South Wales Trauma Network, Serving South Wales, South Powys and West Wales Frequently Asked Questions General Information and Structure of the Network
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Cwm Taf Morgannwg University Health Board Job Description
CWM TAF MORGANNWG UNIVERSITY HEALTH BOARD JOB DESCRIPTION POST: Consultant Physician in Geriatric & General Medicine SALARY: £72,927 - £94,679 per annum DIRECTORATE: Medicine and A&E BASE: Royal Glamorgan Hospital The post holder will also be required to provide services at other hospital sites. Introduction This is a new post, which is being created to develop and improve the Geriatric Medicine services in Cwm Taf Morgannwg University Health Board. The post will be subject to the terms and conditions of service governing the appointment of Medical and Dental Staff in Wales, and to the Health Board's terms and conditions as appropriate. The candidate to be appointed will be required to be fully registered with the General Medical Council, to hold, or to be within 6 months of gaining, a Certificate of Completion of Training in both Geriatric Medicine and General Internal Medicine, and to be on the Specialist Register. The post holder will be joining a dynamic, forward looking and innovative Geriatric Medicine team. The post holder will be based at Royal Glamorgan Hospital in Llantrisant, where the Health Board has acute hospital beds covering a range of medical and surgical specialities. The post holder will be expected to help and develop Geriatric Medicine services provided by the Health Board at the Royal Glamorgan Hospital and in the community setting. A sub-speciality interest will be encouraged but there is flexibility to support personal development in this regard. Key to the development of services will be to develop clinical relationships with the colleagues in the Directorate and Local Health Board as well as strengthening working relationships with Primary Care colleagues in order to develop services locally. -
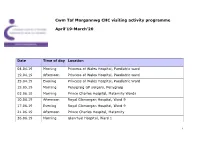
Cwm Taf Morgannwg CHC Visiting Activity Programme April'19-March'20
Cwm Taf Morgannwg CHC visiting activity programme April’19-March’20 Date Time of day Location 04.04.19 Morning Princess of Wales Hospital, Paediatric ward 19.04.19 Afternoon Princess of Wales Hospital, Paediatric ward 25.04.19 Evening Princess of Wales Hospital, Paediatric Ward 15.05.19 Morning Penygraig GP surgery, Penygraig 03.06.19 Morning Prince Charles Hospital, Maternity Wards 10.06.19 Afternoon Royal Glamorgan Hospital, Ward 9 17.06.19 Evening Royal Glamorgan Hospital, Ward 9 21.06.19 Afternoon Prince Charles Hospital, Maternity 26.06.19 Morning Glanrhyd Hospital, Ward 1 1 Date Time of day Location 27.06.19 Afternoon Glanrhyd Hospital, Ward 1 03.07.19 Morning Ysbyty Cwm Rhondda, Ward A1 04.07.19 Afternoon Prince Charles Hospital, Maternity Wards 11.07.19 Morning Royal Glamorgan Hospital, Ward 6 16.07.19 Afternoon Princess of Wales Hospital, Acute Medical Assessment Unit 22.07.19 Morning Princess of Wales Hospital, Acute Medical Assessment Unit 22.07.19 Evening Royal Glamorgan Hospital, Ward 6 24.07.19 Afternoon Ysbyty Cwm Rhondda, Ward A1 05.08.19 Afternoon Prince Charles Hospital, Ward 4 07.08.19 Morning Royal Glamorgan Hospital, Ward 14 14.08.19 Morning Prince Charles Hospital, Ward 4 14.08.19 Afternoon Royal Glamorgan Hospital, Ward 14 19.08.19 Evening Royal Glamorgan Hospital, Ward 14 21.08.19 Evening Prince Charles Hospital, Ward 4 18.09.19 Afternoon Prince Charles Hospital, Maternity Unit 19.09.19 Morning Royal Glamorgan Hospital, Maternity Unit 2 Date Time of day Location 04.12.19 Afternoon Ysbyty Cwm Rhondda, Ward D4 09.12.19 -

Hospital Name Country Location
Hospital Name Country Location 1 Tameside Hospital NHS Foundation Trust England Ashton-under-Lyne 2 Barnsley Hospital NHS Foundation Trust England Barnsley 3 Royal National Hospital for Rheumatic Diseases England Bath 4 Royal United Hospitals Bath NHS Foundation Trust England Bath 5 Bedford Hospital NHS Trust England Bedford 6 South Central Ambulance Service NHS Foundation Trust England Bicester 7 Wirral Community NHS Trust England Birkenhead 8 Birmingham Children's Hospital NHS Foundation Trust England Birmingham 9 Heart Of England NHS Foundation Trust England Birmingham 10 Sandwell and West Birmingham Hospitals NHS Trust England Birmingham 11 University Hospital Birmingham NHS Foundation Trust England Birmingham 12 Birmingham and Solihull Mental Health NHS Foundation Trust England Birmingham 13 Birmingham Community Healthcare NHS Foundation Trust England Birmingham 14 Birmingham Women's NHS Foundation Trust England Birmingham 15 The Royal Orthopaedic Hospital NHS Foundation Trust England Birmingham 16 Blackpool Teaching Hospitals NHS Foundation Trust England Blackpool 17 Bolton NHS Foundation Trust England Bolton 18 The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust England Bournmouth 19 Poole Hospital NHS Foundation Trust England Bournmouth 20 Bradford Teaching Hospitals NHS Foundation Trust England Bradford 21 Bradford District NHS Foundation Trust England Bradford 22 South East Coast Ambulance Service NHS Foundation Trust England Bridgwater 23 Sussex Community NHS Foundation Trust England Brighton 24 Brighton and -
The Future of Stroke Care in Wales Report of the Inquiry Into the Implementation of the Welsh Government’S Stroke Delivery Plan
Cross Party Group on Stroke The Future of Stroke Care in Wales Report of the inquiry into the implementation of the Welsh Government’s Stroke Delivery Plan March 2020 The Cross Party Contents Group on Stroke The following Assembly Members are members of the Cross Party Group Foreword 4 on Stroke: • Dr Dai Lloyd AM (Chair) Executive summary 6 • Neil Hamilton AM • Huw Irranca-Davies AM Background 8 • Adam Price AM • Nick Ramsay AM About the inquiry 9 The Cross Party Group on Stroke is facilitated by the Stroke Association, Preventing stroke 11 which compiled this report. The Cross Party Group on Stroke would like Fast and effective acute care 18 to thank all those individuals and organisations who took part in the inquiry, particularly those who gave Life after stroke 28 either oral or written evidence. A full list of those who provided evidence can be The stroke workforce 37 found in Appendix Two. The Cross Party Group on Stroke The future of the Stroke Delivery Plan 43 can be contacted on [email protected] Appendix one: Full list of recommendations 48 Appendix two: Organisations who provided evidence 50 Foreword My fellow members and I are pleased to present the final report of the Cross A new, strengthened model of delivery and accountability accompanied by the Party Group’s inquiry into the implementation of the Welsh Government’s Stroke highest quality hyperacute stroke units would enable the other challenges set out in Delivery Plan. this report to be overcome, such as attracting the best possible staff to deliver vital rehabilitation and game-changing treatment such as thrombectomy. -

Hospitals in Wales Thank You for Your Request Which I Re
Ein cyf/Our ref: ATISN 12891 22 January 2019 Dear , ATISN 12891 – Hospitals in Wales Thank you for your request which I received on 14 January 2019. You asked for the following information: A list of Welsh Hospitals per trust. The information you requested is attached in annex A. If you are dissatisfied with the Welsh Government’s handling of your request, you can ask for an internal review within 40 working days of the date of this response. Requests for an internal review should be addressed to the Welsh Government’s Freedom of Information Officer at: Information Rights Unit, Welsh Government, Cathays Park, Cardiff, CF10 3NQ or Email: [email protected] Please remember to quote the ATISN reference number above. You also have the right to complain to the Information Commissioner. However, please note the Commissioner will not normally investigate a complaint until it has been through our own internal review process. The Information Commissioner can be contacted at: Grŵp Iechyd a Gwasanaethau Cymdeithasol Health and Social Services Group E-bost E-mail: Parc Cathays Cathays Park [email protected] Caerdydd Cardiff CF10 3NQ Rydym yn croesawu derbyn gohebiaeth yn Gymraeg. Byddwn yn ateb gohebiaeth a dderbynnir yn Gymraeg yn Gymraeg ac ni fydd gohebu yn Gymraeg yn arwain at oedi. We welcome receiving correspondence in Welsh. Any correspondence received in Welsh will be answered in Welsh and corresponding in Welsh will not lead to a delay in responding. Information Commissioner’s Office, Wycliffe House, Water Lane, Wilmslow, Cheshire, SK9 5AF The request you sent me contains personal information about you – for example, your name and address. -

Carers A-Z Guide Cwm Taf Carers A-Z Guide
Cwm Taf Carers A-Z Guide Welcome from Cwm Taf Carers Champions Carers play a vital role in the provision of care, making an enormous contribution to supporting their loved ones in the community. They spend a great deal of their own valuable time and energy caring for vulnerable people and we are committed to ensuring that they are supported in this endeavour. We hope that this A-Z Guide, produced jointly by Merthyr Tydfil and Rhondda Cynon Taf Councils and Cwm Taf University Health Board in a response to the Carers Strategies (Wales) Measure, will help to achieve better outcomes for all by providing a central resource of up to date information about support services that are targeted to meet the needs of carers and other residents living in the Cwm Taf area. Councillor Bill Smith Carers Champion - Merthyr Tydfil CBC Councillor Mike Forey Carers Champion - Rhondda Cynon Taf CBC Independent Board Member Maria Thomas Carers Champion - Cwm Taf Local Health Board Cwm Taf Carers A-Z Guide Introduction This is the second edition of the Cwm Taf Carers Guide. It was originally formed by merging information from Merthyr and RCT’s Carers guides and has been produced to provide you with the information you may need to get the support necessary to help you to meet your caring responsibilities effectively. The useful contacts are listed alphabetically under the following headings to help you to find the specific information you require as easily as possible. We hope that the publication proves to be useful and helps you to better understand the services available locally and how to access them. -
Course Manual O P E N
DOCTORSDOCTORS ACADEMY ACADissemin ating DEMYMedical Knowl edge an d Skills Globally Disseminating Medical Knowledge and Skills Globally 6th Laparoscopic Colorectal Surgery Course & Master Class Dates: 7th and 8th May 2014 Venue: Prince Charles Hospital, Merthyr Tydfil, Wales Course Manual O P E N This course is accredited by the Royal College of Surgeons of Edinburgh. Attendance in this course entitles the delegate to receive 12 CPD points. Doctors Academy Publications Laparoscopic Colorectal Surgery Course & Master Class Prince Charles Hospital, Merthyr Tydfil, Wales Contents Welcome letter 3 Faculty & Orga nise r list 4 Faculty Profiles 5 About the Hospital 6 Course Programme 7 Selected Reading Material and Relevant Publications Steps for Laparoscopic Anterior Resection of Rectum 10 Steps for Laparoscopic Right hemicolectomy 11 The Merthyr Coaching Tool for Laparoscopic Colorectal Surgery 12 Preceptorship Programme 16 Laparoscopic Colorectal Surgery Training and Research - PC H contrib utions 17 Publications 18 Notes 22 Course dinner 24 Acknowledgement 25 Course Manual www.doctorsacademy.org Doctors Academy Publications Laparoscopic Colorectal Surgery Course & Master Class 33 Prince Charles Hospital, Merthyr Tydfil, Wales Welcome Dear Delegate, I am pleased to welcome you to the 6th Laparoscopic Colorectal Course & Masterclass at Prince Charles Hospital in Merthyr Tydfil. The course, started in 2010, is aimed at surgical trainees as well as consultants wishing to gain expertise in this field and has been very popular and very well received in previous years. Consequent upon its success, the course is now run biannually. The course is accredited by the Royal College of Surgeons of Edinburgh and the college awards 12 CPD points for attendance. -

THE NHS ESTATE in WALES Estate Condition and Performance Report the NHS ESTATE in WALES
2010/11 THE NHS ESTATE IN WALES Estate Condition and Performance Report THE NHS ESTATE IN WALES Estate Condition and Performance Report 2010/11 CONTENTS 1 INTRODUCTION 5-7 1.1 Background of the report 1.2 Purpose,format and scope of the report 1.3 Changes to the content of the report 1.4 Report validation 1.5 2010/11 Facilities Performance Report 2 EXECUTIVE SUMMARY 8-14 3 ESTATE PROFILE 15-19 3.1 Key statistics of the NHS estate in Wales 3.2 The age of the estate 3.3 The essential and non-essential estate 3.4 Expenditure on the NHS estate 44 E EstateSTATE PerformancePERFORMANCE 7 - 20 20-31 4.1 General information 4.2 Physical condition 4.3 Statutory and safety compliance 4.4 Functional suitability 4.5 Space utilisation 4.6 Energy performance 55 E EnvironmentalNVIRONMENTAL Issues 20 - 23ISSUES 32-38 5.1 Waste 5.2 Transport 5.3 Water usage 66 A SummaryPPENDICES 24 - 25 39-110 Appendix I Health Board/Trust Risk Adjusted Backlog Costs Appendices II-X Summary of Health Board/Trust information Appendix XI Details of non-essential Health Board/Trust property Appendix XII Performance Indicators and Targets 1 INTRODUCTION 1.1 Background of the report 1.1.1 This is the 10th Estate Condition and Performance Report published by NHS Wales Shared Services Partnership – Facilities Services (NWSSP-FS) and its predecessor organisation,Welsh Health Estates. 1.1.2 The report is based on annual estate data returns submitted to the on-line Estates and Facilities Performance Management System (EFPMS) by seven Health Boards,Velindre NHS Trust and the Welsh Ambulance Services NHS Trust,and cove rs the period from April 2010 to March 2011. -

Estates and Facilities Performance Breakdown
CWM TAF UNIVERSITY HEALTH BOARD Estates and Facilities Performance Breakdown 2017/2018 Key Performance Indicators Percentage of the estate which is of reasonable standard (falls within Estatecode category 'B'/'F') Statutory Health Net Energy Physical Condition Fire Safety Functionally Space utilisation COEmissions * Site Name and Safety Consumption (%) compliance (%) suitable (%) (%) (kg/m²) compliance (%) (kWh/m²) AGGREGATED SITE 87 100 69 98 97 374 80 PINEWOOD HOUSE 86 97 92 92 100 247 58 PONTYPRIDD & DISTRICT HOSPITAL 72 89 77 100 100 333 73 PRINCE CHARLES HOSPITAL 89 72 77 93 99 424 106 ROYAL GLAMORGAN HOSPITAL 81 100 98 99 94 451 110 YSBYTY CWM CYNON 100 98 100 100 98 309 58 YSBYTY CWM RHONDDA 68 89 100 98 98 332 58 YSBYTY GEORGE THOMAS 68 89 100 100 100 374 82 Health Board Average 85 90 85 97 97 406 95 *Target to be agreed Backlog Maintenance Costs Risk High Risk Significant Moderate Low Risks Site Name Adjusted (£) Risks (£) Risks (£) (£) Cost (£) AGGREGATED SITE 5,855 185,656 2,611,465 199,418 213,317 PINEWOOD HOUSE 0 1,739 105,577 9,149 5,563 PONTYPRIDD & DISTRICT HOSPITAL 53,732 267,550 12,277 0 321,691 PRINCE CHARLES HOSPITAL 0 19,320 2,708,027 6,074 109,790 ROYAL GLAMORGAN HOSPITAL 0 4,530,064 3,028,297 478,402 4,646,954 YSBYTY CWM CYNON 0 11,593 0 0 11,593 YSBYTY CWM RHONDDA 0 1,160 767,852 219,472 34,071 YSBYTY GEORGE THOMAS 0 169,696 551,635 11,941 188,481 Health Board Total 59,587 5,186,778 9,785,130 924,456 5,531,460 Energy Net Energy Carbon Emissions Energy Costs Net Hospital Site PI Energy Change COEmissions COper sq. -

Gp out of Hours Service
GP OUT OF HOURS SERVICE GP OUT-OF-HOURS SERVICE The GP Out of Hours (OOHs) service operates between the hours of: • 6.30pm and 8.00am Monday Friday • 6.30pm on Friday evening until 8.00am on Monday morning • Plus all bank holidays The GP Out of Hours service receives high levels of patient demand with more than 60,000 patients being seen each year GP OUT OF-HOURS SERVICE There are four primary care centres where patients with urgent medical problems can be seen Prince Charles Hospital Royal Glamorgan Hospital Ysbyty Cwm Rhondda Ysbyty Cwm Cynon Mobile doctors undertake home visits – mostly to patients in nursing homes, housebound and palliative care patients. A summary of the patient’s contact with the service is sent to the patients registered GP by 8am the following morning GP OUT-OF-HOURS SERVICE The GPs who deliver the service are all sessional and self employed The service fills more than 85 shifts per week The service requires more than 22,000 hours of GP time per year GP SHIFTS IN YSBYTY CWM RHONDDA TOTAL GP NUMBER MONTH % UNFILLED SHIFTS UNFILLED April 2015 30 9 30% May 2015 31 10 32% June 2015 30 7 23% NO OF PATIENTS SEEN AT PRIMARY CARE CENTRES ROYAL YSBYTY CWM MONTH GLAMORGAN RHONDDA HOSPITAL April 2015 1,008 208 May 2015 1,123 278 June 2015 947 184 GP OUT-OF-HOURS SERVICE Challenges: Cwm Taf’s GP Out-of-Hours service is finding it increasingly difficult to recruit sufficient GPs to deliver the service. The GP Out-of-Hours recruitment challenge is not unique to Cwm Taf as other Out-of- Hours services across Wales and the UK have similar experiences. -
Paper 1: Cwm Taf Morgannwg University Health Board , Item 2
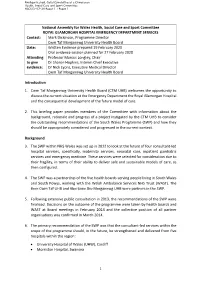
Pwyllgor Iechyd, Gofal Cymdeithasol a Chwaraeon Health, Social Care and Sport Committee HSCS(5)-07-20 Papur 1 / Paper 1 National Assembly for Wales Health, Social Care and Sport Committee ROYAL GLAMORGAN HOSPITAL EMERGENCY DEPARTMENT SERVICES Contact: Mark Dickinson, Programme Director Cwm Taf Morgannwg University Health Board Date: Written Evidence prepared 19 February 2020 Oral evidence session planned for 27 February 2020 Attending Professor Marcus Longley, Chair to give Dr Sharon Hopkins, Interim Chief Executive evidence: Dr Nick Lyons, Executive Medical Director Cwm Taf Morgannwg University Health Board Introduction 1. Cwm Taf Morgannwg University Health Board (CTM UHB) welcomes the opportunity to discuss the current situation at the Emergency Department the Royal Glamorgan Hospital and the consequential development of the future model of care. 2. This briefing paper provides members of the Committee with information about the background, rationale and progress of a project instigated by the CTM UHB to consider the outstanding recommendations of the South Wales Programme (SWP) and how they should be appropriately considered and progressed in the current context. Background 3. The SWP within NHS Wales was set up in 2012 to look at the future of four consultant-led hospital services, specifically, maternity services, neonatal care, inpatient paediatric services and emergency medicine. These services were selected for consideration due to their fragility, in terms of their ability to deliver safe and sustainable models of care, as then configured. 4. The SWP was a partnership of the five health boards serving people living in South Wales and South Powys, working with the Welsh Ambulance Services NHS Trust (WAST). -

Annual Report 2010-11 Contents
Bwrdd Iechyd Cwm Taf Health Board Annual Report 2010-11 Contents Message from the Chair and Chief Clinical Services – Service Executive 4 Developments and Improvements 42 About the Health Board 6 Workforce and Organisational The Health Board Development (OD) 47 Committees Job Centre Plus Award Management Arrangements Health & Wellbeing Directors Interests Working in Partnership Governance 10 European Working Time Regulations Workforce Planning Health and Safety Learning and Development Freedom of Information Act 2000 Policy Development and Equal Opportunities Information on Emergency Preparedness Organisational Development (OD) Statement of Internal Control The Future Public Health 19 Our Workforce in Numbers What are our strategic priorities and where do we want Partnership Working 52 to be in 2015? Local Service Boards What are our key achievements this year? Health, Social Care and Wellbeing Partnerships Acute Stroke Services (HSCWB) – Merthyr Tydfi l and Rhondda Cynon Taff Research & Development 30 Children and Young People’s Partnerships – Merthyr Developments Tydfi l and Rhondda Cynon Taff Achievements Community Safety Partnerships – Merthyr Tydfi l and R&D Activity Rhondda Cynon Taff Forward Plan – Aims and Objectives 2011-2012 Welsh Health Specialised Services Patient Care and Safety 34 Committee (WHSSC) 57 Clinical Governance Arrangements Fundamentals of Care Welsh Health Estates 59 Complaints & Compliments 38 Facilities 60 Compliments Looking Forward to 2011-12 63 Performance 41 Financial Performance and Review 64 Waiting Times