Integrin-Mediated Regulation of Epidermal Wound Functions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

Met Receptor Tyrosine Kinase: Enhanced Signaling Through Adapter Proteins
Oncogene (2000) 19, 5582 ± 5589 ã 2000 Macmillan Publishers Ltd All rights reserved 0950 ± 9232/00 $15.00 www.nature.com/onc Met receptor tyrosine kinase: enhanced signaling through adapter proteins Kyle A Furge1, Yu-Wen Zhang1 and George F Vande Woude*,1 1Van Andel Research Institute, 333 Bostwick, N.E., Grand Rapids, Michigan, MI 49503, USA The Met receptor tyrosine kinase is the prototypic matrix (`invasion') (Jeers et al., 1996c; Matsumoto et member of a small subfamily of growth factor receptors al., 1994; Rong et al., 1994; Weidner et al., 1990). In that when activated induce mitogenic, motogenic, and addition, HGF/SF-Met signaling can induce several morphogenic cellular responses. The ligand for Met is dierent epithelial and mesenchymal cell types to hepatocyte growth factor/scatter factor (HGF/SF) and undergo an involved dierentiation program termed while normal HGF/SF-Met signaling is required for branching morphogenesis when the cells are grown in a embryonic development, abnormal Met signaling has three dimensional matrix (Brinkmann et al., 1995; been strongly implicated in tumorigenesis, particularly in Jeers et al., 1996c; Montesano et al., 1991a; Niemann the development of invasive and metastatic phenotypes. et al., 1998). During branching morphogenesis, groups Following ligand binding and autophosphorylation, Met of cells proliferate, migrate, and dierentiate to form a transmits intercellular signals using a unique multi- connected series of tubules arranged like branches from substrate docking site present within the C-terminal a tree. However, even in the absense of a three end of the receptor. The multisubstrate docking site dimensional matrix, signaling through the Met receptor mediates the binding of several adapter proteins such as can induce morphogenesis and lumen formation in Grb2, SHC, Crk/CRKL, and the large adapter protein certain cell types (Jeers et al., 1996a; Tsarfaty et al., Gab1. -

Silencing of ITGB6 Inhibits the Progression of Cervical Carcinoma Via Regulating JAK/STAT3 Signaling Pathway
803 Original Article Page 1 of 12 Silencing of ITGB6 inhibits the progression of cervical carcinoma via regulating JAK/STAT3 signaling pathway Xiaoxia Zheng, Yanan Zhu, Xiaoping Wang, Yanmei Hou, Yingji Fang Jinan Maternity and Child Care Hospital Affiliated to Shandong First Medical University/Jinan Maternity and Child Care Hospital Affiliated, Jinan, China Contributions: (I) Conception and design: Y Fang; (II) Administrative support: Y Hou; (III) Provision of study materials or patients: X Zheng, Y Zhu, X Wang; (IV) Collection and assembly of data: X Zheng, Y Zhu, X Wang; (V) Data analysis and interpretation: X Zheng, Y Zhu, X Wang; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Yingji Fang. Jinan Maternity and Child Care Hospital Affiliated to Shandong First Medical University/Jinan Maternity and Child Care Hospital Affiliated, No. 2 Jianguo Xiaojingsan Road, Jinan 250001, China. Email:[email protected] . Background: Integrin β6 (ITGB6), a key submonomer of integrin αvβ6, plays an important role in epithelial-to-mesenchymal transition (EMT), wound healing, epithelial-derived tumor growth, fibrosis, and epithelial repair. However, the role of ITGB6 in cervical carcinoma (CC) remains elusive. Methods: The expression levels of ITGB6 in CC tissues and cell lines were determined using quantitative real-time polymerase chain reaction (qRT-PCR). The cell viability, proliferation, apoptosis, migration, and invasion were evaluated by Cell Counting Kit-8 (CCK-8), colony-forming, flow cytometry, and Transwell assay, respectively. The expression of related proteins, including EMT markers and the Janus kinase/signal transducer and activator of transcription (JAK/STAT3) signaling markers, were detected using western blotting. -

Paracrine Wnt1 Drives Interstitial Fibrosis Without Inflammation by Tubulointerstitial Cross-Talk
BASIC RESEARCH www.jasn.org Paracrine Wnt1 Drives Interstitial Fibrosis without Inflammation by Tubulointerstitial Cross-Talk † Omar H. Maarouf,* Anusha Aravamudhan,* Deepika Rangarajan,* Tetsuro Kusaba,* ‡ Victor Zhang,* Jeremy Welborn,* Daniel Gauvin,* Xiuyun Hou,* Rafael Kramann,* and † Benjamin D. Humphreys* § *Renal Division, Department of Medicine, Brigham and Women’s Hospital, Boston, Massachusetts; †Harvard Medical School, Boston, Massachusetts; ‡Division of Nephrology and Clinical Immunology and Medical Faculty, Rheinisch- Westfälische Technische Hochschule Aachen University, Aachen, Germany; and §Harvard Stem Cell Institute, Cambridge, Massachusetts ABSTRACT AKI with incomplete epithelial repair is a major contributor to CKD characterized by tubulointerstitial fibrosis. Injury–induced epithelial secretion of profibrotic factors is hypothesized to underlie this link, but the identity of these factors and whether epithelial injury is required remain undefined. We previously showed that activation of the canonical Wnt signaling pathway in interstitial pericytes cell autonomously drives myofibroblast acti- vation in vivo. Here, we show that inhibition of canonical Wnt signaling also substantially prevented TGFb– dependent myofibroblast activation in vitro. To investigate whether Wnt ligand derived from proximal tubule is sufficient for renal fibrogenesis, we generated a novel mouse strain with inducible proximal tubule Wnt1 secretion. Adult mice were treated with vehicle or tamoxifen and euthanized at 12 or 24 weeks postinjection. Compared -

Integrin Β6 Serves As an Immunohistochemical Marker For
www.nature.com/scientificreports OPEN Integrin β6 serves as an immunohistochemical marker for lymph node metastasis and Received: 21 April 2016 Accepted: 29 June 2016 promotes cell invasiveness in Published: 21 July 2016 cholangiocarcinoma Zequn Li1,2, Siddhartha Biswas1,2, Benjia Liang1,2, Xueqing Zou1,2, Liqun Shan1,2, Yang Li1,2, Ruliang Fang1 & Jun Niu1 Cholangiocarcinoma is a devastating malignancy that is notoriously difficult to diagnose and is associated with a high mortality. Despite extensive efforts to improve the diagnosis and treatment of this neoplasm, limited progress has been made. Integrin β6 is a subtype of integrin that is expressed exclusively on the surfaces of epithelial cells and is associated with a variety of tumors. In the present study, we investigated the expression and roles of integrin β6 in cholangiocarcinoma. β6 upregulation in cholangiocarcinoma was correlated with lymph node metastasis and distant metastasis. Moreover, integrin β6 was identified as a biomarker for the diagnosis of cholangiocarcinoma and an indicator of lymph node metastasis. Integrin β6 significantly promoted the proliferation, migration and invasion of cholangiocarcinoma cells. Furthermore, integrin β6 increased Rac1-GTPase, resulting in the upregulation of metalloproteinase-9 (MMP9) and F-actin polymerization. Taken together, our results indicate that integrin β6 promotes tumor invasiveness in a Rac1-dependent manner and is a potential biomarker for tumor metastasis. Integrin β6 may help to improve the diagnostic accuracy, and targeting β6 may be a novel strategy for the treatment of cholangiocarcinoma. Cholangiocarcinoma is neoplasm originating from the ductular epithelium of the biliary tree, either within the liver (intrahepatic cholangiocarcinoma) or more commonly from the extrahepatic bile ducts (extrahepatic cholan- giocarcinoma). -

Paracrine Signaling Mediated at Cellcell Contacts
Insights & Perspectives Think again Paracrine signaling mediated at cellÀcell contacts Sougata Roy*,† and Thomas B. Kornberg Recent findings in several organ systems show that cytoneme-mediated systems. However, recent work that we signaling transports signaling proteins along cellular extensions and targets discuss here describes paracrine signal- cell-to-cell exchanges to synaptic contacts. This mechanism of paracrine ing that is instead contact-mediated and signaling may be a general one that is used by many (or all) cell types in many (or dependent on transient synapses that all) organs. We briefly review these findings in this perspective. We also non-neuronal cells make. These synap- describe the properties of several signaling systems that have previously been ses form at sites where specialized signaling filopodia called cytonemes interpreted to support a passive diffusion mechanism of signaling protein extend to contact target cells. dispersion, but can now be understood in the context of the cytoneme mechanism. Keywords: The classical model of .cytonemes; filopodia; morphogen; paracrine signaling; synapse; TGF-b paracrine signaling assumes that signals disperse by passive Introduction so that signals are within only 15À20 nm diffusion of their target receptors when they are Animal cells communicate over long released. Paracrine signaling, the third There are many paracrine signaling distances in various ways. Endocrine general mechanism, may be considered proteins that have been characterized. cells signal systemically by releasing to be a variant of endocrine signaling, They include the Fibroblast Growth hormones that disseminate in the vas- functioning at relatively short range Factors (FGFs) and other proteins that culature. Neurons also release signals, when secreted signals move limited activate Receptor Tyrosine Kinases, but they exchange information at syn- distances by passive diffusion in extra- TGF-b family members, Wnt proteins, apses that form where their axons and cellular fluid. -
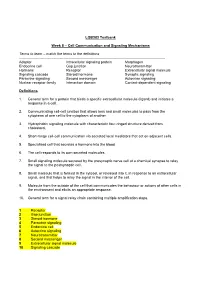
Cell Communication and Signaling Mechanisms Terms to Learn
LQB383 Testbank Week 8 – Cell Communication and Signaling Mechanisms Terms to learn – match the terms to the definitions -------------------------------------------------------------------------------------------------------------------------- Adaptor Intracellular signaling protein Morphogen Endocrine cell Gap junction Neurotransmitter Hormone Receptor Extracellular signal molecule Signaling cascade Steroid hormone Synaptic signaling Paracrine signaling Second messenger Autocrine signaling Nuclear receptor family Interaction domain Contact-dependent signaling Definitions 1. General term for a protein that binds a specific extracellular molecule (ligand) and initiates a response in a cell. 2. Communicating cell-cell junction that allows ions and small molecules to pass from the cytoplasm of one cell to the cytoplasm of another. 3. Hydrophobic signaling molecule with characteristic four-ringed structure derived from cholesterol. 4. Short-range cell-cell communication via secreted local mediators that act on adjacent cells. 5. Specialised cell that secretes a hormone into the blood 6. The cell responds to its own secreted molecules. 7. Small signaling molecule secreted by the presynaptic nerve cell at a chemical synapse to relay the signal to the postsynaptic cell. 8. Small molecule that is formed in the cytosol, or released into it, in response to an extracellular signal, and that helps to relay the signal in the interior of the cell. 9. Molecule from the outside of the cell that communicates the behaviour or actions of other cells in the environment and elicits an appropriate response. 10. General term for a signal relay chain containing multiple amplification steps. 1 Receptor 2 Gap junction 3 Steroid hormone 4 Paracrine signaling 5 Endocrine cell 6 Autocrine signaling 7 Neurotransmitter 8 Second messenger 9 Extracellular signal molecule 10 Signaling cascade Multiple Choice Questions 1. -

Supplementary Table 2
Supplementary Table 2. Differentially Expressed Genes following Sham treatment relative to Untreated Controls Fold Change Accession Name Symbol 3 h 12 h NM_013121 CD28 antigen Cd28 12.82 BG665360 FMS-like tyrosine kinase 1 Flt1 9.63 NM_012701 Adrenergic receptor, beta 1 Adrb1 8.24 0.46 U20796 Nuclear receptor subfamily 1, group D, member 2 Nr1d2 7.22 NM_017116 Calpain 2 Capn2 6.41 BE097282 Guanine nucleotide binding protein, alpha 12 Gna12 6.21 NM_053328 Basic helix-loop-helix domain containing, class B2 Bhlhb2 5.79 NM_053831 Guanylate cyclase 2f Gucy2f 5.71 AW251703 Tumor necrosis factor receptor superfamily, member 12a Tnfrsf12a 5.57 NM_021691 Twist homolog 2 (Drosophila) Twist2 5.42 NM_133550 Fc receptor, IgE, low affinity II, alpha polypeptide Fcer2a 4.93 NM_031120 Signal sequence receptor, gamma Ssr3 4.84 NM_053544 Secreted frizzled-related protein 4 Sfrp4 4.73 NM_053910 Pleckstrin homology, Sec7 and coiled/coil domains 1 Pscd1 4.69 BE113233 Suppressor of cytokine signaling 2 Socs2 4.68 NM_053949 Potassium voltage-gated channel, subfamily H (eag- Kcnh2 4.60 related), member 2 NM_017305 Glutamate cysteine ligase, modifier subunit Gclm 4.59 NM_017309 Protein phospatase 3, regulatory subunit B, alpha Ppp3r1 4.54 isoform,type 1 NM_012765 5-hydroxytryptamine (serotonin) receptor 2C Htr2c 4.46 NM_017218 V-erb-b2 erythroblastic leukemia viral oncogene homolog Erbb3 4.42 3 (avian) AW918369 Zinc finger protein 191 Zfp191 4.38 NM_031034 Guanine nucleotide binding protein, alpha 12 Gna12 4.38 NM_017020 Interleukin 6 receptor Il6r 4.37 AJ002942 -

Biomimetic Surfaces for Cell Engineering
Chapter 18 Biomimetic Surfaces for Cell Engineering John H. Slater, Omar A. Banda, Keely A. Heintz and Hetty T. Nie Cell behavior, in particular, migration, proliferation, differentiation, apoptosis, and activation, is mediated by a multitude of environmental factors: (i) extracellular matrix (ECM) properties including molecular composition, ligand density, ligand gradients, stiffness, topography, and degradability; (ii) soluble factors including type, concentration, and gradients; (iii) cell–cell interactions; and (iv) external forc- es such as shear stress, material strain, osmotic pressure, and temperature changes (Fig. 18.1). The coordinated influence of these environmental cues regulate em- bryonic development, tissue function, homeostasis, and wound healing as well as other crucial events in vivo [1–3]. From a fundamental biology perspective, it is of great interest to understand how these environmental factors regulate cell fate and ultimately cell and tissue function. From an engineering perspective, it is of interest to determine how to present these factors in a well-controlled manner to elicit a de- sired cell output for cell and tissue engineering applications. Both biophysical and biochemical factors mediate intracellular signaling cascades that influence gene ex- pression and ultimately cell behavior [4–7], making it difficult to unravel the hierar- chy of cell fate stimuli [8]. Accordingly, much effort has focused on the fabrication of biomimetic surfaces that recapitulate a single or many aspects of the in vivo mi- croenvironment including topography [9–12], elasticity [5], and ligand presentation [13–17], and by structured materials that allow for control over cell shape [18–23], spreading [18, 23–25], and cytoskeletal tension [26–28]. -

Cell Adhesion Molecules in Normal Skin and Melanoma
biomolecules Review Cell Adhesion Molecules in Normal Skin and Melanoma Cian D’Arcy and Christina Kiel * Systems Biology Ireland & UCD Charles Institute of Dermatology, School of Medicine, University College Dublin, D04 V1W8 Dublin, Ireland; [email protected] * Correspondence: [email protected]; Tel.: +353-1-716-6344 Abstract: Cell adhesion molecules (CAMs) of the cadherin, integrin, immunoglobulin, and selectin protein families are indispensable for the formation and maintenance of multicellular tissues, espe- cially epithelia. In the epidermis, they are involved in cell–cell contacts and in cellular interactions with the extracellular matrix (ECM), thereby contributing to the structural integrity and barrier for- mation of the skin. Bulk and single cell RNA sequencing data show that >170 CAMs are expressed in the healthy human skin, with high expression levels in melanocytes, keratinocytes, endothelial, and smooth muscle cells. Alterations in expression levels of CAMs are involved in melanoma propagation, interaction with the microenvironment, and metastasis. Recent mechanistic analyses together with protein and gene expression data provide a better picture of the role of CAMs in the context of skin physiology and melanoma. Here, we review progress in the field and discuss molecular mechanisms in light of gene expression profiles, including recent single cell RNA expression information. We highlight key adhesion molecules in melanoma, which can guide the identification of pathways and Citation: D’Arcy, C.; Kiel, C. Cell strategies for novel anti-melanoma therapies. Adhesion Molecules in Normal Skin and Melanoma. Biomolecules 2021, 11, Keywords: cadherins; GTEx consortium; Human Protein Atlas; integrins; melanocytes; single cell 1213. https://doi.org/10.3390/ RNA sequencing; selectins; tumour microenvironment biom11081213 Academic Editor: Sang-Han Lee 1. -

Product Datasheet Integrin Beta 4/CD104 Antibody NB100
Product Datasheet Integrin beta 4/CD104 Antibody NB100-65599 Unit Size: 0.1 mg Store at 4C short term. Aliquot and store at -20C long term. Avoid freeze-thaw cycles. www.novusbio.com [email protected] Publications: 1 Protocols, Publications, Related Products, Reviews, Research Tools and Images at: www.novusbio.com/NB100-65599 Updated 6/15/2014 v.20.1 Page 1 of 3 v.20.1 Updated 6/15/2014 NB100-65599 Integrin beta 4/CD104 Antibody (450-9D) Product Information Unit Size 0.1 mg Concentration 1.0 mg/ml Storage Store at 4C short term. Aliquot and store at -20C long term. Avoid freeze-thaw cycles. Clonality Monoclonal Clone 450-9D Preservative 0.09% Sodium Azide Isotype IgG1 Purity Protein G purified Buffer PBS Product Description Host Mouse Gene ID 3691 Gene Symbol ITGB4 Species Human, Ferret, Mustelid Species Reactivity Cross reacts with Mustelid and Ferret. Specificity/Sensitivity NB100-65599 recognizes the human beta4 integrin (also known as CD104), a 205kD glycoprotein which associates with the alpha6 integrin to form the alpha6/beta4 complex. CD104 is expressed on epithelial cells, Schwann cells and various tumour cell lines. NB100-65599 recognizes an extracellular epitope on the CD104 molecule. Immunogen Purified alpha6 beta4 integrin from A431 cells Product Application Details Applications Western Blot, Flow Cytometry, Immunocytochemistry/Immunofluorescence, Immunohistochemistry, Immunohistochemistry-Frozen, Immunoprecipitation Recommended Dilutions Immunoprecipitation 1:10-1:500, Western Blot 1:100-1:2000, Immunohistochemistry-Frozen 1:500-1:1000, Flow Cytometry 1:25-1:100, Immunocytochemistry/Immunofluorescence 1:10-1:500, Immunohistochemistry 1:10-1:500 Application Notes For Flow Cytometry: Use 10 ul of the suggested working dilution to label 10^6 cells in 100 ul. -

Paracrine Signaling by Progesterone ⇑ Renuga Devi Rajaram, Cathrin Brisken
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Infoscience - École polytechnique fédérale de Lausanne Molecular and Cellular Endocrinology xxx (2011) xxx–xxx Contents lists available at SciVerse ScienceDirect Molecular and Cellular Endocrinology journal homepage: www.elsevier.com/locate/mce Review Paracrine signaling by progesterone ⇑ Renuga Devi Rajaram, Cathrin Brisken Ecole Polytechnique Fédérale de Lausanne (EPFL), ISREC – Swiss Institute for Experimental Cancer Research, NCCR Molecular Oncology, SV2832 Station 19, CH-1015 Lausanne, Switzerland article info abstract Article history: Steroid hormones coordinate and control the development and function of many organs and are impli- Available online xxxx cated in many pathological processes. Progesterone signaling, in particular, is essential for several impor- tant female reproductive functions. Physiological effects of progesterone are mediated by its cognate Keywords: receptor, expressed in a subset of cells in target tissues. Experimental evidence has accumulated that pro- Progesterone receptor gesterone acts through both cell intrinsic as well as paracrine signaling mechanisms. By relegating the Paracrine signaling hormonal stimulus to paracrine signaling cascades the systemic signal gets amplified locally and signal- Uterus ing reaches different cell types that are devoid of hormone receptors. Interestingly, distinct biological Ovaries responses to progesterone in different target tissues rely on several tissue-specific and some common Mammary gland Carcinogenesis paracrine factors that coordinate biological responses in different cell types. Evidence is forthcoming that the intercellular signaling pathways that control development and physiological functions are important in tumorigenesis. Crown Copyright Ó 2011 Published by Elsevier Ireland Ltd. All rights reserved. Contents 1. Introduction . ....................................................................................................... 00 2.