Confusion, Hyperactive Delirium, and Secondary Mania in Right Hemispheric Strokes: a Focused Review of Neuroanatomical Correlates David L
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Conflict, Arousal, and Logical Gut Feelings
CONFLICT, AROUSAL, AND LOGICAL GUT FEELINGS Wim De Neys1, 2, 3 1 ‐ CNRS, Unité 3521 LaPsyDÉ, France 2 ‐ Université Paris Descartes, Sorbonne Paris Cité, Unité 3521 LaPsyDÉ, France 3 ‐ Université de Caen Basse‐Normandie, Unité 3521 LaPsyDÉ, France Mailing address: Wim De Neys LaPsyDÉ (Unité CNRS 3521, Université Paris Descartes) Sorbonne - Labo A. Binet 46, rue Saint Jacques 75005 Paris France [email protected] ABSTRACT Although human reasoning is often biased by intuitive heuristics, recent studies on conflict detection during thinking suggest that adult reasoners detect the biased nature of their judgments. Despite their illogical response, adults seem to demonstrate a remarkable sensitivity to possible conflict between their heuristic judgment and logical or probabilistic norms. In this chapter I review the core findings and try to clarify why it makes sense to conceive this logical sensitivity as an intuitive gut feeling. CONFLICT, AROUSAL, AND LOGICAL GUT FEELINGS Imagine you’re on a game show. The host shows you two metal boxes that are both filled with $100 and $1 dollar bills. You get to draw one note out of one of the boxes. Whatever note you draw is yours to keep. The host tells you that box A contains a total of 10 bills, one of which is a $100 note. He also informs you that Box B contains 1000 bills and 99 of these are $100 notes. So box A has got one $100 bill in it while there are 99 of them hiding in box B. Which one of the boxes should you draw from to maximize your chances of winning $100? When presented with this problem a lot of people seem to have a strong intuitive preference for Box B. -

Panic Disorder Issue Brief
Panic Disorder OCTOBER | 2018 Introduction Briefings such as this one are prepared in response to petitions to add new conditions to the list of qualifying conditions for the Minnesota medical cannabis program. The intention of these briefings is to present to the Commissioner of Health, to members of the Medical Cannabis Review Panel, and to interested members of the public scientific studies of cannabis products as therapy for the petitioned condition. Brief information on the condition and its current treatment is provided to help give context to the studies. The primary focus is on clinical trials and observational studies, but for many conditions there are few of these. A selection of articles on pre-clinical studies (typically laboratory and animal model studies) will be included, especially if there are few clinical trials or observational studies. Though interpretation of surveys is usually difficult because it is unclear whether responders represent the population of interest and because of unknown validity of responses, when published in peer-reviewed journals surveys will be included for completeness. When found, published recommendations or opinions of national organizations medical organizations will be included. Searches for published clinical trials and observational studies are performed using the National Library of Medicine’s MEDLINE database using key words appropriate for the petitioned condition. Articles that appeared to be results of clinical trials, observational studies, or review articles of such studies, were accessed for examination. References in the articles were studied to identify additional articles that were not found on the initial search. This continued in an iterative fashion until no additional relevant articles were found. -

A Case of Steroid Induced Mania
Case Report International Journal of Psychiatry A Case of Steroid Induced Mania 1* 1 Maryam M Alnasser , Yasser M Alanzi and Amena H * 2 Corresponding author Alhemyari Maryam M Alnasse, MBBS from University of Dammam, Saudi Arabia, E-mail: [email protected]. 1 MBBS from University of Dammam, Saudi Arabia. Submitted: 14 Dec 2016; Accepted: 26 Dec 2016; Published: 30 Dec 2016 2MBBS from King Faisal University, Saudi Arabia. Abstract Background: Steroids have been widely used and prescribed for a variety of systemic diseases. Although they prove to be highly effective, they have many physical and psychiatric adverse effects. The systemic side effects of these medications are well known and well studied, in contrast to the psychiatric adverse effects which its phenomenology needs to be the focus of more clinical studies. However, the incidence of diagnosable psychiatric disorders due to steroid therapy is reported to be 3-6%. Affective reactions such as depression, mania, and hypomania are the most common adverse effects, along with psychosis, anxiety and delirium. Aim: We describe a case of corticosteroid induced mania, its unusual clinical picture, its course and management. Case description: A 14-year-old female intermediate school student, with a recent diagnosis of Chron’s disease was brought to A&E department due to acute behavioral disturbance in form of confusion, visual hallucinations, psychomotor agitation, irritability, hyperactivity, talkativeness, lack of sleep, and physical aggression. Those symptoms have started few days following corticosteroid therapy which was Prednisolone 40mg PO OD. And she was diagnosed with steroid induced mania. Discussion: This case illustrates the need for more understanding of the phenomenology and diversity of corticosteroids induced psychiatric syndromes. -

The ICD-10 Classification of Mental and Behavioural Disorders : Clinical Descriptions and Diagnostic Guidelines
ICD-10 ThelCD-10 Classification of Mental and Behavioural Disorders Clinical descriptions and diagnostic guidelines | World Health Organization I Geneva I 1992 Reprinted 1993, 1994, 1995, 1998, 2000, 2002, 2004 WHO Library Cataloguing in Publication Data The ICD-10 classification of mental and behavioural disorders : clinical descriptions and diagnostic guidelines. 1.Mental disorders — classification 2.Mental disorders — diagnosis ISBN 92 4 154422 8 (NLM Classification: WM 15) © World Health Organization 1992 All rights reserved. Publications of the World Health Organization can be obtained from Marketing and Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 2476; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications — whether for sale or for noncommercial distribution — should be addressed to Publications, at the above address (fax: +41 22 791 4806; email: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers' products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -
![Arxiv:2011.03588V1 [Cs.CL] 6 Nov 2020](https://docslib.b-cdn.net/cover/9395/arxiv-2011-03588v1-cs-cl-6-nov-2020-1219395.webp)
Arxiv:2011.03588V1 [Cs.CL] 6 Nov 2020
Hostility Detection Dataset in Hindi Mohit Bhardwajy, Md Shad Akhtary, Asif Ekbalz, Amitava Das?, Tanmoy Chakrabortyy yIIIT Delhi, India. zIIT Patna, India. ?Wipro Research, India. fmohit19014,tanmoy,[email protected], [email protected], [email protected] Abstract Despite Hindi being the third most spoken language in the world, and a significant presence of Hindi content on social In this paper, we present a novel hostility detection dataset in Hindi language. We collect and manually annotate ∼ 8200 media platforms, to our surprise, we were not able to find online posts. The annotated dataset covers four hostility di- any significant dataset on fake news or hate speech detec- mensions: fake news, hate speech, offensive, and defamation tion in Hindi. A survey of the literature suggest a few works posts, along with a non-hostile label. The hostile posts are related to hostile post detection in Hindi, such as (Kar et al. also considered for multi-label tags due to a significant over- 2020; Jha et al. 2020; Safi Samghabadi et al. 2020); however, lap among the hostile classes. We release this dataset as part there are two basic issues with these works - either the num- of the CONSTRAINT-2021 shared task on hostile post detec- ber of samples in the dataset are not adequate or they cater tion. to a specific dimension of the hostility only. In this paper, we present our manually annotated dataset for hostile posts 1 Introduction detection in Hindi. We collect more than ∼ 8200 online so- The COVID-19 pandemic has changed our lives forever, cial media posts and annotate them as hostile and non-hostile both online and offline. -

The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic Criteria for Research
The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic criteria for research World Health Organization Geneva The World Health Organization is a specialized agency of the United Nations with primary responsibility for international health matters and public health. Through this organization, which was created in 1948, the health professions of some 180 countries exchange their knowledge and experience with the aim of making possible the attainment by all citizens of the world by the year 2000 of a level of health that will permit them to lead a socially and economically productive life. By means of direct technical cooperation with its Member States, and by stimulating such cooperation among them, WHO promotes the development of comprehensive health services, the prevention and control of diseases, the improvement of environmental conditions, the development of human resources for health, the coordination and development of biomedical and health services research, and the planning and implementation of health programmes. These broad fields of endeavour encompass a wide variety of activities, such as developing systems of primary health care that reach the whole population of Member countries; promoting the health of mothers and children; combating malnutrition; controlling malaria and other communicable diseases including tuberculosis and leprosy; coordinating the global strategy for the prevention and control of AIDS; having achieved the eradication of smallpox, promoting mass immunization against a number of other -
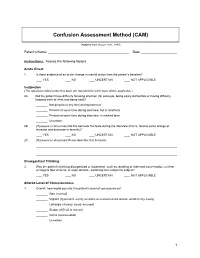
Confusion Assessment Method (CAM)
Confusion Assessment Method (CAM) (Adapted from Inouye et al., 1990) Patient’s Name: Date: Instructions: Assess the following factors. Acute Onset 1. Is there evidence of an acute change in mental status from the patient’s baseline? YES NO UNCERTAIN NOT APPLICABLE Inattention (The questions listed under this topic are repeated for each topic where applicable.) 2A. Did the patient have difficulty focusing attention (for example, being easily distractible or having difficulty keeping track of what was being said)? Not present at any time during interview Present at some time during interview, but in mild form Present at some time during interview, in marked form Uncertain 2B. (If present or abnormal) Did this behavior fluctuate during the interview (that is, tend to come and go or increase and decrease in severity)? YES NO UNCERTAIN NOT APPLICABLE 2C. (If present or abnormal) Please describe this behavior. Disorganized Thinking 3. Was the patient’s thinking disorganized or incoherent, such as rambling or irrelevant conversation, unclear or illogical flow of ideas, or unpredictable, switching from subject to subject? YES NO UNCERTAIN NOT APPLICABLE Altered Level of Consciousness 4. Overall, how would you rate this patient’s level of consciousness? Alert (normal) Vigilant (hyperalert, overly sensitive to environmental stimuli, startled very easily) Lethargic (drowsy, easily aroused) Stupor (difficult to arouse) Coma (unarousable) Uncertain 1 Disorientation 5. Was the patient disoriented at any time during the interview, such as thinking that he or she was somewhere other than the hospital, using the wrong bed, or misjudging the time of day? YES NO UNCERTAIN NOT APPLICABLE Memory Impairment 6. -

Lamotrigine As a Treatment of Agitation in Dementia F
Lamotrigine as a treatment of agitation in Dementia F. Godinho1, A. Valverde2. 1Hospital Espirito Santo de Évora, Department of Psychiatry and Mental Health, Évora, Portugal. 2Hospital Professor Doutor Fernando da Fonseca, Neurology Service, Amadora, Portugal. Background: • Psychomotor agitation is common in patients with dementia but there are no well-established or evidenced-based effective treatments. • Non-pharmacological interventions remain the mainstay of treatment but are not always feasible or sufficient. • Antipsychotic are the most commonly used drugs but concerns regarding tolerability limit their use. • Anticonvulsants are receiving growing attention due to their better safety profile. Objective: Methods: We report a case of a patient with dementia and behavioral disturbance Retrospective review of the clinical chart and literature review on the treated with lamotrigine, and make a brief review of the literature of topic. anticonvulsants use in the treatment of agitation and aggression in dementia. RESULTS Clinical case • A 69 years-old woman with behavioral variant Frontotemporal Dementia, severe stage, totally dependent on activities of daily living and with severe speech difficulties, developed progressive aggressive behavior. • In the following 6 months, quetiapine until 200mg/daily and then risperidone until 1mg/daily was tried, with no success. • Lamotrigine was then introduced and titrated until 100mg/daily. • Since this dosage and in the 2 next consultations, no more aggressive behavior were observed Literature Review -

RELATIONAL EMPATHY 1 Running Head
RELATIONAL EMPATHY 1 Running head: RELATIONAL EMPATHY The Interpersonal Functions of Empathy: A Relational Perspective Alexandra Main, Eric A. Walle, Carmen Kho, & Jodi Halpern Alexandra Main Carmen Kho University of California, Merced University of California, Merced 5200 N Lake Road 5200 N Lake Road Merced, CA 95343 Merced, CA 95343 Phone: 209-228-2429 Phone: 714-253-6163 Email: [email protected] Email: [email protected] Eric A. Walle Jodi Halpern University of California, Merced University of California, Berkeley 5200 N Lake Road 570 University Hall Merced, CA 95343 Berkeley, CA 94720 Phone: 209-228-4634 Phone: 510-642-4366 Email: [email protected] Email: [email protected] Correspondence concerning this article should be addressed to Alexandra Main, Psychological Sciences, 5200 North Lake Road, University of California, Merced, CA 95343. Phone: 209-228-2429, Email: [email protected] RELATIONAL EMPATHY 2 Abstract Empathy is an extensively studied construct, but operationalization of effective empathy is routinely debated in popular culture, theory, and empirical research. This paper offers a process-focused approach emphasizing the relational functions of empathy in interpersonal contexts. We argue that this perspective offers advantages over more traditional conceptualizations that focus on primarily intrapsychic features (i.e., within the individual). Our aim is to enrich current conceptualizations and empirical approaches to the study of empathy by drawing on psychological, philosophical, medical, linguistic, and anthropological perspectives. In doing so, we highlight the various functions of empathy in social interaction, underscore some underemphasized components in empirical studies of empathy, and make recommendations for future research on this important area in the study of emotion. -

Does Psychomotor Agitation in Major Depressive Episodes Indicate Bipolarity? Evidence from the Zurich Study
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by RERO DOC Digital Library Eur Arch Psychiatry Clin Neurosci (2009) 259:55–63 DOI 10.1007/s00406-008-0834-7 ORIGINAL PAPER Jules Angst Æ Alex Gamma Æ Franco Benazzi Æ Vladeta Ajdacic Æ Wulf Ro¨ssler Does psychomotor agitation in major depressive episodes indicate bipolarity? Evidence from the Zurich Study Received: 4 September 2007 / Accepted: 5 June 2008 / Published online: 19 September 2008 j Abstract Background Kraepelin’s partial interpre- were equally associated with the indicators of bipolarity tation of agitated depression as a mixed state of and with anxiety. Longitudinally, agitation and retar- ‘‘manic-depressive insanity’’ (including the current dation were significantly associated with each other concept of bipolar disorder) has recently been the focus (OR = 1.8, 95% CI = 1.0–3.2), and this combined of much research. This paper tested whether, how, and group of major depressives showed stronger associa- to what extent both psychomotor symptoms, agitation tions with bipolarity, with both hypomanic/cyclothy- and retardation in depression are related to bipolarity mic and depressive temperamental traits, and with and anxiety. Method The prospective Zurich Study anxiety. Among agitated, non-retarded depressives, assessed psychiatric and somatic syndromes in a unipolar mood disorder was even twice as common as community sample of young adults (N = 591) (aged bipolar mood disorder. Conclusion Combined agitated 20 at first interview) by six interviews over 20 years and retarded major depressive states are more often (1979–1999). Psychomotor symptoms of agitation and bipolar than unipolar, but, in general, agitated retardation were assessed by professional interviewers depression (with or without retardation) is not more from age 22 to 40 (five interviews) on the basis of the frequently bipolar than retarded depression (with or observed and reported behaviour within the interview without agitation), and pure agitated depression is even section on depression. -
Preliminary Evidence on the Somatic Marker Hypothesis Applied to Investment Choices
Preliminary evidence on the Somatic Marker Hypothesis applied to investment choices Article Accepted Version Cantarella, S., Hillenbrand, C., Aldridge-Waddon, L. and Puzzo, I. (2018) Preliminary evidence on the Somatic Marker Hypothesis applied to investment choices. Journal of Neuroscience, Psychology, and Economics, 11 (4). pp. 228- 238. ISSN 1937-321X doi: https://doi.org/10.1037/npe0000097 Available at http://centaur.reading.ac.uk/80454/ It is advisable to refer to the publisher’s version if you intend to cite from the work. See Guidance on citing . To link to this article DOI: http://dx.doi.org/10.1037/npe0000097 Publisher: American Psychological Association All outputs in CentAUR are protected by Intellectual Property Rights law, including copyright law. Copyright and IPR is retained by the creators or other copyright holders. Terms and conditions for use of this material are defined in the End User Agreement . www.reading.ac.uk/centaur CentAUR Central Archive at the University of Reading Reading’s research outputs online The SMH in Investment Choices Preliminary evidence on the Somatic Marker Hypothesis applied to investment choices Simona Cantarella and Carola Hillenbrand University of Reading Luke Aldridge-Waddon University of Bath Ignazio Puzzo City University of London Words count: 5058 Figures: 5 Tables: 1 Manuscript accepted on the 06/08/2018 1 The SMH in Investment Choices Abstract The somatic marker hypothesis (SMH) is one of the more dominant physiological models of human decision making and yet is seldom applied to decision making in financial investment scenarios. This study provides preliminary evidence about the application of the SMH in investment choices using heart rate (HR) and skin conductance response (SCRs) measures. -

Identifying and Treating Postpartum Depression June Andrews Horowitz and Janice H
CLINICAL ISSUES Identifying and Treating Postpartum Depression June Andrews Horowitz and Janice H. Goodman Postpartum depression affects 10% to 20% of Despite adverse health consequences, systematic women in the United States and negatively influences PPD screening is not standard clinical practice in the maternal, infant, and family health. Assessment of risk United States. Limited availability of psychiatric factors and depression symptoms is needed to identi- services impedes referral for evaluation and treat- fy women at risk for postpartum depression for early ment. Nurses require knowledge about the nature referral and treatment. Individual and group psy- and efficacy of PPD treatments to refer their clients chotherapy have demonstrated efficacy as treatments, and recommend psychiatric services with confi- and some complementary/alternative therapies show dence. To inform nursing practice, this article promise. Treatment considerations include severity of describes PPD, examines screening approaches, and depression, whether a mother is breastfeeding, and synthesizes the literature concerning evidence-based mother’s preference. Nurses who work with childbear- treatments for PPD. ing women can advise depressed mothers regarding treatment options, make appropriate recommenda- Overview of Postpartum Depression tions, provide timely and accessible referrals, and encourage engagement in treatment. JOGNN, 34, 264–273; 2005. DOI: 10.1177/0884217505274583 Description, Prevalence, and Course Keywords: Mental health—Postpartum depres- Symptoms