000 people exposed to surge OR > $100 million in wind damage OR > 8” rain Moderate: 100 – 500 people exposed to surge OR $10 - $100 million in wind damage OR 4” - 8” rain Low: no surge impacts OR < $10 million in wind damage OR < 4” rain Figure 1. 2 FEMA Hurricane Sandy Impact Analysis The consequences of the storm’s destructive power were significant. -

A FAILURE of INITIATIVE Final Report of the Select Bipartisan Committee to Investigate the Preparation for and Response to Hurricane Katrina
A FAILURE OF INITIATIVE Final Report of the Select Bipartisan Committee to Investigate the Preparation for and Response to Hurricane Katrina U.S. House of Representatives 4 A FAILURE OF INITIATIVE A FAILURE OF INITIATIVE Final Report of the Select Bipartisan Committee to Investigate the Preparation for and Response to Hurricane Katrina Union Calendar No. 00 109th Congress Report 2nd Session 000-000 A FAILURE OF INITIATIVE Final Report of the Select Bipartisan Committee to Investigate the Preparation for and Response to Hurricane Katrina Report by the Select Bipartisan Committee to Investigate the Preparation for and Response to Hurricane Katrina Available via the World Wide Web: http://www.gpoacess.gov/congress/index.html February 15, 2006. — Committed to the Committee of the Whole House on the State of the Union and ordered to be printed U. S. GOVERNMEN T PRINTING OFFICE Keeping America Informed I www.gpo.gov WASHINGTON 2 0 0 6 23950 PDF For sale by the Superintendent of Documents, U.S. Government Printing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512-1800; DC area (202) 512-1800 Fax: (202) 512-2250 Mail: Stop SSOP, Washington, DC 20402-0001 COVER PHOTO: FEMA, BACKGROUND PHOTO: NASA SELECT BIPARTISAN COMMITTEE TO INVESTIGATE THE PREPARATION FOR AND RESPONSE TO HURRICANE KATRINA TOM DAVIS, (VA) Chairman HAROLD ROGERS (KY) CHRISTOPHER SHAYS (CT) HENRY BONILLA (TX) STEVE BUYER (IN) SUE MYRICK (NC) MAC THORNBERRY (TX) KAY GRANGER (TX) CHARLES W. “CHIP” PICKERING (MS) BILL SHUSTER (PA) JEFF MILLER (FL) Members who participated at the invitation of the Select Committee CHARLIE MELANCON (LA) GENE TAYLOR (MS) WILLIAM J. -

US Energy Industry Response to Recent Hurricane Seasons
Hardening and Resiliency U.S. Energy Industry Response to Recent Hurricane Seasons Infrastructure Security and Energy Restoration Office of Electricity Delivery and Energy Reliability U.S. Department of Energy August 2010 For Further Information This report was prepared by the Office of Electricity Delivery and Energy Reliability under the direction of Patricia Hoffman, Assistant Secretary, and William Bryan, Deputy Assistant Secretary. Specific questions about information in this report may be directed to Alice Lippert, Senior Technical Advisor ([email protected]). Contributors include Mindi Farber-DeAnda, Matthew Cleaver, Carleen Lewandowski, and Kateri Young. Cover photo sources: Lineman photo: David H. Lewis/istockphoto.com Pipeline photo: Christian Lagereek/istockphoto.com Refinery photo: Erik de Graaf/istockphoto.com Mobile transformer photo: Deltastar, reproduced with permission. OE/ISER Final Report 8/16/10 i Table of Contents Executive Summary ........................................................................................................................ v Background ..................................................................................................................................... 1 Focus of the Study .......................................................................................................................... 3 Aging Infrastructure and Hurricane Hazards .............................................................................. 5 Storm Surge and Flood Damage ............................................................................................ -

Hurricane Katrina and New Orleans: Discursive Spaces of Safety and Resulting Environmental Injustice
HURRICANE KATRINA AND NEW ORLEANS: DISCURSIVE SPACES OF SAFETY AND RESULTING ENVIRONMENTAL INJUSTICE A dissertation submitted to Kent State University in partial fulfillment of the requirements for the degree of Doctor of Philosophy by Andrew B. Shears August, 2011 Dissertation written by Andrew B. Shears B.S., Ball State University, 2003 M.S., Ball State University, 2005 Ph.D., Kent State University, 2011 Approved by ____________________________________, Chair, Doctoral Dissertation Committee Dr. James A. Tyner ____________________________________, Members, Doctoral Dissertation Committee Dr. Mandy Munro-Stasiuk ____________________________________ Dr. Robert M. SchwartZ ____________________________________ Dr. Scott C. Sheridan Accepted by ____________________________________, Chair, Department of Geography Dr. Mandy Munro-Stasiuk ____________________________________, Dean, College of Arts and Sciences Dr. Timothy Moerland ii TABLE OF CONTENTS LIST OF FIGURES……………………………………………..………………………………………………….iv ACKNOWLEDGEMENTS………………………………………………………………………………………vi DEDICATION……………………………………………………………………………………………………...vii CHAPTER I. INTRODUCTION…………………………………………………………………………………..1 A. DEFINING ENVIRONMENTAL JUSTICE………………………………………….3 B. THE GAME PLAN………………………………………………………………………..19 C. METHODOLOGICAL FRAMEWORK……………………………………………..20 II. ABOUT NEW ORLEANS……………………………………………………………………...29 A. THE HISTORY OF NEW ORLEANS……………………………………………….33 B. NEW ORLEANS IN 2005…………….……………………………………………….85 C. CONCLUSION…………………………………………………………………………...111 III. HURRICANE KATRINA……………………………………………………………………..113 -

Lessons Learned: Evacuations Management of Hurricane Gustav
4th Symposium on Policy and Socio-Economic Research, American Meteorological Society, Phoenix, AZ, 2009. 2.5 LESSONS LEARNED: EVACUATIONS MANAGEMENT OF HURRICANE GUSTAV Gina M. Eosco1, Mark A. Shafer2, and Barry Keim3 1Department of Communications, University of Oklahoma 2Oklahoma Climatological Survey, University of Oklahoma 3 Department of Geography and Anthropology, Louisiana State University Experience is what you get when you don’t get what you want. The experience of Hurricane Katrina was not what anyone in New Orleans wanted, yet three years after New Orleans was struck by Hurricane Katrina, the city proved they were ready for the next big one. As the National Hurricane Center forecasts started indicating a possible category 3 or stronger hurricane heading towards Louisiana, the city began preparations for evacuation. Gulf coast residents responded with the largest evacuation in U.S. history. Given the contrast with Katrina, why was the response to Gustav so much better? It is true that government officials learned from Katrina, but Katrina was just one milestone along the way toward making New Orleans safer. This paper examines prior recent experience with hurricanes in Louisiana, events surrounding Hurricane Gustav, and Figure 1. Track of Hurricane Georges, September how we have learned from other disasters. Not only 20-27, 1998 (Image source: Unisys did Louisiana officials learn from prior hurricanes, http://weather.unisys.com/hurricane/). but those far-removed from the area of impact learned from their own disaster experiences to hurricane Georges was uncoordinated and chaotic. manage the influx of evacuees. The progression of Each parish had its own separate response plan. -

Tropical Topics Week 2021 NWS Florida &
5/21/2021 Tornado Recognition, Impacts & Messaging Scott Spratt; NWS Melbourne | Robert Molleda; NWS Miami 1 TC Tornadoes Tornado Recognition, Impacts & Messaging 2 1 5/21/2021 TC Tornadoes Today’s Presentation Topics • Previous Events • Climatology/Favorable Patterns • Worse Case Scenario • Threat/Impact Messaging Hurricane Irma September 10, 2017 EF-1 Tornado 1124 am | Indialantic, FL • Future Improvements 3 TC Tornadoes What is the relative threat? Which tropical cyclone hazard poses the greatest threat? A. Wind B. Storm Surge Flooding C. Heavy Rainfall Flooding D. Tornadoes E. It depends – on the particular storm/hurricane; and on where you are located 4 2 5/21/2021 The TC Tornado Hazard can be Significant A Specific Example – Tropical Storm Gordon (1994) T Barefoot Bay, FL November 16, 1994 Nearly 500 MH damaged Including 62 destroyed Tropical storm center at 1 Fatality; 40 injuries time of tornado T Tornado location 5 TC Tornadoes Threat Recognition, Impacts & Messaging The primary Tropical Cyclone (TC) tornado challenges are. 1) Predicting tornadoes outside the area where people are prepared for hurricane force winds; or prior to the damaging hurricane wind onset. 2) Predicting tornadoes from weaker systems where tornadoes may pose the greatest threat. 3) Minimizing the amount of over-warning. 4) Successfully Messaging #1-3 6 3 5/21/2021 TC Tornadoes Addressing the primary challenges • Threat Assessment • Impact Recognition • Effective Messaging 7 TC Tornado Development Diagnosing the local tornado hazard • Certain weather factors enhance the tornado potential of landfalling or paralleling systems: ✓ Strong low-level wind shear (maximized in right-front quadrant). ✓ Pockets of dry air (enhance instability; isolated cells).