Respiratory Support
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Oxyhaemoglobin Dissociation Curve in Critical Illness
Basic sciences review The Oxyhaemoglobin Dissociation Curve in Critical Illness T. J. MORGAN Intensive Care Facility, Division of Anaesthesiology and Intensive Care, Royal Brisbane Hospital, Brisbane, QUEENSLAND ABSTRACT Objective: To review the status of haemoglobin-oxygen affinity in critical illness and investigate the potential to improve gas exchange, tissue oxygenation and outcome by manipulations of the oxyhaemoglobin dissociation curve. Data sources: Articles and published peer-review abstracts. Summary of review: The P50 of a species is determined by natural selection according to animal size, tissue metabolic requirements and ambient oxygen tension. In right to left shunting mathematical modeling indicates that an increased P50 defends capillary oxygenation, the one exception being sustained hypercapnia. Increasing the P50 should also be protective in tissue ischaemia, and this is supported by modeling and experimental evidence. Most studies of critically ill patients have indicated reduced 2,3-DPG concentrations. This is probably due to acidaemia, and the in vivo P50 is likely to be normal despite low 2,3-DPG levels. It may soon be possible to achieve significant P50 elevations without potentially harmful manipulations of acid-base balance or hazardous drug therapy. Conclusions: Despite encouraging theoretical and experimental data, it is not known whether manipulations of the P50 in critical illness can improve gas exchange and tissue oxygenation or improve outcome. The status of the P50 may warrant more routine quantification and consideration along with the traditional determinants of tissue oxygen availability. (Critical Care and Resuscitation 1999; 1: 93-100) Key words: Critical illness, haemoglobin-oxygen affinity, ischaemia, P50, tissue oxygenation, shunt In intensive care practice, manipulations to improve in the tissues. -

Oxygenation and Oxygen Therapy
Rules on Oxygen Therapy: Physiology: 1. PO2, SaO2, CaO2 are all related but different. 2. PaO2 is a sensitive and non-specific indicator of the lungs’ ability to exchange gases with the atmosphere. 3. FIO2 is the same at all altitudes 4. Normal PaO2 decreases with age 5. The body does not store oxygen Therapy & Diagnosis: 1. Supplemental O2 is an FIO2 > 21% and is a drug. 2. A reduced PaO2 is a non-specific finding. 3. A normal PaO2 and alveolar-arterial PO2 difference (A-a gradient) do NOT rule out pulmonary embolism. 4. High FIO2 doesn’t affect COPD hypoxic drive 5. A given liter flow rate of nasal O2 does not equal any specific FIO2. 6. Face masks cannot deliver 100% oxygen unless there is a tight seal. 7. No need to humidify if flow of 4 LPM or less Indications for Oxygen Therapy: 1. Hypoxemia 2. Increased work of breathing 3. Increased myocardial work 4. Pulmonary hypertension Delivery Devices: 1. Nasal Cannula a. 1 – 6 LPM b. FIO2 0.24 – 0.44 (approx 4% per liter flow) c. FIO2 decreases as Ve increases 2. Simple Mask a. 5 – 8 LPM b. FIO2 0.35 – 0.55 (approx 4% per liter flow) c. Minimum flow 5 LPM to flush CO2 from mask 3. Venturi Mask a. Variable LPM b. FIO2 0.24 – 0.50 c. Flow and corresponding FIO2 varies by manufacturer 4. Partial Rebreather a. 6 – 10 LPM b. FIO2 0.50 – 0.70 c. Flow must be sufficient to keep reservoir bag from deflating upon inspiration 5. -

Measurement of the Respiratory Quotient of Peat
Utah State University DigitalCommons@USU Hydroponics/Soilless Media Research 8-10-2012 Measurement of the Respiratory Quotient of Peat Jake Nelson Follow this and additional works at: https://digitalcommons.usu.edu/cpl_hydroponics Part of the Plant Sciences Commons Recommended Citation Nelson, Jake, "Measurement of the Respiratory Quotient of Peat" (2012). Hydroponics/Soilless Media. Paper 5. https://digitalcommons.usu.edu/cpl_hydroponics/5 This Article is brought to you for free and open access by the Research at DigitalCommons@USU. It has been accepted for inclusion in Hydroponics/Soilless Media by an authorized administrator of DigitalCommons@USU. For more information, please contact [email protected]. Measurement of the respiratory quotient of peat Jake Nelson 8/10/2012 BIOL 5800 Undergraduate Research Summer 2010 Introduction Respiratory quotient (RQ) is the ratio of CO produced to O consumed by an organism. Complete respiration 2 2 of glucose will give an RQ of 1 as described by the formula C H O +nO →nCO +nH O. The respiration of n 2n n 2 2 2 molecules with lower oxygen content, such as lipids, give RQ values of less than one, whereas in cases of anaerobic metabolism, an increase in biomass or the respiration of substances such as humic, oxalic and citric acids the respiratory quotient can be greater than one. In complex systems such as soil, Dilly (2003) found that the RQ varied dramatically, and changed within the same soil under varying conditions. Similarly, Hollender et al. (2003) found RQ was informative in determining the underlying metabolic mechanisms, such as nitrification processes. Dilly (2004), studied the effects of various organic compounds on RQ, and found that beech forest soils amended with cellulose or humic acid maintained RQ values greater than one for more than 20 days after application. -

The Role Identity Plays in B-Ball Players' and Gangsta Rappers
Vassar College Digital Window @ Vassar Senior Capstone Projects 2016 Playin’ tha game: the role identity plays in b-ball players’ and gangsta rappers’ public stances on black sociopolitical issues Kelsey Cox Vassar College Follow this and additional works at: https://digitalwindow.vassar.edu/senior_capstone Recommended Citation Cox, Kelsey, "Playin’ tha game: the role identity plays in b-ball players’ and gangsta rappers’ public stances on black sociopolitical issues" (2016). Senior Capstone Projects. 527. https://digitalwindow.vassar.edu/senior_capstone/527 This Open Access is brought to you for free and open access by Digital Window @ Vassar. It has been accepted for inclusion in Senior Capstone Projects by an authorized administrator of Digital Window @ Vassar. For more information, please contact [email protected]. Cox playin’ tha Game: The role identity plays in b-ball players’ and gangsta rappers’ public stances on black sociopolitical issues A Senior thesis by kelsey cox Advised by bill hoynes and Justin patch Vassar College Media Studies April 22, 2016 !1 Cox acknowledgments I would first like to thank my family for helping me through this process. I know it wasn’t easy hearing me complain over school breaks about the amount of work I had to do. Mom – thank you for all of the help and guidance you have provided. There aren’t enough words to express how grateful I am to you for helping me navigate this thesis. Dad – thank you for helping me find my love of basketball, without you I would have never found my passion. Jon – although your constant reminders about my thesis over winter break were annoying you really helped me keep on track, so thank you for that. -
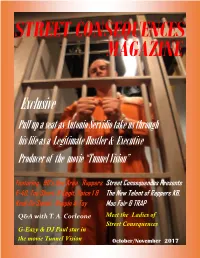
G-Eazy & DJ Paul Star in the Movie Tunnel Vision October/November 2017 in the BAY AREA YOUR VIEW IS UNLIMITED
STREET CONSEQUENCES MAGAZINE Exclusive Pull up a seat as Antonio Servidio take us through his life as a Legitimate Hustler & Executive Producer of the movie “Tunnel Vision” Featuring 90’s Bay Area Rappers Street Consequences Presents E-40, Too Short, B-Legit, Spice 1 & The New Talent of Rappers KB, Keak Da Sneak, Rappin 4-Tay Mac Fair & TRAP Q&A with T. A. Corleone Meet the Ladies of Street Consequences G-Eazy & DJ Paul star in the movie Tunnel Vision October/November 2017 IN THE BAY AREA YOUR VIEW IS UNLIMITED October/November 2017 2 October /November 2017 Contents Publisher’s Word Exclusive Interview with Antonio Servidio Featuring the Bay Area Rappers Meet the Ladies of Street Consequences Street Consequences presents new talent of Rappers October/November 2017 3 Publisher’s Words Street Consequences What are the Street Consequences of today’s hustling life- style’s ? Do you know? Do you have any idea? Street Con- sequences Magazine is just what you need. As you read federal inmates whose stories should give you knowledge on just what the street Consequences are. Some of the arti- cles in this magazine are from real people who are in jail because of these Street Consequences. You will also read their opinion on politics and their beliefs on what we, as people, need to do to chance and make a better future for the up-coming youth of today. Stories in this magazine are from big timer in the games to small street level drug dealers and regular people too, Hopefully this magazine will open up your eyes and ears to the things that are going on around you, and have to make a decision that will make you not enter into the game that will leave you dead or in jail. -

Respiratory Physiology for the Anesthesiologist
REVIEW ARTICLE Deborah J. Culley, M.D., Editor ABSTRACT Respiratory function is fundamental in the practice of anesthesia. Knowledge of basic physiologic principles of respiration assists in the proper implemen- tation of daily actions of induction and maintenance of general anesthesia, Respiratory Physiology delivery of mechanical ventilation, discontinuation of mechanical and pharma- cologic support, and return to the preoperative state. The current work pro- Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/130/6/1064/455191/20190600_0-00035.pdf by guest on 24 September 2021 for the Anesthesiologist vides a review of classic physiology and emphasizes features important to the anesthesiologist. The material is divided in two main sections, gas exchange Luca Bigatello, M.D., Antonio Pesenti, M.D. and respiratory mechanics; each section presents the physiology as the basis ANESTHESIOLOGY 2019; 130:1064–77 of abnormal states. We review the path of oxygen from air to the artery and of carbon dioxide the opposite way, and we have the causes of hypoxemia and of hypercarbia based on these very footpaths. We present the actions nesthesiologists take control of the respiratory func- of pressure, flow, and volume as the normal determinants of ventilation, and Ation of millions of patients throughout the world each we review the resulting abnormalities in terms of changes of resistance and day. We learn to maintain gas exchange and use respiration compliance. to administer anesthetic gases through the completion of (ANESTHESIOLOGY 2019; 130:1064–77) surgery, when we return this vital function to its legitimate owners, ideally with a seamless transition to a healthy post- operative course. -

Respiratory Therapy Pocket Reference
Pulmonary Physiology Volume Control Pressure Control Pressure Support Respiratory Therapy “AC” Assist Control; AC-VC, ~CMV (controlled mandatory Measure of static lung compliance. If in AC-VC, perform a.k.a. a.k.a. AC-PC; Assist Control Pressure Control; ~CMV-PC a.k.a PS (~BiPAP). Spontaneous: Pressure-present inspiratory pause (when there is no flow, there is no effect ventilation = all modes with RR and fixed Ti) PPlateau of Resistance; Pplat@Palv); or set Pause Time ~0.5s; RR, Pinsp, PEEP, FiO2, Flow Trigger, rise time, I:E (set Pocket Reference RR, Vt, PEEP, FiO2, Flow Trigger, Flow pattern, I:E (either Settings Pinsp, PEEP, FiO2, Flow Trigger, Rise time Target: < 30, Optimal: ~ 25 Settings directly or by inspiratory time Ti) Settings directly or via peak flow, Ti settings) Decreasing Ramp (potentially more physiologic) PIP: Total inspiratory work by vent; Reflects resistance & - Decreasing Ramp (potentially more physiologic) Card design by Respiratory care providers from: Square wave/constant vs Decreasing Ramp (potentially Flow Determined by: 1) PS level, 2) R, Rise Time ( rise time ® PPeak inspiratory compliance; Normal ~20 cmH20 (@8cc/kg and adult ETT); - Peak Flow determined by 1) Pinsp level, 2) R, 3)Ti (shorter Flow more physiologic) ¯ peak flow and 3.) pt effort Resp failure 30-40 (low VT use); Concern if >40. Flow = more flow), 4) pressure rise time (¯ Rise Time ® Peak v 0.9 Flow), 5) pt effort ( effort ® peak flow) Pplat-PEEP: tidal stress (lung injury & mortality risk). Target Determined by set RR, Vt, & Flow Pattern (i.e. for any set I:E Determined by patient effort & flow termination (“Esens” – PDriving peak flow, Square (¯ Ti) & Ramp ( Ti); Normal Ti: 1-1.5s; see below “Breath Termination”) < 15 cmH2O. -

E-40 Album Download DOWNLOAD ALBUM: Too Short & E-40 -Ain’T Gone Do It Terms and Conditions ZIP
e-40 album download DOWNLOAD ALBUM: Too Short & E-40 -Ain’t Gone Do It Terms and Conditions ZIP. DOWNLOAD Too Short & E-40 Ain’t Gone Do It Terms and Conditions ZIP & MP3 File. Ever Trending Star drops this amazing song titled “Too Short & E-40 – Ain’t Gone Do It Terms and Conditions Album“, its available for your listening pleasure and free download to your mobile devices or computer. You can Easily Stream & listen to this new “ FULL ALBUM: Too Short & E-40 – Ain’t Gone Do It Terms and Conditions Zip File” free mp3 download” 320kbps, cdq, itunes, datafilehost, zip, torrent, flac, rar zippyshare fakaza Song below. E-40 album download. Artist: E-40 And B-Legit Album: Connected And Respected Released: 2018 Style: Hip Hop. Format: MP3 320Kbps. Tracklist: 01 – Life Lessons 02 – Straight Like That 03 – Boy 04 – Guilty By Association 05 – Carpal Tunnel 06 – Stompdown (Skit 1) 07 – Meet The Dealers 08 – Get It On My Own 09 – Up Against It 10 – Fsho 11 – Whooped 12 – Tap In 13 – You Ah Lie 14 – Need To Know 15 – Stompdown (Skit 2) 16 – Bare 17 – Barbershop 18 – Blame It 19 – So High. DOWNLOAD LINKS: RAPIDGATOR: DOWNLOAD TURBOBIT: DOWNLOAD. E-40 Discography @ 320 (21 Albums+1)(RAP)(by dragan09) 1990 - E-40 - Mr. Flamboyant @192 1994 - E-40 - Federal 1994 - E-40 - The Mail Man (EP) 1995 - E-40 - In a Major Way 1996 - E-40 - Tha Hall of Game 1997 - E-40 & B-Legit - Southwest Riders (2 CD`s) 1998 - E-40 - The Element Of Surprise (2 CD`s) 1999 - E-40 - Charlie Hustle - The Blueprint of a Self-Made Millionaire 2000 - E-40 - Loyalty and Betrayal 2002 - E-40 - Grit & Grind 2003 - E-40 - Breakin' News 2004 - E-40 - My Ghetto Report Card 2008 - E-40 - The Ball Street Journal 2010 - E-40 - Revenue Retrievin' Day Shift 2010 - E-40 - Revenue Retrievin' Night Shift 2011 - E-40 - Revenue Retrievin'. -

Effect of Positive End-Expiratory Pressure on Intrapulmonary Shunt at Different Levels of Fractional Inspired Oxygen
Thorax: first published as 10.1136/thx.35.3.181 on 1 March 1980. Downloaded from Thorax, 1980, 35, 181-186 Effect of positive end-expiratory pressure on intrapulmonary shunt at different levels of fractional inspired oxygen A OLIVEN, U TAITELMAN, F ZVEIBIL, AND S BURSZTEIN From the Intensive Care Department, Rambam Medical Centre, Haifa, Israel ABSTRACT In 10 patients undergoing ventilation, venous admixture was measured at different values of positive end-expiratory pressure (PEEP). The measurements were performed at the level of fractional inspired oxygen (FIO2) at which each patient was ventilated, and at FIo2=1. In patients ventilated at FIo2 between 0-21 and 0 3 venous admixture was not modified by PEEP, while in patients ventilated with FIO2 between 0'4 and 0-6, venous admixture decreased significantly (p<0 01). With FIO2=1, increased PEEP produced a reduction in venous admixture in all cases (p < 0 .05). These observations suggest that in patients similar to ours, PEEP does not reduce venous admixture at low levels of Fio2 (0-21-0.3), and the observed reduction with PEEP at FIO2= I may be misinterpreted. copyright. In patients with acute respiratory failure, and vital signs and minute volume were positive end-expiratory pressure (PEEP) has repeatedly checked, in order to confirm steady been said to reduce pulmonary venous admixture state condi-tions. Blood samples were drawn and improve arterial blood oxygenation.13 The simultaneously into heparinised glass syringes efficiency of PEEP can thus be -evaluated by its from an indwelling arterial line and from a http://thorax.bmj.com/ influence on venous admixture. -

Small Door Veterinary
CAT PARENTING 101 Everything you need to know about caring for your new cat. Cat Parenting 101 | Page 2 CONGRATULATIONS! Welcoming a new cat into your family is one of the most rewarding experiences in life, and we’re so excited for you to get to know your new furry family member over the coming days and weeks. As a new cat owner, there’s a lot to learn, so we’ve put together this comprehensive guide to help you navigate cat parenthood. Remember – as a Small Door member, you can contact us 24/7 via the app for advice or if you ever have any concerns about your new kitty. Best of luck, and we can’t wait to meet you both at the practice soon! CONTENTS Page 3 The essentials, on one page Page 22 Grooming Page 22 Nail trimming Page 4 Bringing your new cat home Page 23 Ear cleaning Page 4 Preparing your home Page 5 The first day with your new cat Page 24 Medical care Page 5 Introducing your cat to other pets Page 24 Vaccinations Page 25 Vaccine reactions Page 7 Socialization Page 25 Preventatives Page 26 Wellness care schedules Page 8 Stimulation, exercise & play Page 27 Indoor cats Page 8 Toys Page 28 Spaying and neutering Page 10 How to play with your cat Page 29 Dental health Page 11 How much playtime do cats need? Page 30 How to brush your cat’s teeth Page 11 Catios for indoor cats Page 31 Microchipping Page 12 Behavior & training Page 31 Pet insurance Page 12 Positive reinforcement Page 32 Developing a positive vet experience Page 12 Discouraging unwanted behaviors Page 33 Common problems & when to seek help Page 14 Litter box training Page -

Respiratory Equations – Behind the Numbers
Southern African Journal of Anaesthesia and Analgesia. 2020;26(6 Suppl 3):S90-93 https://doi.org/10.36303/SAJAA.2020.26.6.S3.2546 South Afr J Anaesth Analg Open Access article distributed under the terms of the ISSN 2220-1181 EISSN 2220-1173 Creative Commons License [CC BY-NC 3.0] © 2020 The Author(s) http://creativecommons.org/licenses/by-nc/3.0 FCA 1 REFRESHER COURSE Respiratory equations – behind the numbers T Leonard Department of Anaesthesia, School of Clinical Medicine, Faculty of Health Sciences, Chris Hani Baragwanath Academic Hospital, University of the Witwatersrand, South Africa Corresponding author, email: [email protected] Summary Candidates for the FCA 1 exam will come across dozens of equations that eventually all merge into something complicated and daunting. The purpose of this review is to highlight some of the respiratory equations that are important and that candidates find confusing and explain the mathematical and physiological principles behind them. Keywords: equations, respiratory physiology, ventilation, perfusion, dead space Introduction VD / VT = (PACO2 – PECO2) / PACO2 P CO partial pressure of CO in alveolar gas There are many equations that candidates will come across in A 2 2 their study of respiratory physiology. These equations describe PECO2 partial pressure of CO2 in the total mixed principles of ventilation, perfusion and diffusion within the res- exhaled breath piratory system. This review attempts to explain the origins and A further modification was made by Henrik Enghoff due to make sense -

1. Ventilator Management
1. Ventilator Management Indications for Mechanical Ventilation Apnea Ventilatory insufficiency Increase in PaCo2 and decrease in ph Refractory hypoxemia Complications Associated with Mechanical Ventilation Hypotension Increased intrathoracic pressure decreases venous return to the heart Increased risk of ventilator associated pneumonia (VAP) Keep HOB at > 30 Maintain frequent, good oral care Problems with endotracheal tube Mucous plugging Tube my become dislodged Kinking or biting of tube Cuff rupture Pneumothorax Initial Ventilator Settings—parameters to be clarified Type of ventilation Mode of ventilation Tidal volume or peak inspiratory setting Respiratory rate FiO2 PEEP (Positive End Expiratory Pressure) Types of Ventilation Volume Cycled Ventilation(VCV) A pre-selected tidal volume is delivered at the pressure required. Tidal volume guaranteed. Peak inspiratory pressure will vary depending on airway resistance and lung compliance. Pressure Control Time-Cycled Ventilation (PCV) Operator selects inspiratory pressure and inspiratory time Breath is terminated when inspiratory time is reached Inspiratory pressure is guaranteed; tidal volume is dependant on airway resistance and lung compliance Pressure Support (PSV) Requires intact respiratory drive Operator selects inspiratory pressure Patient initiates breath, pressure quickly rises to set pressure and is maintained throughout the inspiratory phase Tidal volume determined by lung compliance and inspiratory effort Modes of Ventilation Assist/Control