Use of Inhaled Human Insulin in Patients with Diabetes Mellitus Meghan K
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![LANTUS® (Insulin Glargine [Rdna Origin] Injection)](https://docslib.b-cdn.net/cover/0369/lantus%C2%AE-insulin-glargine-rdna-origin-injection-60369.webp)
LANTUS® (Insulin Glargine [Rdna Origin] Injection)
Rev. March 2007 Rx Only LANTUS® (insulin glargine [rDNA origin] injection) LANTUS® must NOT be diluted or mixed with any other insulin or solution. DESCRIPTION LANTUS® (insulin glargine [rDNA origin] injection) is a sterile solution of insulin glargine for use as an injection. Insulin glargine is a recombinant human insulin analog that is a long-acting (up to 24-hour duration of action), parenteral blood-glucose-lowering agent. (See CLINICAL PHARMACOLOGY). LANTUS is produced by recombinant DNA technology utilizing a non- pathogenic laboratory strain of Escherichia coli (K12) as the production organism. Insulin glargine differs from human insulin in that the amino acid asparagine at position A21 is replaced by glycine and two arginines are added to the C-terminus of the B-chain. Chemically, it is 21A- B B Gly-30 a-L-Arg-30 b-L-Arg-human insulin and has the empirical formula C267H404N72O78S6 and a molecular weight of 6063. It has the following structural formula: LANTUS consists of insulin glargine dissolved in a clear aqueous fluid. Each milliliter of LANTUS (insulin glargine injection) contains 100 IU (3.6378 mg) insulin glargine. Inactive ingredients for the 10 mL vial are 30 mcg zinc, 2.7 mg m-cresol, 20 mg glycerol 85%, 20 mcg polysorbate 20, and water for injection. Inactive ingredients for the 3 mL cartridge are 30 mcg zinc, 2.7 mg m-cresol, 20 mg glycerol 85%, and water for injection. The pH is adjusted by addition of aqueous solutions of hydrochloric acid and sodium hydroxide. LANTUS has a pH of approximately 4. CLINICAL PHARMACOLOGY Mechanism of Action: The primary activity of insulin, including insulin glargine, is regulation of glucose metabolism. -

Comparison of Adjunctive Therapy with Metformin and Acarbose in Patients with Type-1 Diabetes Mellitus
Original Article Comparison of adjunctive therapy with metformin and acarbose in patients with Type-1 diabetes mellitus Amir Ziaee1, Neda Esmailzadehha2, Maryam Honardoost3 ABSTRACT Objective: All the aforementioned data have stimulated interest in studying other potential therapies for T1DM including noninsulin pharmacological therapies. The present study attempts to investigate the effect of adjunctive therapy with metformin and acarbose in patients with Type-1 diabetes mellitus. Method: In a single-center, placebo-controlled study (IRCT201102165844N1) we compared the results of two clinical trials conducted in two different time periods on 40 patients with Type-1 diabetes mellitus. In the first section, metformin was given to the subjects.After six months, metformin was replaced with acarbose in the therapeutic regimen. In both studies, subjects were checked for their BMI, FBS, HbA1C, TGs, Cholesterol, LDL, HDL, 2hpp, unit of NPH and regular insulin variations. Results: Placebo-controlled evaluation of selected factors has showna significant decrease in FBS and TG levels in the metformin group during follow up but acarbose group has shown substantial influence on two hour post prandial (2hpp) and regular insulin intake decline.Moreover, Comparison differences after intervention between two test groups has shown that metformin has had superior impact on FBS and HbA1C decline in patients. Nonetheless, acarbose treatment had noteworthy influence on 2hpp, TGs, Cholesterol, LDL, and regular insulin intake control. Conclusion: The results of this experiment demonstrate that the addition of acarbose or metformin to patients with Type-1 diabetes mellitus who are controlled with insulin is commonly well tolerated and help to improve metabolic control in patients. -

Diabetes Mellitus: Patterns of Pharmaceutical Use in Manitoba
Diabetes Mellitus: Patterns of Pharmaceutical Use in Manitoba by Kim¡ T. G. Guilbert A Thesis submitted to The Faculty of Graduate Studies in Partial Fulfillment of the Requirements for the Degree of MASTER OF SCIENCE Faculty of Pharmacy The University of Manitoba Winnipeg, Manitoba @ Kimi T.G. Guilbert, March 2005 TIIE UMYERSITY OF MANITOBA F'ACULTY OF GRADUATE STTJDIES +g+ù+ COPYRIGIIT PERMISSION PAGE Diabetes Mellitus: Patterns of Pharmaceutical Use in Manitoba BY Kimi T.G. Guilbert A ThesisÆracticum submitted to the Faculty of Graduate Studies of The University of Manitoba in partial fulfillment of the requirements of the degree of MASTER OF SCIENCE KIMI T.G. GTIILBERT O2()O5 Permission has been granted to the Library of The University of Manitoba to lend or sell copies of this thesis/practicum, to the National Library of Canada to microfïlm this thesis and to lend or sell copies of the film, and to University Microfilm Inc. to publish an abstract of this thesis/practicum. The author reserves other publication rights, and neither this thesis/practicum nor extensive extracts from it may be printed or otherwise reproduced without the author's written permission. Acknowledgements Upon initiation of this project I had a clear objective in mind--to learn more. As with many endeavors in life that are worthwhile, the path I have followed has brought me many places I did not anticipate at the beginning of my journey. ln reaching the end, it is without a doubt that I did learn more, and the knowledge I have been able to take with me includes a wider spectrum than the topic of population health and medication utilization. -

KFHC DRUG FORMULARY Iii Preface FORMULARY
Drug Formulary prescribe generic first TM TM 9700 Stockdale Highway Bakersfield, California 93311-3617 1-800-391-2000 kernfamilyhealthcare.com L NK Drug Formulary February 2020 February 2020 The Kern Family Health Care Drug Formulary includes information boxes prior to some of the major therapeutic categories. Please use these tools to assist with your care of our members. TM This symbol indicates some or all of the dosage forms are available generically. Prescribing generic brands of medication is key to keeping the escalating medication costs down to a minimum. Kern Health Systems PMPM medication cost is approaching $35. 65 This symbol indicates a drug identified by National Committee for Quality Assurance (NCQA) as a high risk medication for the elderly and should generally be avoided for this population. Please consider a formulary alternative. Q This symbol indicates the drug should be billed to Medicare Part B as primary and Kern Family Health Care as a secondary payer. 1 This symbol indicates a tier. It will designate the tier only in regards to cost share. It does not reflect any step-therapy status. KFHC DRUG FORMULARY iii Preface FORMULARY The member identification number will be the CIN number. This is a number assigned by the state and is not the social security number. Kern Family Health Care (KHS Medi-Cal) BIN 600428 PCN 04970000 Pt. Number is CIN Number Formulary OTC’s Covered Formulary Prenatal Vitamins Covered (OTC included) Formulary Contraceptives Covered No copayments TAR’s allowed for OTC and legend PHARMACY AND THERAPEUTICS COMMITTEE The Pharmacy and Therapeutics Committee is composed of Physician and Pharmacist community providers as well as staff from Kern Health Systems. -

Type 2 Diabetes Adult Outpatient Insulin Guidelines
Diabetes Coalition of California TYPE 2 DIABETES ADULT OUTPATIENT INSULIN GUIDELINES GENERAL RECOMMENDATIONS Start insulin if A1C and glucose levels are above goal despite optimal use of other diabetes 6,7,8 medications. (Consider insulin as initial therapy if A1C very high, such as > 10.0%) 6,7,8 Start with BASAL INSULIN for most patients 1,6 Consider the following goals ADA A1C Goals: A1C < 7.0 for most patients A1C > 7.0 (consider 7.0-7.9) for higher risk patients 1. History of severe hypoglycemia 2. Multiple co-morbid conditions 3. Long standing diabetes 4. Limited life expectancy 5. Advanced complications or 6. Difficult to control despite use of insulin ADA Glucose Goals*: Fasting and premeal glucose < 130 Peak post-meal glucose (1-2 hours after meal) < 180 Difference between premeal and post-meal glucose < 50 *for higher risk patients individualize glucose goals in order to avoid hypoglycemia BASAL INSULIN Intermediate-acting: NPH Note: NPH insulin has elevated risk of hypoglycemia so use with extra caution6,8,15,17,25,32 Long-acting: Glargine (Lantus®) Detemir (Levemir®) 6,7,8 Basal insulin is best starting insulin choice for most patients (if fasting glucose above goal). 6,7 8 Start one of the intermediate-acting or long-acting insulins listed above. Start insulin at night. When starting basal insulin: Continue secretagogues. Continue metformin. 7,8,20,29 Note: if NPH causes nocturnal hypoglycemia, consider switching NPH to long-acting insulin. 17,25,32 STARTING DOSE: Start dose: 10 units6,7,8,11,12,13,14,16,19,20,21,22,25 Consider using a lower starting dose (such as 0.1 units/kg/day32) especially if 17,19 patient is thin or has a fasting glucose only minimally above goal. -

Insulin : Past, Present and Future
2016.5.13. 29th Spring Congress of Korean Diabetes Association Insulin : Past, Present and Future Seung-Hwan Lee, MD, PhD Seoul St.Mary’s Hospital The Catholic Univ. of Korea 본 발표와 관련된 이해관계 • 강의 및 자문료: Sanofi Aventis, Eli Lilly History of glucose-lowering drugs Kahn SE et al. Lancet, 2014 Groundwork for the discovery of insulin Josef Von Mering Oskar Minkowski Paul Langerhans (1849-1908) (1858-1931) (1847-88) pancreatectomy in dog displayed polyuria, small clusters of cells in thirst, hyperphagia pancreas separated from exocrine & ductal tissue demonstrated blood glucose lowering properties of pancreas “islets of Langerhans” Insulin in medical history: 4 Nobel prizes Frederick Sanger Chemistry 1958 Aminoacid sequence of insulin Dorothy Hodgkin Frederick Banting & John Macleod Chemistry 1964 Medicine 1923 X-ray crystallography Discovery of insulin Rosalyn Yalow Medicine 1977 RIA Charles Best James Collip Developments in insulin therapy: a journey not a destination Isolation Hagedorn protamine of insulin -retarded insulin Recombinant human Basal (Banting & Macleod) NPH insulin insulin analogues 1922 1946 1977 2000s Time The beginning 1923 1950s 1990s Animal insulin p Lente® insulin Rapid-acting reparations series insulin analogues NPH, neutral protamine Hagedorn Isolation of insulin • 1921: Banting and Best filter pancreatic tissue to produce ‘isletin’ in Professor Macleod’s laboratory at the University of Toronto • Purification of insulin by Bertram Collip First use of insulin in human January 1922: At Toronto General Hospital, 14-year-old Leonard Thompson was the first human to receive insulin • Banting and Best injected a 14-year-old “charity” patient who weighed 29 kg with 7.5 ml of a “thick brown muck” in each buttock. -

United States Experience of Insulin Degludec Alone Or in Combination for Type 1 and Type 2 Diabetes
Journal name: Drug Design, Development and Therapy Article Designation: Review Year: 2017 Volume: 11 Drug Design, Development and Therapy Dovepress Running head verso: Rendell Running head recto: Degludec insulin in the USA open access to scientific and medical research DOI: http://dx.doi.org/10.2147/DDDT.S132581 Open Access Full Text Article REVIEW United States experience of insulin degludec alone or in combination for type 1 and type 2 diabetes Marc Rendell1,2 Abstract: Insulin degludec has been the product of a sophisticated and systematic biochemical 1The Rose Salter Medical Research engineering program which began with the release of insulin detemir. The goal was to pro- Foundation, 2The Association of duce a long-lasting basal insulin with low individual variability. Certainly, this goal has been Diabetes Investigators, Newport achieved. Degludec has a duration of action approaching twice that of glargine. Another advan- Coast, CA, USA tage of degludec is in its lack of unpredictable copolymerization of added aspart. In several studies, degludec has shown lower rates of nocturnal hypoglycemia than glargine. Degludec can be administered flexibly with a very flat insulin concentration curve at any time of day. Initial US Food and Drug Administration concerns about a possible increase in cardiac events in degludec-treated patients have been allayed by the results of a study targeting individuals with high cardiac risk. Degludec is now marketed in the US competing with glargine. Despite the long duration of action of degludec, attempted administration three times weekly resulted For personal use only. in less effective lowering of glycated hemoglobin and an increased incidence of hypoglycemia compared to daily glargine. -
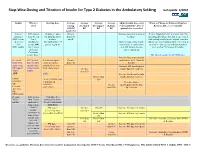
Step-Wise Dosing and Titration of Insulin for Type 2 Diabetes in the Ambulatory Setting Last Update 5/2010
Step -Wise Dosing and Titration of Insulin for Type 2 Diabetes in the Ambulatory Setting last update 5/2010 Insulin When to Starting dose Average Average Average Average Adjust Insulin dose every When to Change to Different Regimen start fasting Pre-lunch Pre-supper Bedtime 3 days until BG < 130, or Recheck A1C every 3 months AM BG BG BG BG optimal dose is reached Goal<130 Lantus A1C greater 10 units or up to Greater Increase dose by 2-4 units at If after 3 months if A1c is greater than 7% (glargine) than 8% on 0.2 units/kg SQ at than 130 bedtime. and optimal bedtime dose has been reached OR Levemir 2 or 3 bedtime mg/dL with fasting blood glucose at goal, consider (detemir) antidiabetic (DC sulfonylurea if Optimal long acting (basal) adding a pre-meal bolus insulin at the largest OR agents OR part of regimen) insulin dose keeps bedtime meal of the day, pre-meal bolus insulin at NPH insulin 1 or 2 agents and AM fasting glucose each meal or 70/30 premix insulin. if Serum values consistent. Creatinine greater than 2 DC all oral agents except Metformin. Increase long acting (basal) Pre-meal A1C greater 2-4 units of rapid Greater insulin dose by 2-4 units at bolus with than 7% with acting or regular than 130 bedtime rapid acting optimal long insulin SQ at each Increase AM rapid/regular OR regular acting (basal) meal (base dose) Greater insulin dose by 2-4 units. insulin insulin. than 130 AND with Increase lunch rapid/regular Greater than insulin dose by 2-4 units. -

Timely Addition of Insulin to Oral Therapy for Type 2 Diabetes
EDITORIAL Timely Addition of Insulin to Oral Therapy for Type 2 Diabetes he U.K. Prospective Diabetes Study betes to treatment with diet alone, insulin (usually by 20–50%) the requirement for (UKPDS) has shaped our view of the alone, or a sulfonylurea alone initially, but exogenous insulin, which cannot be T management of type 2 diabetes insulin was added when fasting blood adapted to varying needs after injection, more than any other trial. It proved that glucose was persistently Ͼ108 mg/dl. especially during exercise, when mobili- glycemic control limits retinopathy (and The sulfonylureas used were glipizide or zation of insulin from subcutaneous de- probably other microvascular complica- chlorpropamide, perhaps because earlier pots can inappropriately increase. tions) as much for type 2 diabetic patients in the trial, glyburide was associated with Ongoing sulfonylurea treatment may also as had previously been shown for type 1 more hypoglycemia. Insulin was given enhance the opportunity for normal diabetic patients (1). It defined the pro- first as ultralente alone, with mealtime downregulation of endogenous insulin gressive natural history of type 2 diabetes, regular insulin added subsequently as when blood glucose declines. These with declining -cell function over time needed. As in the main UKPDS protocol, mechanisms could lead to smaller within- and a need for progressively more active both pharmacotherapeutic regimens out- and between-day variations of blood glu- treatment to maintain glycemic control performed diet alone. However, the regi- cose as well as less risk of hypoglycemia at (2). In addition, it has offered important men mandating the timely addition of any mean level of glycemia, resulting in insights into the effects of several forms of insulin to a sulfonylurea proved superior the opportunity to achieve lower HbA1c treatment. -

Combination Use of Insulin and Incretins in Type 2 Diabetes
Canadian Agency for Agence canadienne Drugs and Technologies des médicaments et des in Health technologies de la santé CADTH Optimal Use Report Volume 3, Issue 1C Combination Use of Insulin and July 2013 Incretins in Type 2 Diabetes Supporting Informed Decisions This report is prepared by the Canadian Agency for Drugs and Technologies in Health (CADTH). The report contains a comprehensive review of the existing public literature, studies, materials, and other information and documentation (collectively the “source documentation”) available to CADTH at the time of report preparation. The information in this report is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. The information in this report should not be used as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process, nor is it intended to replace professional medical advice. While CADTH has taken care in the preparation of this document to ensure that its contents are accurate, complete, and up to date as of the date of publication, CADTH does not make any guarantee to that effect. CADTH is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in the source documentation. CADTH is not responsible for any errors or omissions or injury, loss, or damage arising from or relating to the use (or misuse) of any information, statements, or conclusions contained in or implied by the information in this document or in any of the source documentation. -

Randomized Controlled Clinical Trial of Glargine Versus Ultralente Insulin in the Treatment of Type 1 Diabetes
Clinical Care/Education/Nutrition ORIGINAL ARTICLE Randomized Controlled Clinical Trial of Glargine Versus Ultralente Insulin in the Treatment of Type 1 Diabetes 1 1 YOGISH C. KUDVA, MD, MBBS JULIE A. GEBEL, RN poglycemia (1). In the past, ultralente or 1 2 ANANDA BASU, MD DEBRA A. VOGELSANG, NP NPH insulin were commonly used to pro- 1 1 GREGORY D. JENKINS, MS STEVEN A. SMITH, MD vide basal insulin concentrations (2). 2 1 GUILLERMO M. PONS, MD ROBERT A. RIZZA, MD 1 1 More recently, glargine has been LORI L. QUANDT, RN WILLIAM L. ISLEY, MD shown to be an effective basal insulin preparation. Several studies have shown that when compared with NPH insulin, use of glargine as a basal insulin prepara- OBJECTIVE — Multiple daily insulin injection programs are commonly accompanied by tion results in comparable or lower HbA considerable glycemic variation and hypoglycemia. We conducted a randomized crossover 1c design clinical trial to compare glargine with ultralente insulin as a basal insulin in type 1 concentrations and lower frequency of diabetes. nocturnal hypoglycemia (3). However, the observation that nocturnal hypoglyce- RESEARCH DESIGN AND METHODS — To determine whether the use of glargine mia was lower with glargine than NPH insulin as a basal insulin would result in a comparable HbA1c and less glycemic variation and insulin is not particularly surprising since hypoglycemia than ultralente insulin, 22 individuals (aged 44 Ϯ 14 years [ϮSD], 55% men) with insulin concentrations peak 6–8 h after type 1 diabetes who were experienced with multiple daily insulin injections and had an HbA1c Ͻ injection (i.e., in the middle of the night) of 7.8% were randomized in a crossover design to receive either glargine or ultralente as the when NPH insulin is injected at bedtime. -

Combination Therapies with Insulin in Type 2 Diabetes
Reviews/Commentaries/Position Statements REVIEW ARTICLE Combination Therapies With Insulin in Type 2 Diabetes 1 HANNELE YKI-JA¨RVINEN, MD, FRCP patients who are poorly controlled on oral drugs. One may also predict from these data that if the insulin dose is lowered less than ϳ30% when patients are transferred he U.K. Prospective Diabetes Study lar end points but only on surrogate from insulin alone to insulin combined (UKPDS) demonstrated that inten- markers of risk of micro- and macrovas- with sulfonylurea or metformin, glycemic T sive glucose control with insulin or cular complications, mostly data on gly- control will be better during insulin com- sulfonylureas markedly reduces the risk cemia, body weight, insulin doses, lipids, bination therapy. This is documented by of microvascular complications (1). For and in a few studies, also accurate data on analysis of data from studies in previously myocardial infarction, the reduction in the frequency of hypoglycemias. insulin-treated patients (Table 2). In these comparisons, glycemic control was better risk (16% for a 0.9% decrease in HbA1c) According to a Medline search (1966– was of borderline significance but corre- 2000), insulin alone has been compared in most (19 of 25) comparisons, but the sponded closely to epidemiological pre- with insulin combination therapy in a to- insulin dose was decreased by only 19% dictions (14% decrease for a 1% drop in tal of 34 prospective studies that lasted at in the combination regimens using met- HbA ) (2). These data demonstrated that least 2 months and reported data on HbA formin and by 21% in comparisons using 1c 1 insulin and sulfonylureas (Table 2).