The Development of the Modern Prostate Biopsy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2005 Tumori Della Vescica Visualizza
Basi scientifiche per la definizione di linee-guida in ambito clinico per i Tumori della Vescica Luglio 2005 1 2 PREFAZIONE Le “Basi scientifiche per la definizione di linee guida in ambito clinico per i Tumori della Vescica” rappresentano un ulteriore risultato del progetto editoriale sponsorizzato e finanziato dai Progetti Strategici Oncologia del CNR-MIUR. Anche in questo caso il proposito degli estensori è stato mirato non già alla costruzione di vere e proprie linee guida, ma a raccogliere in un unico compendio le principali evidenze scientifiche sull’epidemiologia, la diagnosi, l’inquadramento anatomo-patologico e biologico, la stadiazione, il trattamento e il follow-up delle neoplasie della vescica, che sono tra le patologie urologiche più frequenti e di maggiore rilevanza, anche sociale. Il materiale scientifico è ordinato in maniera sinottica, in modo da favorire la consultazione da parte di un’ampia utenza, non solo specialistica, ed è corredato dalle raccomandazioni scaturite dall’esperienza degli esperti qualificati che sono stati coinvolti nella estensione e nella revisione dei diversi capitoli. Tali raccomandazioni hanno lo scopo di consentire al lettore di costruire un proprio percorso diagnostico-terapeutico, alla luce anche delle evidenze fornite. Lasciamo pertanto al lettore il compito di integrare queste raccomandazioni con quanto proviene dalla personale esperienza e di conformarle con le linee guida già esistenti, in relazione anche alle specifiche esigenze. Vista la matrice di questa iniziativa, rappresentata dal CNR e MIUR, non potevano mancare nell’opera specifici riferimenti alle problematiche scientifiche, in grado di fornire spunti per le ricerche future. Certi che anche questa monografia potrà riscuotere lo stesso successo di quelle dedicate in precedenza al carcinoma della prostata e agli altri tumori solidi, sentiamo ancora una volta il dovere di esprimere la nostra gratitudine, per l’impegno e l’essenziale contributo, a tutti gli esperti coinvolti nel Gruppo di Studio e nel Gruppo di Consenso. -

Bladder Cancer
Clinical Practice in Urology Series Editor: Geoffrey D. Chisholm Titles in the series already published Urinary Diversion Edited by Michael Handley Ashken Chemotherapy and Urological Malignancy Edited by A. S. D. Spiers Urodynamics Paul Abrams, Roger Feneley and Michael Torrens Male Infertility Edited by T. B. Hargreave The Pharmacology of the Urinary Tract Edited by M. Caine Forthcoming titles in the series Urological Prostheses, Appliances and Catheters Edited by J. P. Pryor Percutaneous and Interventional Uroradiology Edited by Erich K. Lang Adenocarcinoma of the Prostate Edited by Andrew W. Bruce and John Trachtenberg Bladder Cancer Edited by E. J. Zingg and D. M. A. Wallace With 50 Figures Springer-Verlag Berlin Heidelberg New York Tokyo E. J. Zingg, MD Professor and Chairman, Department of Urology, Univ~rsity of Berne, Inselspital, 3010 Berne, Switzerland D. M. A. Wallace, FRCS Consultant Urologist, Department of Urology, Queen Elizabeth Medical Centre, Birmingham, England Series Editor Geoffrey D. Chisholm, ChM, FRCS, FRCSEd Professor of Surgery, University of Edinburgh; Consultant Urological Surgeon, Western General Hospital, Edinburgh, Scotland ISBN -13: 978-1-4471-1364-5 e-ISBN -13: 978-1-4471-1362-1 DOI: 10.1007/978-1-4471-1362-1 Library of Congress Cataloging in Publication Data Main entry under title: Bladder Cancer (Clinical Practice in Urology) Includes bibliographies and index. 1. Bladder - Cancer. I. Zingg, Ernst J. II. Wallace, D.M.A. (David Michael Alexander), 1946- DNLM: 1. Bladder Neoplasms. WJ 504 B6313 RC280.B5B632 1985 616.99'462 85-2572 ISBN-13:978-1-4471-1364-5 (U.S.) This work is subject to copyright. -
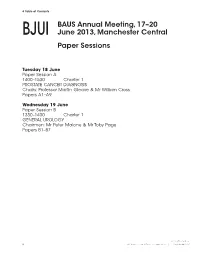
Paper Sessions
8 Table of Contents BAUS Annual Meeting, 17–20 BJUI June 2013, Manchester Central Paper Sessions Tuesday 18 June Paper Session A 1400–1530 Charter 1 PROSTATE CANCER DIAGNOSIS Chairs: Professor Martin Gleave & Mr William Cross Papers A1–A9 Wednesday 19 June Paper Session B 1330–1430 Charter 1 GENERAL UROLOGY Chairmen: Mr Peter Malone & Mr Toby Page Papers B1–B7 © 2013 The Authors 8 BJU International © 2013 BJU International | 111, Supplement 3, 8 Papers Abstracts 9 Tuesday 18 June BJUI Paper Session A 1400–1530 Charter 1 PROSTATE CANCER DIAGNOSIS Chairs: Professor Martin Gleave & Mr William Cross Papers A1–A9 A1 We then compared cancer yield in 50 Conclusion : Visualisation of each biopsy 3 D Visualisation of biopsy consecutive cases of positive prostate trajectory signifi cantly increases cancer trajectory and its clinical impact biopsies in the 2D vs. the 3D group (Part 2 detection rates and allows for a more in routine diagnostic TRUS guided of the study) through sampling of the prostate. Not only prostate biopsy Results : Th e results are tabulated as does this have a role in targeted biopsies K Narahari, A Peltier, R Van Velthoven follows but also in routine diagnostic biopsies. University Hospital of Wales, United Kingdom Introduction and Aims : Transrectal ultrasound (TRUS) guided biopsy remains Part 1 the gold standard in prostate cancer Parameter 2D USS * 3D USS *** P value diagnosis however prostate remains n = 110 n = 110 Student ’s t test perhaps the only solid organ where biopsy Age in years 64 (46–90) 65 (46–84) NS is “blind”. Traditionally the surgeon would Mean (Range) prepare a “mental image” of the prostate PSA ng/ml 9 (0.5–70) 10 (0.5–59) NS and target his biopsy cores evenly to map Mean (Range) out the prostate as best as possible. -

Prostate Cancer Early Detection, Diagnosis, and Staging Finding Prostate Cancer Early
cancer.org | 1.800.227.2345 Prostate Cancer Early Detection, Diagnosis, and Staging Finding Prostate Cancer Early Catching cancer early often allows for more treatment options. Some early cancers may have signs and symptoms that can be noticed, but that is not always the case. ● Can Prostate Cancer Be Found Early? ● Screening Tests for Prostate Cancer ● American Cancer Society Recommendations for Prostate Cancer Early Detection ● Insurance Coverage for Prostate Cancer Screening Diagnosis and Planning Treatment After a cancer diagnosis, staging provides important information about the extent of cancer in the body and anticipated response to treatment. ● Signs and Symptoms of Prostate Cancer ● Tests to Diagnose and Stage Prostate Cancer ● Prostate Pathology ● Prostate Cancer Stages and Other Ways to Assess Risk ● Survival Rates for Prostate Cancer ● Questions To Ask About Prostate Cancer 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 Can Prostate Cancer Be Found Early? Screening is testing to find cancer in people before they have symptoms. For some types of cancer, screening can help find cancers at an early stage, when they are likely to be easier to treat. Prostate cancer can often be found early by testing for prostate-specific antigen (PSA) levels in a man’s blood. Another way to find prostate cancer is the digital rectal exam (DRE). For a DRE, the doctor puts a gloved, lubricated finger into the rectum to feel the prostate gland. These tests and the actual process of screening are described in more detail in Screening Tests for Prostate Cancer. If the results of either of these tests is abnormal, further testing (such as a prostate biopsy) is often done to see if a man has cancer. -

Primary Urethral Carcinoma
EAU Guidelines on Primary Urethral Carcinoma G. Gakis, J.A. Witjes, E. Compérat, N.C. Cowan, V. Hernàndez, T. Lebret, A. Lorch, M.J. Ribal, A.G. van der Heijden Guidelines Associates: M. Bruins, E. Linares Espinós, M. Rouanne, Y. Neuzillet, E. Veskimäe © European Association of Urology 2017 TABLE OF CONTENTS PAGE 1. INTRODUCTION 3 1.1 Aims and scope 3 1.2 Panel composition 3 1.3 Publication history and summary of changes 3 1.3.1 Summary of changes 3 2. METHODS 3 2.1 Data identification 3 2.2 Review 3 2.3 Future goals 4 3. EPIDEMIOLOGY, AETIOLOGY AND PATHOLOGY 4 3.1 Epidemiology 4 3.2 Aetiology 4 3.3 Histopathology 4 4. STAGING AND CLASSIFICATION SYSTEMS 5 4.1 Tumour, Node, Metastasis (TNM) staging system 5 4.2 Tumour grade 5 5. DIAGNOSTIC EVALUATION AND STAGING 6 5.1 History 6 5.2 Clinical examination 6 5.3 Urinary cytology 6 5.4 Diagnostic urethrocystoscopy and biopsy 6 5.5 Radiological imaging 7 5.6 Regional lymph nodes 7 6. PROGNOSIS 7 6.1 Long-term survival after primary urethral carcinoma 7 6.2 Predictors of survival in primary urethral carcinoma 7 7. DISEASE MANAGEMENT 8 7.1 Treatment of localised primary urethral carcinoma in males 8 7.2 Treatment of localised urethral carcinoma in females 8 7.2.1 Urethrectomy and urethra-sparing surgery 8 7.2.2 Radiotherapy 8 7.3 Multimodal treatment in advanced urethral carcinoma in both genders 9 7.3.1 Preoperative platinum-based chemotherapy 9 7.3.2 Preoperative chemoradiotherapy in locally advanced squamous cell carcinoma of the urethra 9 7.4 Treatment of urothelial carcinoma of the prostate 9 8. -

Urology Clinical Privileges
Urology Clinical Privileges Name: _____________________________________________________ Effective from _______/_______/_______ to _______/_______/_______ ❏ Initial privileges (initial appointment) ❏ Renewal of privileges (reappointment) All new applicants should meet the following requirements as approved by the governing body, effective: February 18, 2015 Applicant: Check the “Requested” box for each privilege requested. Applicants are responsible for producing required documentation for a proper evaluation of current skill, current clinical activity, and other qualifications and for resolving any doubts related to qualifications for requested privileges. Please provide this supporting information separately. [Department/Program Head or Leaders/ Chief]: Check the appropriate box for recommendation on the last page of this form and include your recommendation for any required evaluation. If recommended with conditions or not recommended, provide the condition or explanation on the last page of this form. Current experience is an estimate of the level of activity below which a collegial discussion about support should be triggered. It is not a disqualifier. This discussion should be guided not only by the expectations and standards outlined in the dictionary but also by the risks inherent in the privilege being discussed and by similar activities that contribute to the skill under consideration. This is an opportunity to reflect with a respected colleague on one's professional practice and to deliberately plan an approach to skills maintenance. Other requirements • Note that privileges granted may only be exercised at the site(s) and/or setting(s) that have sufficient space, equipment, staffing, and other resources required to support the privilege. • This document is focused on defining qualifications related to competency to exercise clinical privileges. -

Frontiers in Oncologic Prostate Care and Ablative Local Therapy
Frontiers in Oncologic Prostate Care and Ablative Local Therapy FOR MORE INFORMATION& TO REGISTER www.focalcme.com FACULTY PROGRAM DIRECTORS Arvin K. George, MD Abhinav Sidana, MD FACULTY Andre Abreu, MD Hashim U. Ahmed, MD Casey Dauw, MD Mihir Desai, MD Christopher Dixon, MD Mark Emberton, MD, FRCS Inderbir S. Gill, MD Amin Herati, MD Amar Kishan, MD Amir Lebastchi, MD Leonard S. Marks, MD Peter A. Pinto, MD Thomas J. Polascik, MD Art R. Rastinehad, DO Stephen Scionti, MD M. Minhaj Siddiqui, MD Samir S. Taneja, MD Sadhna Verma, MD Srinivas Vourganti, MD Jonathan Warner, MD James Wysock, MD FOCAL2020 AGENDA OCTOBER 3-4, 2020 Frontiers in Oncologic Prostate Care and Ablative Local Therapy WWW.FOCALCME.COM SATURDAY, OCTOBER 3, 2020 (9:25 AM - 7:00 PM EDT) SESSION 1: PROSTATE MRI/FUSION BIOPSY 9:25 am Welcome Remarks Arvin K. George, MD 9:30 am – 9:45 am The Evidence for Prostate MRI and Fusion Biopsy Peter A. Pinto, MD 9:45 am – 10:10 am Prostate MRI for the Urologist Sadhna Verma, MD 10:10 am – 10:30 am LIVE Interactive Session: Prostate MRI Case Review Art R. Rastinehad, DO SESSION 2: INTRODUCTION TO FOCAL THERAPY 10:30 am – 10:45 am Rationale for Focal Therapy Mark Emberton, MD, FRCS 10:45 am – 11:00 am Patient Selection for Focal Therapy James Wysock, MD 11:00 am – 11:10 am Role of Biomarkers in Patient Selection in Focal Therapy M. Minhaj Siddiqui, MD 11:10 am – 11:25 am Live Discussion 11:25 am – 11:40 am COFFEE TALK: Considerations of Brachytherapy for Focal Treatment Ronald M. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Poster Sessions
TABLE OF CONTENTS BAUS Annual Meeting, 25–28 June 2012, BJUI Glasgow, SECC SUPPLEMENTS Poster Sessions Tuesday 26 June 2012 Poster Session 1 11:00–12:30 Alsh PROSTATE CANCER DIAGNOSIS Chairmen: Mr Rick Popert & Mr Garrett Durkan Posters P1–P10 Poster Session 2 11:00–12:30 Carron UPPER TRACT DISORDERS AND IMAGING Chairmen: Mr Toby Page & Mr Chandra Shekhar Biyani Posters P11–P20 Poster Session 3 14:00–16:00 Alsh SCIENTIFIC DISCOVERY Chairpersons: Mr Rakesh Heer & Mrs Caroline Moore Posters P21–P34 Poster Session 4 14:00–16:00 Carron STONES Chairpersons: Mr Daron Smith & Miss Kay Thomas Posters P35–P45 Wednesday 27 June 2012 Poster Session 5 11:00–12:30 Alsh BLADDER CANCER Chairpersons: Ms Jo Cresswell & Mr Rik Bryan Posters P46–P57 © 2012 THE AUTHORS 14 BJU INTERNATIONAL © 2012 BJU INTERNATIONAL | 109, SUPPLEMENT 7, 14–15 TABLE OF CONTENTS Poster Session 6 11:00–12:30 Carron TECHNIQUES AND INNOVATION Chairmen: Mr Ghulam Nabi & Mr John McGrath Posters P58–P67 Poster Session 7 14:00–16:00 Alsh FEMALE UROLOGY AND LUTS Chairpersons: Mr Chris Harding & Miss Mary Garthwaite Posters P68–P82 Thursday 28 June 2012 Poster Session 8 11:00–12:30 Alsh ANDROLOGY Chairmen: Mr Richard Pearcy & Mr Mike Foster Posters P83–P92 Poster Session 9 11:00–12:30 Carron RENAL CANCER Chairmen: Mr Simon Williams & Mr Neil Barber Posters P93–P102 © 2012 THE AUTHORS BJU INTERNATIONAL © 2012 BJU INTERNATIONAL | 109, SUPPLEMENT 7, 14–15 15 POSTER ABSTRACTS Tuesday 26 June 2012 BJUI Poster Session 1 SUPPLEMENTS 11:00–12:30 Alsh PROSTATE CANCER DIAGNOSIS Chairmen: Mr Rick Popert & Mr Garrett Durkan Posters P1–P10 P1 compared with the most affl uent. -

Bladder Cancer
PDF hosted at the Radboud Repository of the Radboud University Nijmegen The following full text is a publisher's version. For additional information about this publication click this link. http://hdl.handle.net/2066/19207 Please be advised that this information was generated on 2021-09-27 and may be subject to change. SUPERFICIAL BLADDER CANCER PROGNOSIS AND MANAGEMENT SUPERFICIAL BLADDER CANCER PROGNOSIS AND MANAGEMENT een wetenschappelijke proeve op het gebied van de Medische Wetenschappen Proefschrift ter verkrijging van de graad van doctor aan de Katholieke Universiteit Nijmegen op gezag van de Rector Magnificus Prof. dr. C. W. P. M. Blom, volgens besluit van het College van Decanen in het openbaar te verdedigen op woensdag 11 december 2002 des morgens om 11.00 uur precies door Necmettin Aydin Mungan geboren op 24 maart 1965 te Ankara Promotor : Prof. dr. F.M.J. Debruyne Co-Promotores : Dr. J.A. Witjes Dr. L.A.L.M. Kiemeney Manuscriptcommissie : Prof. dr. P. de Mulder Prof. dr. A.L.M. Lagro-Janssen Prof. dr. H. Boonstra Superficial bladder cancer: prognosis and management Necmettin Aydin Mungan ISBN 90-9016303-4 Printed by: ZES Tanitim, Ankara Cover design: Superficial bladder cancer Publication of this thesis was sponsored by: Onko&Koçsel Pharmaceuticals and Aventis Pasteur, Schering-Plough and Abbott Laboratories To my wife and kids Science is the truest guide for life, success and everything else in the world. Mustafa Kemal Ataturk Founder of Republic of Turkey CONTENTS Chapter Title Page 1 Introduction and outline of the thesis 9 2 Gender differences of (superficial) bladder cancer 21 3 Can sensitivity of voided urinary cytology or bladder 67 wash cytology be improved by the use of different urinary portions? 4 Detection of malignant cells: Can cytology be 79 replaced? 5 Comparison of the diagnostic value of the BTA Stat 101 Test with voided urinary cytology for detection of bladder cancer. -

The Precision Prostatectomy: an IDEAL Stage 0, 1 and 2A Study
Open access Original article BMJ Surg Interv Health Technologies: first published as 10.1136/bmjsit-2019-000002 on 19 August 2019. Downloaded from The Precision Prostatectomy: an IDEAL Stage 0, 1 and 2a Study Akshay Sood, 1 Wooju Jeong,1 Kanika Taneja,2 Firas Abdollah,1 Isaac Palma-Zamora,1 Sohrab Arora,1 Nilesh Gupta,2 Mani Menon1 To cite: Sood A, Jeong W, ABSTRACT Key messages Taneja K, et al. The Precision Objective This study aimed to develop a preclinical model Prostatectomy: an IDEAL Stage of prostate cancer (CaP) for studying focal/hemiablation What is already known about this subject? 0, 1 and 2a Study. BMJ Surg of the prostate (IDEAL stage 0), and to use the information Interv Health Technologies Whole-gland treatment of prostate cancer (CaP) of- from the stage 0 investigation to design a novel focal ► 2019;1:e000002. doi:10.1136/ ten leads to unintended adverse functional effects, surgical treatment approach—the precision prostatectomy bmjsit-2019-000002 in particular, sexual impotence. (IDEAL stage 1/2a). ► Focal ablative techniques for treatment of local- Received 18 March 2019 Methods The IDEAL stage 0 study included simulation ized CaP have recently emerged to avoid such Revised 17 July 2019 of focal/hemiablation in whole-mount prostate functional decline; although these focal ablative Accepted 17 July 2019 specimens obtained from 100 men who had undergone techniques have shown promise, a few limitations radical prostatectomies, but met the criteria for focal/ have emerged: (1) an inability or reluctance to treat hemiablation. The IDEAL stage 1/2a was a prospective, a prostate gland >40 gm, (2) an inability to ablate single-arm, Institutional Review Board-approved study of >60% of the whole gland, (3) lack of pathological precision prostatectomy undertaken in eight men, who information, and (4) a high positive biopsy rate in the met the predetermined criteria. -

Prostate Gland Biopsy
PROSTATE GLAND BIOPSY EUGENE F. POUTASSE, M.D. Department of Urology HE incidence of cancer of the prostate gland among men who have symp- Ttoms of bladder neck obstruction is about one out of five. The actual inci- dence of cancer is higher because many men are seen with symptoms unrelated to the urinary tract, such as bone pain, or who have evidence of the tumor without symptoms. It is the third most common cancer in men, exceeded only by cancer of the skin and alimentary tract in frequency of recognition. The chief methods by which a physician discovers prostatic cancer are rectal palpation of the gland, serum acid phosphatase determination, and roentgenographic study of the urinary tract and skeleton. These are satisfactory when the tumor has spread widely beyond the prostate. In this paper methods of biopsy for establishing the diagnosis when cancer of the prostate gland is suspected or when it is desirable to corroborate the clinical diagnosis of exten- sive cancer will be discussed. The actual diagnosis of cancer is made by micro- scopic definition, preferably on a block of tumor tissue. Under study is the cytologic examination of prostatic secretion for exfoliated tumor cells,1 which requires a great deal of time and experience. Methods of Biopsy A. Perineal. Exposure of the prostate gland through the perineum permits biopsy of any area of the gland which has been suspected of malignancy on rectal palpation. This approach is particularly useful because more than 90 per cent of all prostatic neoplasms arise in the posterior lobe accessible to rectal palpation.