Preliminary Report Integrated Survey Dadu District, Sindh Province
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Weekly Field Epidemiology Report
Federal Disease Surveillance and Response Unit Field Epidemiology & Disease Surveillance Division National Institute of Health (NIH) Islamabad WEEKLY FIELD EPIDEMIOLOGY REPORT Volume 2 Issue 48 Nov 25 - Dec 01, 2019 Date: December 12, 2019 Provincial Technical Officers and fellows of FELTP PDSRUs/RDSRUs. In week 48 of 2019, no new case was assigned at the Disease Surveillance, Response Units reported. (DSRU’s) are working with provincial, and district health Diphtheria Surveillance: authorities on event based disease surveillance and During 2018 total 464 suspected cases of Diphtheria were outbreak response. reported. Total 544 cases reported in 2019 including 11 new DSRUs are sharing the disease surveillance data, case reported last week. outbreak reports and activities of FELTP fellows to the Dengue Surveillance: Federal Disease Surveillance and Response Unit In 2018 total 3204 Dengue cases were reported, from Sindh (FDSRU) at the Field Epidemiology and Disease (2088) while in 2019 total 24,336 cases have been reported Surveillance Division (FEDSD) National Institute of so far. In week 48, 2019, Punjab (62), KP (11), Baluchistan Health (NIH) Islamabad on weekly basis. (45), No report received from KP Merged Areas, ICT, KP, Sindh & AJK. Inside Issues Page No. CCHF Surveillance: Diphtheria /Dengue/ CCHF Surveillance 1 XDR/MDR-Typhoid Surveillance Karachi / In 2018 total 63 CCHF (suspected and confirmed) cases 1-5 Hyderabad Sindh were reported from DSRUs and 75 cases have been reported TVC campaign Sind and AEFI Surveillance 5-6 in 2019. -

PESA-DP-Hyderabad-Sindh.Pdf
Rani Bagh, Hyderabad “Disaster risk reduction has been a part of USAID’s work for decades. ……..we strive to do so in ways that better assess the threat of hazards, reduce losses, and ultimately protect and save more people during the next disaster.” Kasey Channell, Acting Director of the Disaster Response and Mitigation Division of USAID’s Office of U.S. Foreign Disas ter Ass istance (OFDA) PAKISTAN EMERGENCY SITUATIONAL ANALYSIS District Hyderabad August 2014 “Disasters can be seen as often as predictable events, requiring forward planning which is integrated in to broader de velopment programs.” Helen Clark, UNDP Administrator, Bureau of Crisis Preven on and Recovery. Annual Report 2011 Disclaimer iMMAP Pakistan is pleased to publish this district profile. The purpose of this profile is to promote public awareness, welfare, and safety while providing community and other related stakeholders, access to vital information for enhancing their disaster mitigation and response efforts. While iMMAP team has tried its best to provide proper source of information and ensure consistency in analyses within the given time limits; iMMAP shall not be held responsible for any inaccuracies that may be encountered. In any situation where the Official Public Records differs from the information provided in this district profile, the Official Public Records should take as precedence. iMMAP disclaims any responsibility and makes no representations or warranties as to the quality, accuracy, content, or completeness of any information contained in this report. Final assessment of accuracy and reliability of information is the responsibility of the user. iMMAP shall not be liable for damages of any nature whatsoever resulting from the use or misuse of information contained in this report. -

Acute Malnutrition Situation in Jamshoro, Tharparkar and Umerkot Districts in Sindh
Acute Malnutrition Situation in Jamshoro, Tharparkar and Umerkot Districts in Sindh Results of IPC Acute Malnutrition Analysis IPC Global Partners With the support of OBJECTIVES OF IPC ACUTE MALNUTRITION ANALYSIS IN SINDH . Classify the areas (Jamshoro, Umerkot and Tharparkar) based on the prevalence of acute malnutrition . Identify major contributing factors to acute malnutrition . Provide actionable knowledge by consolidating wide-ranging evidence on acute malnutrition and contributing factors for response planning METHODS AND PROCESS (1) • Globally, three scales of IPC classification are being used at present: . IPC for Acute Food Insecurity (IPC AFI), . IPC for Chronic Food Insecurity (IPC CFI) and . IPC for Acute Malnutrition (IPC AMN) • Outcome indicator for IPC AMN: GAM by WHZ (Weight for Height) or GAM by MUAC of children age 6-59 months • 5 phases in IPC AMN METHODS & PROCESSES (2) • The data on outcome indicator GAM (MUAC) was taken from Livelihood and Food Security Assessment (LFSA) conducted in April/May 2017. • For other indicators/contributing factors, – SMART nutrition surveys conducted by UNICEF and partners in the targeted districts, – LFSA, MICS, PSLM, and other national surveys were used as the main sources of information in the analysis. • Experts and analysts on nutrition, health and food security from Pakistan with the support from IPC Global (Rome) and Regional (Bangkok) team carried out the analysis • The experts were representatives of . Sindh Govt (Planning & Development Department, Nutrition Support Program, PDMA, Bureau of Statistics, Livestock Department); . Federal Government (Ministry of Planning, Development & Reform, Ministry of National Food Security & Research, Pakistan Agriculture Research Centre); . UN organizations (FAO, WFP, UNICEF, WHO); and . -

Pdf | 951.36 Kb
P a g e | 1 Operation Updates Report Pakistan: Monsoon Floods DREF n° MDRPK019 GLIDE n° FL-2020-000185-PAK Operation update n° 1; Date of issue: 6/10/2020 Timeframe covered by this update: 10/08/2020 – 07/09/2020 Operation start date: 10/08/2020 Operation timeframe: 6 months; End date: 28/02/2021 Funding requirements (CHF): DREF second allocation amount CHF 339,183 (Initial DREF CHF 259,466 - Total DREF budget CHF 598,649) N° of people being assisted: 96,250 (revised from the initially planned 68,250 people) Red Cross Red Crescent Movement partners currently actively involved in the operation: IFRC Pakistan Country Office is actively involved in the coordination and is supporting Pakistan Red Crescent Society (PRCS) in this operation. In addition, PRCS is maintaining close liaison with other in-country Movement partners: International Committee of the Red Cross (ICRC), German Red Cross (GRC), Norwegian Red Cross (NorCross) and Turkish Red Crescent Society (TRCS) – who are likely to support the National Society’s response. Other partner organizations actively involved in the operation: National Disaster Management Authority (NDMA), Provincial Disaster Management Authorities (PDMAs), District Administration, United Nations (UN) and local NGOs. Summary of major revisions made to emergency plan of action: Another round of continuous heavy rains started in most part of the country on the week of 20 August 2020 until 3 September 2020 intermittently. The second round of torrential rains caused urban flooding in the Sindh province and flash flooding in Khyber Pakhtunkhwa (KP). New areas have been affected by the urban flooding including the districts of Malir, Karachi Central, Karachi West, Karachi East and Korangi (Sindh), and District Shangla, Swat and Charsadda in Khyber Pakhtunkhwa. -

Organizational Presence in Union Councils of Sindh - ER - Floods 2011
Organizational presence in Union Councils of Sindh - ER - Floods 2011 Gilgit Baltistan China ! ! ! ! ! ! ! ! ! !! ! ! !! Khyber Pakhtun! khwa !! ! ! Azad Kashmi!r! Disputed Territory Afghanistan Fata ! 4 Punjab Tangwani Kashmore Thul Balochistan Kashmore India Jacobabad Jacobabad Iran Ubauro Kanhdkot Sindh Shikarpur Garhi Khairo Khanpur (Shikarpur) Ghotki Arabian sea Shahdadkot Shikarpur Qubo Saeed Khan Lakhi Daharki Garhi Yasin Pano Aqil Miro Khan Ghotki Ratodero Sukkur Mirpur Mathelo Kingri Qambar Shahdadkot Rohri Kambar Ali Khan Larkana Khairpur Khangarh Larkana Gambat Warah Bakrani Sukkur Kot Diji Salehpat Dokri Sobodhero Mehar Khairpur Nathan Shah Kandiaro Mirwah Ghulam Shah Bagrani Saeedpur Bhiria Naushahro Feroze Dadu Dadu Naushahro Feroze Faiz Ganj Khairpur Moro Nara Johi Kazi Ahmed Daur Shaheed Benazirabad Nawabshah Sehwan Sinjhoro Barhoon Sakrand Shahdadpur Sanghar Ashgarabad Sinjhoro Sindh Jaffar Khan Laghari Kurkali Jhatia Jhol Khipro Hala Manik ThaheemSyes Sughatullah Shaheed Manjhand Khori Tando Adam Sanghar Hatungo Matiari Jan Nawaz Ali Jamshoro Jhando Mari Matiari Dassori Khahi Mirabad Mirpur Khas Pithoro Thano Bula Khan Kotri Shadi pali Pithoro Saabho Qasimabad Tando Allah Yar Tando Allah Yar Umerkot Hyderabad City Hyderabad Sanjar Chang Dengan Dad Jarwar Samaro Umerkot Hyderabad Kot Ghulam Muhammad Latifabad MMirir pImuamr B uKx Hhadai Bsux Burgury padhario Tando Muhammad Khan Saeed Khan Lund Digri Chachro Matli Sufan Shah Kunri Mulakatyar Mir Khuda Buksh Saeed Matto Lakhat Tando Jan Mohammad Karachi City Thatta Malir -

Sindh Flood 2011 - Union Council Ranking - Tharparkar District
PAKISTAN - Sindh Flood 2011 - Union Council Ranking - Tharparkar District Union council ranking exercise, coordinated by UNOCHA and UNDP, is a joint effort of Government and humanitarian partners Community Restoration Food Education in the notified districts of 2011 floods in Sindh. Its purpose is to: SANGHAR SANGHAR SANGHAR Parno Gadro Parno Gadro Parno Gadro Identify high priority union councils with outstanding needs. Pirano Pirano Pirano Jo Par Jo Par Jo Par Facilitate stackholders to plan/support interventions and divert INDIA INDIA INDIA UMERKOT UMERKOT Tar Ahmed Tar Ahmed UMERKOT Tar Ahmed Mithrio Mithrio Mithrio resources where they are most needed. Charan Charan Charan MATIARI Sarianghiar MATIARI Sarianghiar MATIARI Sarianghiar Provide common prioritization framework to clusters, agencies Vejhiar Chachro Vejhiar Chachro Vejhiar Chachro Kantio Hirar Tardos Kantio Hirar Tardos Kantio Hirar Tardos Mithrio Mithrio Mithrio and donors. Chelhar Charan Chelhar Charan Chelhar Charan Satidero Satidero Satidero First round of this exercise is completed from February - March Mohrano Islamkot Mohrano Islamkot Mohrano Islamkot Mithrio Singaro Tingusar Mithrio Singaro Tingusar Mithrio Singaro Tingusar Bhitaro Bhatti Bhitaro Bhatti Bhitaro Bhatti BADIN Joruo BADIN Joruo BADIN Joruo 2012. Khario Harho Khario Harho Khario Harho Khetlari Ghulam Nagarparkar Khetlari Ghulam Nagarparkar Khetlari Ghulam Nagarparkar Shah Shah Shah Malanhori Mithi Malanhori Mithi Malanhori Mithi Virawah Virawah Virawah Sobhiar Vena Sobhiar Vena Sobhiar Vena Pithapur -

Population According to Religion, Tables-6, Pakistan
-No. 32A 11 I I ! I , 1 --.. ".._" I l <t I If _:ENSUS OF RAKISTAN, 1951 ( 1 - - I O .PUlA'TION ACC<!>R'DING TO RELIGIO ~ (TA~LE; 6)/ \ 1 \ \ ,I tin N~.2 1 • t ~ ~ I, . : - f I ~ (bFICE OF THE ~ENSU) ' COMMISSIO ~ ER; .1 :VERNMENT OF PAKISTAN, l .. October 1951 - ~........-.~ .1',l 1 RY OF THE INTERIOR, PI'ice Rs. 2 ~f 5. it '7 J . CH I. ~ CE.N TABLE 6.-RELIGION SECTION 6·1.-PAKISTAN Thousand personc:. ,Prorinces and States Total Muslim Caste Sch~duled Christian Others (Note 1) Hindu Caste Hindu ~ --- (l b c d e f g _-'--- --- ---- KISTAN 7,56,36 6,49,59 43,49 54,21 5,41 3,66 ;:histan and States 11,54 11,37 12 ] 4 listricts 6,02 5,94 3 1 4 States 5,52 5,43 9 ,: Bengal 4,19,32 3,22,27 41,87 50,52 1,07 3,59 aeral Capital Area, 11,23 10,78 5 13 21 6 Karachi. ·W. F. P. and Tribal 58,65 58,58 1 2 4 Areas. Districts 32,23 32,17 " 4 Agencies (Tribal Areas) 26,42 26,41 aIIjab and BahawaJpur 2,06,37 2,02,01 3 30 4,03 State. Districts 1,88,15 1,83,93 2 19 4,01 Bahawa1pur State 18,22 18,08 11 2 ';ind and Kbairpur State 49,25 44,58 1,41 3,23 2 1 Districts 46,06 41,49 1,34 3,20 2 Khairpur State 3,19 3,09 7 3 I.-Excluding 207 thousand persons claiming Nationalities other than Pakistani. -

Format for the Minutes of Monthly Review Meeting
MINUTES OF THE (10th ) MONTHLY REVIEW MEETING OF DISTRICT HYDERABAD Monthly Review Meeting (M.R.M) of District, Hyderabad for the Month of August, 2012 was held on 13.09.2012 at meeting Hall of Ex-Zila Nazim Office, Hyderabad. Written invitations to participate were sent to the Administrator/ DCO, the D.H.O, all Focal persons of Vertical Programs, District Population Officer i.e EPI, TB DOTS,MNCH, National Program, Malaria Control, Hepatitis, DHIS & DEWS, representatives WHO, all I/c Medical Officers/ FMOs/LHVs etc. List of Participants: S Sr. Names Designation Names Designation # 1. Mr. Mustafa Kamal Tagar DSM, PPHI 41 Dr. Shazia Zeeshan FMO 2. Dr. Ahmed Ali Talpur A: DHO 42 Dr. Anaila Soomro WMO 3. Dr. Qazi Rasheed Ahmed F.P, DHIS 43 Dr. Mumtaz Rajper FMO 4. Dr. Sono Khan Bhurgri T.H.O Hyd Rural 44 Dr. Neelofer Kazi FMO 5. Dr. M Ayoub Unar Dist: T.B Coor. 45 Dr. Rubina Sheikh SWMO 6. Dr. Naveed Ahmed Eye Specialist 46 Dr. Samira Tebani WMO 7. Dr. Shabum DDO 47 Dr. Yasir MO 8. Dr. Rafique Ahmed MO 48 Dr. Mehwish FMO 9. Dr. Ammnullah Ogahi SMO 49 Dr. Fareeda FMO 10. Dr. Azeem Shah SMO I/C 50 Dr. Shabnum Tunio FMO 11. Dr. A. Rahim Khatian SMO I/C 51 Dr. Liaquat Siyal MO 12. Dr. Raza Muhammad SMO I/C 52 Dr. Farzana Agha WMO 13. Dr. Muqadus Ali MO 53 Dr. Kapil Dev M O HQ 14. Dr. Khadim Hussain SMO / IC 54 Sanjar Kumar Asst. 15. Dr. Khalid Dawich MO I/C 55 Dr. -

Sindh Province - Flood Analysis (Flood Extent from 27 August 2010 to 07 September 2010)
Pakistan Floods: Sindh Province - Flood Analysis (Flood Extent from 27 August 2010 to 07 September 2010) Kashmore Taluka Thul Taluka Kashmore PUNJAB Jacobabad Taluka Kandhkot Taluka BALOCHISTAN Jaccobabad Ubauro Taluka Shikarpur Taluka Garhi Khairo Taluka Khanpur Taluka Ghotki Taluka Shikarpur Lakhi Taluka Garhi Yasin Taluka Shahdad Kot Taluka Pano Aqil Taluka Ghotki Daharki Taluka Miro Khan Taluka Sukkur Taluka Ratodero Taluka Kambar Ali Khan Taluka Mirpur Mathelo Taluka Kingri Taluka Rohri Taluka Qambar Shahdad kot Larkana Taluka Khairpur Taluka Khangarh Taluka Larkana Gambat Taluka Hamal Lake Warah Taluka Sukkur Dokri Taluka Kot Diji Taluka Salehpat Taluka Sobho Dero Taluka Mehar Taluka An estimated 7 million people are affected Khairpur Nathan Shah Taluka Kandiaro Taluka Mirwah Taluka 19 districts and 7,277 villages are affected. 1,098,720 houses are damaged Bhiria Taluka 199 deaths and 1,072 injuries are reported Naushahro Feroze (Source: NDMA, PDMA, GBDMA, FDMA as of 13092010) Dadu Khairpur Faiz Ganj Taluka Naushahro Feroze Taluka Dadu Taluka Moro Taluka Nara Taluka Johi Taluka Manchar Lake Daulat Pur Taluka Nawabshah Taluka Flood Water entered Jhanagar ! ! S.Banazirabad and Bajara towns as Manchar lake brusted as of 13 Sep 2010 Sehwan Taluka SINDH (UNOCHA Sit Rep # 24) Sakrand Taluka Shahdadpur Taluka Sanghar Taluka Water Supplies to Shewan tehsil I N D I A was cut down due to possible Sinjhoro Taluka contamination as of 13 Sep 2010 Sanghar Hala Taluka (UNOCHA Sit Rep # 24). Khipro Taluka Tando Adam Taluka Matiari Jam Nawaz -

District: UMAR KOT MERIT LIST of CANDIDATES APPLIED FOR
MBBS MERIT LIST OF CANDIDATES APPLIED FOR ADMISSION IN MBBS COURSE ACADEMIC SESSION 2020-2021 SESSION 2020-2021 AT GAMBAT MEDICAL COLLEGE, @ PIR ABDUL QADIR SHAH JEELANI INSTITUTE OF MEDICAL SCIENCES, GAMBAT District: UMAR KOT Int. Adj. Matric Matric O / Level Inter A / Level MDCAT Merit GIMS FILE Test ROLL MDCAT Test 40% 10% Name of Candidates Fathers Name Surname CNIC Gender District B B Test Total Score NO# NO. Obt Inter NUMBER 50% o Year Marks Total o Year Grade Marks Marks % Aa Aa 1 G-1482 Tooba Muneer Tarique Muneer Kahloon 4430333488214 F UMERKOT g2016 951 1100 g2020 938 85 A1 2402160 170 42.5 34.1091 8.6455 85.255 a a B B 2 G-1083 Manisha Kumari Vinesh Kumar Khatri 4440122391488 F UMERKOT I2018 745 850 I 2020 985 90 A1 2903411 149 37.25 35.8182 8.7647 81.833 S S M M 3 G-306 Harmat Singh Ghansham Das Sangrasi 4440122265385 M UMERKOT i2018 709 850 i 2020 980 89 A1 4900548 151 37.75 35.6364 8.3412 81.728 r r B B 4 G-91 KAMRAN ALI ABDUL AZIZ RAHIMOON 4440176905885 M UMERKOT I2017 698 850 I 2020 971 88 A1 3307849 152 38 35.3091 8.2118 81.521 S S B B 5 G-1277 JALAL DIN ABDULLAH KHAN PATHAN 4440411925627 M UMERKOT I2018 656 850 I 2020 960 87 A1 4900692 155 38.75 34.9091 7.7176 81.377 S S M M 6 G-300 Pardeep Kumar Mohan Lohana 4440392509487 M UMERKOT i2018 716 850 i 2020 995 90 A1 4900052 147 36.75 36.1818 8.4235 81.355 r r B B 7 G-327 Bashir Ahmed Sardar Ali Samejo 4440135929031 M UMERKOT I2018 655 850 I 2020 954 87 A1 2904607 155 38.75 34.6909 7.7059 81.147 S S B B 8 G-547 Suresh Kumar Rano Mal Meghwar 4440118625881 M UMERKOT I2018 672 -
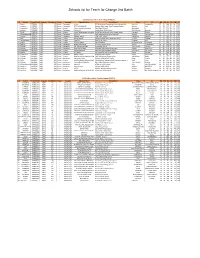
Schools List for Teach for Change 2Nd Batch
Schools list for Teach for Change 2nd Batch ESSP Schools List For Teach for Change (PHASE-II) S # District School Code Program Enrollment Phase Category Operator Name School Name Taluka UC ND NM NS ED EM ES 1 Sukkur ESSP0041 ESSP 435 Phase I Elementary Ali Bux REHMAN Model Computrized School Mubrak Pur. Pano Akil Mubarak Pur 27 40 288 69 19 729 2 Jamshoro ESSP0046 ESSP 363 Phase I Elementary RAZA MUHAMMAD Shaheed Rajib Anmol Free Education System Sehwan Arazi 26 28 132 67 47 667 3 Hyderabad ESSP0053 ESSP 450 Phase I Primary Free Journalist Foundation Zakia Model School Qasimabad 4 25 25 730 68 20 212 4 Khairpur ESSP0089 ESSP 476 Phase I Elementary Zulfiqar Ali Sachal Model Public School Thari Mirwah Kharirah 27 01 926 68 31 711 5 Ghotki ESSP0108 ESSP 491 Phase I Primary Lanjari Development foundation Sachal Sarmast model school dargahi arbani Khangarh Behtoor 27 49 553 69 20 705 6 ShaheedbenazirabaESSP0156 ESSP 201 Phase I Elementary Amir Bux Saath welfare public school (mashaik) Sakrand Gohram Mari 26 15 244 68 08 968 7 Khairpur ESSP0181 ESSP 294 Phase I Elementary Naseem Begum Faiza Public School Sobhodero Meerakh 27 15 283 68 20 911 8 Dadu ESSP0207 ESSP 338 Phase I Primary ghulam sarwar Danish Paradise New Elementary School Kn Shah Chandan 27 03 006 67 34 229 9 TandoAllahyar ESSP0306 ESSP 274 Phase I Primary Himat Ali New Vision School Chumber Jarki 25 24 009 68 49 275 10 Karachi ESSP0336 ESSP 303 Phase I Primary Kishwar Jabeen Mazin Academy Bin Qasim Twon Chowkandi 24 51 388 67 14 679 11 Sanghar ESSP0442 ESSP 589 Phase I Elementary -

Spatio-Temporal Flood Analysis Along the Indus River, Sindh, Punjab
p !( !( 23 August 2010 !( FL-2010-000141-PAK S p a t i o - Te m p o r a l F!( lo o d A n a l y s i s a l o n g t h e I n d u s R i v e r, S i n d h , P u n j a b , K P K a n d B a l o c h i s t a n P r o v i n c e s , P a k i s t a n p Version 1.0 !( This map shows daily variation in flo!(od water extent along the Indus rivers in Sindph, Punjab, Balochistan and KPK Index map CHINA p Crisis Satellite data : MODIS Terra / Aqua Map Scale for 1:1,000,000 Map prepared by: Supported by: provinces based on time-series MODIS Terra and Aqua datasets from August 17 to August 21, 2010. Resolution : 250m Legend 0 25 50 100 AFGHANISTAN !( Image date : August 18-22, 2010 Result show that the flood extent isq® continously increasing during the last 5 days as observed in Shahdad Kot Tehsil p Source : NASA Pre-Flood River Line (2009) Kilometres of Sindh and Balochistan provinces covering villages of Shahdad, Jamali, Rahoja, Silra. In the Punjab provinces flood has q® Airport p Pre-flood Image : MODIS Terra / Aqua Map layout designed for A1 Printing (36 x 24 inch) !( partially increased further in Shujabad Tehsil villages of Bajuwala Ti!(bba, Faizpur, Isanwali, Mulana)as. Over 1000 villages !( ® Resolution : 250m Flood Water extent (Aug 18) p and 100 towns were identified as severly affepcted by flood waters and vanalysis was performed using geospatial database ® Heliport !( Image date : September 19, 2009 !( v !( Flood Water extent (Aug 19) ! received from University of Georgia, google earth and GIS data of NIMA (USGS).