19 May 2011 (19.05.2011) 1 a Z
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

International Journal of Scientific Research and Reviews
Saha Sudipta, IJSRR 2018, 7(3), 1749-1768 Review article Available online www.ijsrr.org ISSN: 2279–0543 International Journal of Scientific Research and Reviews Novel Antitussive Agents from Natural Source-A Review Saha Sudipta* Assistant Professor, Department of Chemistry, TrivenideviBhalotia College, Raniganj, PaschimBardhaman, West-Bengal, India, Pin-713347 Email: [email protected]; Mobile No:-+91-94343486121 ABSTRACT Cough, acts as the defender of the foreign materials and secretions from the airways. Cough gives the protection of the lungs and distal parts of airways from chocking and infected mucus. Cough is one of the major worldwide problem as patients suffering from this visit physician. In this way it leads to the economical problem in the society. The mostly used and available antitussive agents in the markets are codeine and dextromethorphan. Although they are good cough suppressing but they have also numerous side effects e.g., sedation, nausea, addictive potential, and constipation. Although a new class of antitussive drugs are not coming into the market for a long time. To solve this problem pharmacists and researchers are searching novel, less toxic, more effective antitussive drugs from the nature. Plant derived medicines act as the supplementary to the synthetic drugs followed by engineered protein and gene therapy. In this context pharmacotherapy provides some novel alkaloids, triterpenoids, phenolglycosides, polysaccharides, flavonoids, as more effective and less toxic antitussive agents. These said phytochemicals isolated from botanical source play a major role in the treatment of many respiratory diseases including cough. Some of the above mentioned extracts from the shrubs are used in the Indian traditional medicine, they can be used as a safe antitussive agents. -
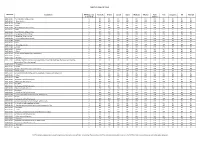
TARIFF SCHEDULE of CHILE Description MFN Base Rate
TARIFF SCHEDULE OF CHILE Tariff Line Description MFN Base rate Australia Brunei Canada Japan Malaysia Mexico New Peru Singapore US Vietnam (1 Jan 2010) Zealand 0101.10.00 -Pure-bred breeding animals 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0101.90.11 ---Race horses 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0101.90.19 ---Other 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0101.90.90 --Other 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0102.10.00 -Pure-bred breeding animals 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0102.90.00 -Other 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0103.10.00 -Pure-bred breeding animals 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0103.91.00 --Weighing less than 50 kg 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0103.92.00 --Weighing 50 kg or more 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0104.10.10 --Pure-bred breeding animals 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0104.10.90 --Other 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0104.20.00 -Goats 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0105.11.10 ---Breeding animals 6 EIF EIF B8 EIF EIF EIF EIF EIF EIF EIF EIF 0105.11.90 ---Other 6 EIF EIF B8 EIF EIF EIF EIF EIF EIF EIF EIF 0105.12.00 --Turkeys 6 EIF EIF B8 EIF EIF EIF EIF EIF EIF EIF EIF 0105.19.00 --Other 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF 0105.94.00 --Fowls of the species Gallus domesticus 6 EIF EIF B8 EIF EIF EIF EIF EIF EIF EIF EIF 0105.99.00 --Other 6 EIF EIF B8 EIF EIF EIF EIF EIF EIF EIF EIF 0106.11.00 --Primates 6 EIF EIF EIF EIF EIF EIF EIF EIF EIF EIF -

Product List March 2019 - Page 1 of 53
Wessex has been sourcing and supplying active substances to medicine manufacturers since its incorporation in 1994. We supply from known, trusted partners working to full cGMP and with full regulatory support. Please contact us for details of the following products. Product CAS No. ( R)-2-Methyl-CBS-oxazaborolidine 112022-83-0 (-) (1R) Menthyl Chloroformate 14602-86-9 (+)-Sotalol Hydrochloride 959-24-0 (2R)-2-[(4-Ethyl-2, 3-dioxopiperazinyl) carbonylamino]-2-phenylacetic 63422-71-9 acid (2R)-2-[(4-Ethyl-2-3-dioxopiperazinyl) carbonylamino]-2-(4- 62893-24-7 hydroxyphenyl) acetic acid (r)-(+)-α-Lipoic Acid 1200-22-2 (S)-1-(2-Chloroacetyl) pyrrolidine-2-carbonitrile 207557-35-5 1,1'-Carbonyl diimidazole 530-62-1 1,3-Cyclohexanedione 504-02-9 1-[2-amino-1-(4-methoxyphenyl) ethyl] cyclohexanol acetate 839705-03-2 1-[2-Amino-1-(4-methoxyphenyl) ethyl] cyclohexanol Hydrochloride 130198-05-9 1-[Cyano-(4-methoxyphenyl) methyl] cyclohexanol 93413-76-4 1-Chloroethyl-4-nitrophenyl carbonate 101623-69-2 2-(2-Aminothiazol-4-yl) acetic acid Hydrochloride 66659-20-9 2-(4-Nitrophenyl)ethanamine Hydrochloride 29968-78-3 2,4 Dichlorobenzyl Alcohol (2,4 DCBA) 1777-82-8 2,6-Dichlorophenol 87-65-0 2.6 Diamino Pyridine 136-40-3 2-Aminoheptane Sulfate 6411-75-2 2-Ethylhexanoyl Chloride 760-67-8 2-Ethylhexyl Chloroformate 24468-13-1 2-Isopropyl-4-(N-methylaminomethyl) thiazole Hydrochloride 908591-25-3 4,4,4-Trifluoro-1-(4-methylphenyl)-1,3-butane dione 720-94-5 4,5,6,7-Tetrahydrothieno[3,2,c] pyridine Hydrochloride 28783-41-7 4-Chloro-N-methyl-piperidine 5570-77-4 -

IIIHIIIUSOO5304377A Unitedo States Patent 19 (11) Patent Number: 5,304,377 Yamada Et Al
IIIHIIIUSOO5304377A UnitedO States Patent 19 (11) Patent Number: 5,304,377 Yamada et al. (45) Date of Patent: Apr. 19, 1994 54 PROLONGED RELEASE PREPARATION 4,954,298 9/1990 Yamamoto et al. ................. 264/4.6 AND POLYMERS THEREOF 4,962,091 10/1990 Eppstein et al. ........................ 514/2 75) Inventors: Minoru Yamada; Seiko Ishiguro, both 5,061,492 10/1991 Okada et al. ........................ 424/423 Otokuni, all of Japan 0052510 11/1981 European Pat. Off. 73) Assignee: Sherical4. industries, Ltd., O256726O190833 7/19871/1986 European Pat. Off. a, Japan 0263490 10/1987 European Pat. Off. (21) Appl. No.: 986,299 0281482 3/1988 European Pat. Off. 035.0246 7/1989 European Pat. Off. 22 Filed: Dec. 7, 1992 2-212436 8/1990 Japan. Related U.S. Application Data OTHER PUBLICATIONS 63) continuation of ser. No. 777,170, oct. 16, 1991, aban- Chemical Abstracts, vol. 114/No. 6 (Feb. 11, 1991); doned. Columbus, Ohio; Abstract No. 49615R. 30 Foreign Application Priority Data Primary Ent, S. Sir Mueller & Oct. 16, 1990 (JP) Japan .................................. 2-278037 story Agent, or Firm-Wegner, Cantor, Mueller Aug. 28, 1991 JP Japan .................................. 3.217045 51 Int, Cl. ......................... A61K 9/22; A61K 9/52; ' ABSTRACT A61K 31/74 A polymer for a prolonged release preparation which 52 U.S. Cl. ................................. 424/426; 424/78.08; comprises 424/78.37; 424/434; 424/457; 424/468; (A) a polylactic acid and 424/486; 424/497; 525/450, 514/2 (B) a copolymer of glycolic acid and a hydroxycar 58) Field of Search .................. 424/426, 78.08, 78.37, boxylic acid of general formula 424/434, 457, 468, 486, 497; 525/450; 514/2 (56) References Cited R U.S. -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

(12) Patent Application Publication (10) Pub. No.: US 2004/0224012 A1 Suvanprakorn Et Al
US 2004O224012A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2004/0224012 A1 Suvanprakorn et al. (43) Pub. Date: Nov. 11, 2004 (54) TOPICAL APPLICATION AND METHODS Related U.S. Application Data FOR ADMINISTRATION OF ACTIVE AGENTS USING LIPOSOME MACRO-BEADS (63) Continuation-in-part of application No. 10/264,205, filed on Oct. 3, 2002. (76) Inventors: Pichit Suvanprakorn, Bangkok (TH); (60) Provisional application No. 60/327,643, filed on Oct. Tanusin Ploysangam, Bangkok (TH); 5, 2001. Lerson Tanasugarn, Bangkok (TH); Suwalee Chandrkrachang, Bangkok Publication Classification (TH); Nardo Zaias, Miami Beach, FL (US) (51) Int. CI.7. A61K 9/127; A61K 9/14 (52) U.S. Cl. ............................................ 424/450; 424/489 Correspondence Address: (57) ABSTRACT Eric G. Masamori 6520 Ridgewood Drive A topical application and methods for administration of Castro Valley, CA 94.552 (US) active agents encapsulated within non-permeable macro beads to enable a wider range of delivery vehicles, to provide longer product shelf-life, to allow multiple active (21) Appl. No.: 10/864,149 agents within the composition, to allow the controlled use of the active agents, to provide protected and designable release features and to provide visual inspection for damage (22) Filed: Jun. 9, 2004 and inconsistency. US 2004/0224012 A1 Nov. 11, 2004 TOPCAL APPLICATION AND METHODS FOR 0006 Various limitations on the shelf-life and use of ADMINISTRATION OF ACTIVE AGENTS USING liposome compounds exist due to the relatively fragile LPOSOME MACRO-BEADS nature of liposomes. Major problems encountered during liposome drug Storage in vesicular Suspension are the chemi CROSS REFERENCE TO OTHER cal alterations of the lipoSome compounds, Such as phos APPLICATIONS pholipids, cholesterols, ceramides, leading to potentially toxic degradation of the products, leakage of the drug from 0001) This application claims the benefit of U.S. -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -

Pharmaceutical Manufacturing Formulations Liquid Products V () L UME Sarfaraz K
HANDBOOK OF Pharmaceutical Manufacturing Formulations Liquid Products V () L UME Sarfaraz K. Niazi CRC PRESS Boca Raton London New York Washington, D.C. Table of Contents PART I Regulatory and Manufacturing Guidance 1 Chapter 1 Current Good Manufacturing Practice Considerations in Liquid Manufacturing 3 I. Introduction 3 II. Facilities 3 III. Equipment 3 IV. Raw Materials 4 V. Compounding 4 VI. Microbiological Quality 4 VII. Oral Suspensions 5 VIII. Product Specifications 5 IX. Process Validation 5 X. Stability 5 XI. Packaging 6 Chapter 2 Stability Testing of New Drug Substances and Products 7 I. Introduction 7 II. Drug Substance 7 A. General Case 8 B. Drug Substances Intended for Storage in a Refrigerator 8 C. Drag Substances Intended for Storage in a Freezer 8 D. Drug Substances Intended for Storage below -20°C 9 HI. Drag Product 10 A. General Case •' B. Drag Products Packaged in Impermeable Containers 11 C. Drag Products Packaged in Semipermeable Containers 11 D. Drag Products Intended for Storage in a Refrigerator 12 E. Drag Products Intended for Storage in a Freezer 13 F. Drag Products Intended for Storage below -20"C 13 IV Glossary 14 References 1() Chapter 3 Container Closure Systems '7 I. Introduction '7 A. Definitions '7 B. Current Good Manufacturing Practice, the Consumer Product Safety Commission, and Requirements on Containers and Closures 17 C. Additional Considerations 17 II. Qualification and Quality Control of Packaging Components 18 A. Description 21 B. Information about Suitability 21 C. Stability Data (Packaging Concerns) 22 D. Inhalation Drag Products 23 E. Injection and Ophthalmic Drag Products 23 F. -

Genl:VE 1970 © World Health Organization 1970
Nathan B. Eddy, Hans Friebel, Klaus-Jiirgen Hahn & Hans Halbach WORLD HEALTH ORGANIZATION ORGANISATION .MONDIALE DE LA SANT~ GENl:VE 1970 © World Health Organization 1970 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. Nevertheless governmental agencies or learned and professional societies may reproduce data or excerpts or illustrations from them without requesting an authorization from the World Health Organization. For rights of reproduction or translation of WHO publications in toto, application should be made to the Division of Editorial and Reference Services, World Health Organization, Geneva, Switzerland. The World Health Organization welcomes such applications. Authors alone are responsible for views expressed in signed articles. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the Director-General of the World Health Organization concerning the legal status of any country or territory or of its authorities, or concerning the delimitation of its frontiers. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. © Organisation mondiale de la Sante 1970 Les publications de l'Organisation mondiale de la Sante beneficient de la protection prevue par les dispositions du Protocole n° 2 de la Convention universelle pour la Protection du Droit d'Auteur. Les institutions gouvernementales et les societes savantes ou professionnelles peuvent, toutefois, reproduire des donnees, des extraits ou des illustrations provenant de ces publications, sans en demander l'autorisation a l'Organisation mondiale de la Sante. Pour toute reproduction ou traduction integrate, une autorisation doit etre demandee a la Division des Services d'Edition et de Documentation, Organisation mondiale de la Sante, Geneve, Suisse. -

(12) United States Patent (10) Patent No.: US 8,603,526 B2 Tygesen Et Al
USOO8603526B2 (12) United States Patent (10) Patent No.: US 8,603,526 B2 Tygesen et al. (45) Date of Patent: Dec. 10, 2013 (54) PHARMACEUTICAL COMPOSITIONS 2008. O152595 A1 6/2008 Emigh et al. RESISTANT TO ABUSE 2008. O166407 A1 7/2008 Shalaby et al. 2008/0299.199 A1 12/2008 Bar-Shalom et al. 2008/0311205 A1 12/2008 Habib et al. (75) Inventors: Peter Holm Tygesen, Smoerum (DK); 2009/0022790 A1 1/2009 Flath et al. Jan Martin Oevergaard, Frederikssund 2010/0203129 A1 8/2010 Andersen et al. (DK); Karsten Lindhardt, Haslev (DK); 2010/0204259 A1 8/2010 Tygesen et al. Louise Inoka Lyhne-versen, Gentofte 2010/0239667 A1 9/2010 Hemmingsen et al. (DK); Martin Rex Olsen, Holbaek 2010, O291205 A1 11/2010 Downie et al. (DK); Anne-Mette Haahr, Birkeroed 2011 O159100 A1 6/2011 Andersen et al. (DK); Jacob Aas Hoellund-Jensen, FOREIGN PATENT DOCUMENTS Frederikssund (DK); Pemille Kristine Hoeyrup Hemmingsen, Bagsvaerd DE 20 2006 014131 1, 2007 (DK) EP O435,726 8, 1991 EP O493513 7, 1992 EP O406315 11, 1992 (73) Assignee: Egalet Ltd., London (GB) EP 1213014 6, 2002 WO WO 89,09066 10, 1989 (*) Notice: Subject to any disclaimer, the term of this WO WO91,040 15 4f1991 patent is extended or adjusted under 35 WO WO95/22962 8, 1995 U.S.C. 154(b) by 489 days. WO WO99,51208 10, 1999 WO WOOOf 41704 T 2000 WO WO 03/024426 3, 2003 (21) Appl. No.: 12/701,429 WO WOO3,O24429 3, 2003 WO WOO3,O24430 3, 2003 (22) Filed: Feb. -

(12) United States Patent (10) Patent No.: US 9,314.465 B2 Brew Et Al
US009314465B2 (12) United States Patent (10) Patent No.: US 9,314.465 B2 Brew et al. (45) Date of Patent: *Apr. 19, 2016 (54) DRUG COMBINATIONS AND USES IN 2008.0003280 A1 1/2008 Levine et al. ................. 424/456 TREATING A COUGHING CONDITION 2008/O176955 A1 7/2008 Hecket al. 2008, 0220078 A1 9, 2008 Morton et al. (71) Applicant: Infirst Healthcare Limited 2009, O136427 A1 5/2009 Croft et al. 2009, O220594 A1 9, 2009 Field (72) Inventors: John Brew, London (GB); Robin Mark 2012/O128738 A1 5, 2012 Brew et al. Bannister, London (GB) 2012fO252824 A1 10/2012 Brew et al. (73) Assignee: Infirst Healthcare Limited, London FOREIGN PATENT DOCUMENTS (GB) CN 1593451 3, 2005 CN 101024.014 A 8, 2007 (*) Notice: Subject to any disclaimer, the term of this CN 101112383 B 5, 2010 patent is extended or adjusted under 35 DE 4420708 A1 12, 1995 U.S.C. 154(b) by 0 days. EP 2050435 B1 4/2009 GB 2114001 A 8, 1983 This patent is Subject to a terminal dis GB 2284761 A 6, 1995 claimer. GB 2424.185 B 9, 2006 GB 2442828 A 4/2008 JP 62-249924 A 10, 1987 (21) Appl. No.: 14/287,014 JP H1O-316568 A 12/1998 JP 2001-518928 A 10, 2001 (22) Filed: May 24, 2014 JP 200219.3839. A T 2002 JP 2003-012514 A 1, 2003 (65) Prior Publication Data JP 20030552.58 A 2, 2003 JP 2003128549 A 5, 2003 US 2014/O256750 A1 Sep. 11, 2014 JP 2003-321357 A 11, 2003 JP 2005-516917 A 6, 2005 JP 2008O31146 A 2, 2008 Related U.S. -

Pharmacology on Your Palms CLASSIFICATION of the DRUGS
Pharmacology on your palms CLASSIFICATION OF THE DRUGS DRUGS FROM DRUGS AFFECTING THE ORGANS CHEMOTHERAPEUTIC DIFFERENT DRUGS AFFECTING THE NERVOUS SYSTEM AND TISSUES DRUGS PHARMACOLOGICAL GROUPS Drugs affecting peripheral Antitumor drugs Drugs affecting the cardiovascular Antimicrobial, antiviral, Drugs affecting the nervous system Antiallergic drugs system antiparasitic drugs central nervous system Drugs affecting the sensory Antidotes nerve endings Cardiac glycosides Antibiotics CNS DEPRESSANTS (AFFECTING THE Antihypertensive drugs Sulfonamides Analgesics (opioid, AFFERENT INNERVATION) Antianginal drugs Antituberculous drugs analgesics-antipyretics, Antiarrhythmic drugs Antihelminthic drugs NSAIDs) Local anaesthetics Antihyperlipidemic drugs Antifungal drugs Sedative and hypnotic Coating drugs Spasmolytics Antiviral drugs drugs Adsorbents Drugs affecting the excretory system Antimalarial drugs Tranquilizers Astringents Diuretics Antisyphilitic drugs Neuroleptics Expectorants Drugs affecting the hemopoietic system Antiseptics Anticonvulsants Irritant drugs Drugs affecting blood coagulation Disinfectants Antiparkinsonian drugs Drugs affecting peripheral Drugs affecting erythro- and leukopoiesis General anaesthetics neurotransmitter processes Drugs affecting the digestive system CNS STIMULANTS (AFFECTING THE Anorectic drugs Psychomotor stimulants EFFERENT PART OF THE Bitter stuffs. Drugs for replacement therapy Analeptics NERVOUS SYSTEM) Antiacid drugs Antidepressants Direct-acting-cholinomimetics Antiulcer drugs Nootropics (Cognitive