Cardiac Output Monitoring: a Comparative Prospective
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Product ID Product Type Product Description Notes Price (USD) Weight (KG) SKU 10534 Mobile-Phone Apple Iphone 4S 8GB White 226.8
Rm A1,10/F, Shun Luen Factory Building, 86 Tokwawan Road, Hong Kong TEL: +852 2325 1867 FAX: +852 23251689 Website: http://www.ac-electronic.com/ For products not in our pricelist, please contact our sales. 29/8/2015 Product Price Weight Product Type Product Description Notes SKU ID (USD) (KG) 10534 mobile-phone Apple iPhone 4S 8GB White 226.8 0.5 40599 10491 mobile-phone Apple iPhone 5s 16GB Black Slate 486.4 0.5 40557 10497 mobile-phone Apple iPhone 5s 16GB Gold 495.6 0.5 40563 10494 mobile-phone Apple iPhone 5s 16GB White Silver 487.7 0.5 40560 10498 mobile-phone Apple iPhone 5s 32GB Gold 536.3 0.5 40564 11941 mobile-phone Apple iPhone 6 128GB Gold 784.1 0.5 41970 11939 mobile-phone Apple iPhone 6 16GB Gold 622.8 0.5 41968 11936 mobile-phone Apple iPhone 6 16GB Silver 633.3 0.5 41965 11942 mobile-phone Apple iPhone 6 16GB Space Grey 618.9 0.5 41971 11940 mobile-phone Apple iPhone 6 64GB Gold 705.4 0.5 41969 11937 mobile-phone Apple iPhone 6 64GB Silver 706.7 0.5 41966 11943 mobile-phone Apple iPhone 6 64GB Space Grey 708 0.5 41972 11963 mobile-phone Apple iPhone 6 Plus 128GB Silver 917.9 1 41991 11955 mobile-phone Apple iPhone 6 Plus 16GB Gold 755.3 1 41983 11961 mobile-phone Apple iPhone 6 Plus 16GB Silver 731.6 1 41989 11958 mobile-phone Apple iPhone 6 Plus 16GB Space Grey 735.6 1 41986 11956 mobile-phone Apple iPhone 6 Plus 64GB Gold 843.1 1 41984 11962 mobile-phone Apple iPhone 6 Plus 64GB Silver 841.8 1 41990 11959 mobile-phone Apple iPhone 6 Plus 64GB Space Grey 840.5 1 41987 12733 mobile-phone ASUS ZenFone 2 ZE550ML Dual SIM -

Electronic 3D Models Catalogue (On July 26, 2019)
Electronic 3D models Catalogue (on July 26, 2019) Acer 001 Acer Iconia Tab A510 002 Acer Liquid Z5 003 Acer Liquid S2 Red 004 Acer Liquid S2 Black 005 Acer Iconia Tab A3 White 006 Acer Iconia Tab A1-810 White 007 Acer Iconia W4 008 Acer Liquid E3 Black 009 Acer Liquid E3 Silver 010 Acer Iconia B1-720 Iron Gray 011 Acer Iconia B1-720 Red 012 Acer Iconia B1-720 White 013 Acer Liquid Z3 Rock Black 014 Acer Liquid Z3 Classic White 015 Acer Iconia One 7 B1-730 Black 016 Acer Iconia One 7 B1-730 Red 017 Acer Iconia One 7 B1-730 Yellow 018 Acer Iconia One 7 B1-730 Green 019 Acer Iconia One 7 B1-730 Pink 020 Acer Iconia One 7 B1-730 Orange 021 Acer Iconia One 7 B1-730 Purple 022 Acer Iconia One 7 B1-730 White 023 Acer Iconia One 7 B1-730 Blue 024 Acer Iconia One 7 B1-730 Cyan 025 Acer Aspire Switch 10 026 Acer Iconia Tab A1-810 Red 027 Acer Iconia Tab A1-810 Black 028 Acer Iconia A1-830 White 029 Acer Liquid Z4 White 030 Acer Liquid Z4 Black 031 Acer Liquid Z200 Essential White 032 Acer Liquid Z200 Titanium Black 033 Acer Liquid Z200 Fragrant Pink 034 Acer Liquid Z200 Sky Blue 035 Acer Liquid Z200 Sunshine Yellow 036 Acer Liquid Jade Black 037 Acer Liquid Jade Green 038 Acer Liquid Jade White 039 Acer Liquid Z500 Sandy Silver 040 Acer Liquid Z500 Aquamarine Green 041 Acer Liquid Z500 Titanium Black 042 Acer Iconia Tab 7 (A1-713) 043 Acer Iconia Tab 7 (A1-713HD) 044 Acer Liquid E700 Burgundy Red 045 Acer Liquid E700 Titan Black 046 Acer Iconia Tab 8 047 Acer Liquid X1 Graphite Black 048 Acer Liquid X1 Wine Red 049 Acer Iconia Tab 8 W 050 Acer -

Phone Compatibility
Phone Compatibility • Compatible with iPhone models 4S and above using iOS versions 7 or higher. Last Updated: February 14, 2017 • Compatible with phone models using Android versions 4.1 (Jelly Bean) or higher, and that have the following four sensors: Accelerometer, Gyroscope, Magnetometer, GPS/Location Services. • Phone compatibility information is provided by phone manufacturers and third-party sources. While every attempt is made to ensure the accuracy of this information, this list should only be used as a guide. As phones are consistently introduced to market, this list may not be all inclusive and will be updated as new information is received. Please check your phone for the required sensors and operating system. Brand Phone Compatible Non-Compatible Acer Acer Iconia Talk S • Acer Acer Jade Primo • Acer Acer Liquid E3 • Acer Acer Liquid E600 • Acer Acer Liquid E700 • Acer Acer Liquid Jade • Acer Acer Liquid Jade 2 • Acer Acer Liquid Jade Primo • Acer Acer Liquid Jade S • Acer Acer Liquid Jade Z • Acer Acer Liquid M220 • Acer Acer Liquid S1 • Acer Acer Liquid S2 • Acer Acer Liquid X1 • Acer Acer Liquid X2 • Acer Acer Liquid Z200 • Acer Acer Liquid Z220 • Acer Acer Liquid Z3 • Acer Acer Liquid Z4 • Acer Acer Liquid Z410 • Acer Acer Liquid Z5 • Acer Acer Liquid Z500 • Acer Acer Liquid Z520 • Acer Acer Liquid Z6 • Acer Acer Liquid Z6 Plus • Acer Acer Liquid Zest • Acer Acer Liquid Zest Plus • Acer Acer Predator 8 • Alcatel Alcatel Fierce • Alcatel Alcatel Fierce 4 • Alcatel Alcatel Flash Plus 2 • Alcatel Alcatel Go Play • Alcatel Alcatel Idol 4 • Alcatel Alcatel Idol 4s • Alcatel Alcatel One Touch Fire C • Alcatel Alcatel One Touch Fire E • Alcatel Alcatel One Touch Fire S • 1 Phone Compatibility • Compatible with iPhone models 4S and above using iOS versions 7 or higher. -

Box Price Oppo A37 16Gb 650,000 550,000 350,000
Harga Sesuai Grade Box Brand Model Memory Price A B C D Oppo A37 16gb 650,000 550,000 350,000 200,000 50,000 Oppo A39 32gb 700,000 600,000 400,000 250,000 50,000 Oppo F1 PLUS 64gb 900,000 800,000 500,000 300,000 50,000 Oppo F1S 32gb 850,000 750,000 500,000 300,000 50,000 Oppo F1S 64gb 850,000 750,000 500,000 300,000 50,000 Oppo F3 64gb 1,050,000 850,000 550,000 350,000 100,000 Oppo F5 32gb 1,100,000 1,000,000 600,000 350,000 100,000 Oppo F5 64gb 1,100,000 1,000,000 600,000 350,000 100,000 Oppo F7 64gb 1,500,000 1,250,000 850,000 500,000 100,000 Oppo F7 128gb 1,500,000 1,250,000 850,000 500,000 100,000 Oppo F9 64gb 1,750,000 1,500,000 1,300,000 700,000 100,000 Galaxy A3 (2016) Single Samsung 16gb SIM 650,000 550,000 350,000 200,000 50,000 Samsung Galaxy A3 (2016) 16gb 650,000 550,000 350,000 200,000 50,000 Galaxy A5 (2016) Single Samsung 16gb SIM 800,000 700,000 500,000 300,000 50,000 Samsung Galaxy A5 (2016) 16gb 800,000 700,000 500,000 300,000 50,000 Samsung Galaxy A5 (2017) 32gb 1,100,000 1,000,000 600,000 400,000 100,000 Galaxy A5 (2017) Single Samsung 32gb SIM 1,100,000 1,000,000 600,000 400,000 100,000 Samsung Galaxy A6 (2018) 32gb 1,100,000 1,000,000 600,000 400,000 100,000 Samsung Galaxy A6 plus (2018) 32gb 1,500,000 1,400,000 900,000 600,000 100,000 Galaxy A7 (2016) Single Samsung 16gb Sim 950,000 850,000 550,000 300,000 50,000 Samsung Galaxy A7 (2016) 16gb 950,000 850,000 550,000 300,000 50,000 Samsung Galaxy A7 (2017) 32gb 1,200,000 1,100,000 650,000 400,000 100,000 Galaxy A7 (2017) Single Samsung 32gb SIM 1,200,000 1,100,000 -
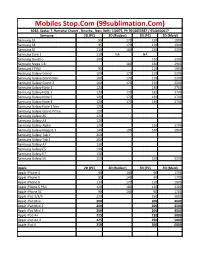
Mobiles Stop.Com (99Sublimation.Com)
Mobiles Stop.Com (99sublimation.Com) B282, Sector 7, Ramphal Chowk , Dwarka , New Delhi 110075, Ph 9910053987 / 9540300017 Samsung 2D (PC) 2D (Rubber) 3D (PC) 3D (Mold) Samsung S3 95 170 110 1900 Samsung S4 95 170 110 1900 Samsung S5 110 180 120 2200 Samsung Core 2 110 NA NA Samsung Quattro 100 120 2200 Samsung Mega 5.8 180 130 2900 Samsung S7562 95 110 1900 Samsung Galaxy Grand 100 170 110 2200 Samsung Galaxy Grand Neo 100 170 110 2200 Samsung Galaxy Grand 2 100 170 110 2200 Samsung Galaxy Note 1 120 130 2700 Samsung Galaxy Note 2 120 170 130 2700 Samsung Galaxy Note 3 120 170 130 2700 Samsung Galaxy Note 4 120 170 130 2700 Samsung Galaxy Note 3 Neo 120 Samsung Galaxy Grand Prime 120 Samsung Galaxy A5 120 Samsung Galaxy A3 120 Samsung Galaxy Alpha 120 130 2700 Samsung Galaxy Mega 6.3 140 190 140 2900 Samsung Galaxy Tab 2 200 Samsung Galaxy Tab 3 200 Samsung Galaxy A7 130 Samsung Galaxy E5 130 Samsung Galaxy E7 130 Samsung Galaxy S6 150 150 3200 Apple 2D (PC) 2D (Rubber) 3D (PC) 3D (Mold) Apple iPhone 4 90 140 90 1700 Apple iPhone 5 90 140 90 1700 Apple iPhone 6 110 170 110 1900 Apple iPhone 6 Plus 120 180 120 2200 Apple iPhone 5C 90 140 90 1700 Apple iPad 2/3/4 220 250 5000 Apple iPad Mini 200 200 4500 Apple iPad Mini 2 200 200 4500 Apple iPad Mini 3 200 200 4500 Apple iPad Air 225 250 5000 Apple iPad Air 2 225 250 5000 Apple iPad 6 250 300 6000 LG 2D (PC) 2D (Rubber) 3D (PC) 3D (Mold) LG G2 130 130 2700 LG G3 130 130 2700 LG L70 120 LG L90 120 LG Nexus 4 110 LG Nexus 5 110 110 2200 HTC HTC Desire 816 130 140 2900 HTC Desire 820 140 -

Offer Terms & Conditions • This Promotional Offer Is Only Available
Offer Terms & Conditions This promotional offer is only available to customers purchasing select models of smartphones (list available below) from Amazon.in between Aug 10th, 2015 and Aug 12th, 2015. In addition, this offer is only available to Amazon.in customers (i) located in India, (ii) that have set India as their country of record in their Amazon.in account settings, (iii) with a billing address in India and (iv) who have accepted the Amazon.in Kindle Store Terms of Use. Any customer attempting to redeem this promotion from outside of India (or from a device with a non-India IP address) are not eligible for this offer. By August 15, 2015 eligible participants will receive the promotion code to buy eBooks worth Rs.300 This is a limited time offer and the promotional credit will expire on September 9th, 2015 The promotional credit may only be applied to Kindle eBook titles sold and delivered by be Amazon Digital South Asia Inc. Offer limited to one promotional credit per qualifying device purchase. Promotional supplies are limited. Promotional credit will be allocated proportionally among all qualifying items in your order. If any of the products or content related to this offer are returned, your refund will equal the amount you paid for the product or content, subject to applicable refund policies. Standard terms and conditions, including the Amazon.in Conditions of Use and Sale and Privacy Notice, apply to this promotion, use of the Amazon.in website and the Kindle reading apps. The promotional credit is non-transferable, not exchangeable or redeemable for cash or other goods or services and may not be combined with other credits or special offers. -

Mobile Mcode 3D Cover Mold Apple Iphone 4-EM02 EM01 Yes 0 Apple Iphone 4S-EM01 EM02 Yes 0 Apple Iphone 5/5S/SE-EM04 EM03 Yes
ExclusiveBay Solutions More than 500 models of 3D Sublimation Mobile Covers, Molds, Silicon Whatsapp or Call +91-8199993691, +91-8587095427 Mobile Mcode 3D Cover Mold Apple Iphone 4-EM02 EM01 Yes 0 Apple Iphone 4S-EM01 EM02 Yes 0 Apple Iphone 5/5s/SE-EM04 EM03 Yes 0 Apple Iphone 5S/5/SE-EM03 EM04 Yes 0 Apple Iphone 6-EM06 EM05 Yes 0 Apple Iphone 6S-EM05 EM06 Yes 0 Samsung Galaxy J7 (2015) EM08 Yes 0 Samsung Galaxy J1 (2015) EM09 Yes Yes Samsung Galaxy J5 (2016) EM10 Yes Yes Samsung Galaxy J5 (2015) EM11 Yes 0 Samsung Galaxy J2 (2016)-EM96 EM12 Yes 0 Samsung Galaxy J2 (2015) EM13 Yes 0 Xiaomi Redmi Note 3 EM14 Yes 0 Samsung Galaxy J7 (2016) EM15 Yes 0 Xiaomi Mi 5 EM16 Yes 0 Xiaomi Mi 4 EM17 Yes Yes Xiaomi Mi 4i EM18 Yes 0 Samsung Galaxy E5(E500) (2016) EM19 Yes 0 Samsung Galaxy E7(E700) (2016) EM20 Yes 0 Motorola Moto X Play EM21 Yes 0 Motorola Moto G Turbo-EM24-EM29 EM22 Yes 0 Motorola Moto X Style EM23 Yes 0 Motorola Moto Turbo-EM22-EM29 EM24 Yes 0 Motorola Moto X Force-EM563 EM25 Yes 0 Motorola Moto X 2nd Gen EM26 Yes 0 Motorola Moto G 1st Gen EM27 Yes 0 Motorola Moto G 2nd Gen EM28 Yes Yes Motorola Moto G 3rd Gen-EM22 EM29 Yes 0 Motorola Moto E 1st Gen EM30 Yes Yes Lenovo Vibe K5-EM45 EM31 Yes Yes Lenovo Vibe K4 Note/A7010-EM272 EM32 Yes 0 Lenovo A2010 4G-EM606/441 EM34 Yes 0 Lenovo A7000/K3 Note-EM342 EM35 Yes 0 Huawei P9 EM36 Yes Yes LeEco (LeTV) Le 2 Pro-EM600 EM41 Yes Yes Lenovo K5 Note EM42 Yes 0 Lenovo Vibe K5 Plus-EM31 EM45 Yes 0 Lenovo Vibe P1 Turbo-EM343 EM46 Yes 0 LG G5 EM47 Yes 0 LG Stylus 2 Plus-EM577 EM48 Yes 0 Micromax -

Equipos De Préstamo
Equipos de préstamo TMCH entregará a clientes Empresas, sean estos representantes legales, interlocutores válidos y usuarios, que envíen sus equipos a reparar un equipo de préstamo similar en características al que posee. Esto es, según sistema operativo y tipo de Simcard. El equipo otorgado como préstamo se encuentra sujeto a disponibilidad de stock al momento del ingreso a reparación. Es obligatorio hacer la devolución de este móvil en buen estado al momento de recibir el equipo enviado a taller. Todos los equipos devueltos en mal estado o no devueltos según lo indicado anteriormente serán facturados según la gama del equipo entregado en préstamo de acuerdo a la siguiente tabla. PRECIO EQUIPO DESCRIPCIÓN MODELO PRESTAMO ALCATEL 1V METALLIC BLUE $ 63.990 XIAOMI REDMI 9A 32GB GRANITE GREY $ 111.990 SAMSUNG GALAXY S20 FE LAVENDER $ 479.990 SAMSUNG GALAXY S20 FE ORANGE $ 479.990 IPHONE XR 64GB WHITE $ 439.990 APPLE IPHONE 11 BLACK 64GB $ 527.990 SAMSUNG GALAXY S10+ PRISM WHITE $ 519.990 SAMSUNG GALAXY S10+ PRISM BLACK $ 519.990 SAMSUNG GALAXY A31 RED $ 215.990 SAMSUNG GALAXY A31 BLUE $ 215.990 IPHONE XR 64GB (PRODUCT) RED $ 439.990 APPLE IPH 11 64GB BLACK+WATCH 38 SL AL $ 751.990 APPLE IPHONE 11 PURPLE 64GB $ 527.990 IPHONE XR 64GB BLACK $ 439.990 HUAWEI P30 LITE TWILIGHT $ 263.990 HUAWEI P30 LITE BLACK $ 263.990 IPHONE XR 128GB BLACK $ 543.990 IPAD PRO 12.9 4TH WIFI+CELL SILVER 128GB $ 983.990 IPAD PRO 12.9 4TH WIFI SPACE GRAY 128GB $ 847.990 IPAD PRO 11 2TH WIFI+CELL SILVER 128GB $ 823.990 IPAD PRO 11 2TH WIFI+CEL SPACEGRAY 128GB $ 823.990 -

MODELS Redmi Mi4i Samsung Mi5 Samsung Galaxy S2 Redmi 1S Samsung Galaxy S3 Redmi 2S Samsung Galaxy S4 Redmi 3S Samsung Galaxy S5
3D MOBILE CASE BLANK MODEL LIST (UPDATED ON 20TH SEPT 2015) MODELS Redmi Mi4i Samsung Mi5 Samsung Galaxy S2 Redmi 1S Samsung Galaxy S3 Redmi 2S Samsung Galaxy S4 Redmi 3S Samsung Galaxy S5 Redmi Note / Note 4G Samsung Galaxy S6 Redmi Note 2 (2nd Gen) Samsung Galaxy S6 Edge Redmi 2A Samsung Galaxy S6 Edge Plus Lenovo Samsung Galaxy S3 Mini Lenovo Vibe Z K910 Samsung Galaxy S4 Mini Lenovo Vibe Z2 Pro K920 Samsung Galaxy S5 Mini Lenovo A6000 Samsung Galaxy Grand Lenovo A6000 Plus Samsung Galaxy Grand Neo Lenovo A7000 Samsung Galaxy Grand Neo Plus Lenovo K3 Note Samsung Galaxy Grand 2 Micromax Samsung Galaxy Grand Prime Micromax Knight A350 Samsung Galaxy Grand 3 Micromax Unite 2 A106 Samsung Galaxy Grand Max MIcromax Unite 3 Q372 Samsung Galaxy Note 1 Micromax A110/A110Q Samsung Galaxy Note 2 Micromax HD A116 Samsung Galaxy Note 3 Micromax Magnus A117 Samsung Galaxy Note 3 Neo Micromax YU Yurekha Samsung Galaxy Note 4 Micromax YU Yuphoria Samsung Note Edge/ Note 4 Edge Micromax Android A1 Samsung Galaxy Note 5 Micromax Canvas Spark Q380 Samsung Galaxy Note 5 Edge Micromax Canvas Fire 4 A107 Samsung Galaxy Mega 5.8 Micromax Canvas Nitro 2 E311 Samsung Galaxy Mega 6.3 Micromax Canvas Sliver 5 Q450 Samsung Galaxy Alpha Micromax Canvas Express 2 E313 Samsung Galaxy A3 One Plus Samsung Galaxy A5 One Plus One Samsung Galaxy A7 One Plus Two Samsung Galaxy A8 Asus Samsung Galaxy E5 Asus Zenfone 2 Samsung Galaxy E7 Asus Zenfone 5 Samsung Galaxy Ace 3 Asus Zenfone 6 Samsung Galaxy S Duos S7562 Asus Zenfone Selfie Samsung Galaxy S Duos S7582 Asus Zenfone -

The Use of Mobile Phone Camera in Close Range Photogrammetry
Palestine Polytechnic University College of Engineering Civil & Architectural Engineering Department Surveying and Geomatics Engineering Graduation Project The use of mobile phone camera in close range photogrammetry BY Ayat Abed Al Aziz Majdoleen Ayaydeh Mariam Abu Attalah Supervisor: DR. Ghadi Zakarneh Hebron-West Bank Palestine December-2015 اﻹهداء إلى شهداء الوطن الحبيب اللذين امتزجت دمائهم بثرى الوطن الحبيب ليرسمو الىطريق الحرية إلى القابعين خلف قضبان الحديد ينتظرون يوم الحرية إلى من أصبحت المستشفيات بيوتهم الثانية إلى أمي الغالية رفيقة دربي في ليالي السهر الطوال إلى أبي رمز العطاء الدائم المغني عن السؤال إلى كل من تحرك القلم في يده بخط كلمه خير تشرق بها شموس الفجر إلى الدموع السائلة ترقب الفجر القريب إليك يا وطن و إلى كل القلوب الصافية إلى إخواني وأخواتي وزمﻻئي و إلى كل من علم حرفا وإلى كل من ساهم في انجاح هذا المشروع فريق العمل I Acknowledgment Thanks God ( Allah) , the most Merciful who granted us the ability and willing to start this project. Thanks our University and Department of civil and architectural engineering. We express our thanks to Dr. Ghadi Zakarneh who gave us knowledge, valuable help, encouragement, supervision and guidance in solving the problems that we faced from time to time during this project. Finally our deep sense and sincere thanks to our parents, brothers and sisters for their patience, also for ever one who helped us during our work and gave us strength to complete this task especially to Shoroq Swiety. II Abstract The use of mobile phone camera in close range photogrammetry Abstract The project aims to use the simple technology owned by anyone for close range photogrammetric applications by using different mobile phone cameras in different levels of resolution. -

Daftar Harga Trade-In Kisaran Harga Perangkat Lama Anda Dapat Berubah Sesuai Dengan Kondisi Perangkat Lama Anda
Daftar Harga Trade-in www.samsung.com/id Kisaran harga perangkat lama Anda dapat berubah sesuai dengan kondisi perangkat lama Anda Harga Tertinggi Perangkat Brand Tipe Smartphone Lama Anda Asus Asus Selfie Zd551KlRp 300.000 Asus Asus Zenfone 2 Ze551MlRp 300.000 Asus Asus Zenfone 3 Max Zc520TlRp 450.000 Asus Asus Zenfone 3 Ze520KlRp 550.000 Asus Asus Zenfone 3 Ze552KlRp 650.000 Asus Asus Zenfone 4 Max Zc554Kl 32GbRp 450.000 Asus Asus Zenfone 5 Ze620KlRp 1.300.000 Asus Asus Zenfone 5Z Zs620Kl 128GbRp 1.950.000 Asus Asus Zenfone Live (L1) Za550KlRp 450.000 Asus Asus Zenfone Max (M1) Zb555KlRp 650.000 Asus Asus Zenfone Max Pro M1 Zb601Kl 32GbRp 850.000 Asus Asus Zenfone Max Pro M1 Zb601Kl 64GbRp 950.000 Asus Asus Zenfone Max Pro M2 Zb631KlRp 1.100.000 Asus Asus Zenfone Max Zc553KlRp 400.000 Blackberry Blackberry Aurora 32GbRp 450.000 Blackberry Blackberry Keyone 64GbRp 1.350.000 Google Google Pixel XlRp 1.050.000 Huawei Huawei Mate 20 ProRp 2.700.000 Huawei Huawei Nova 3I 128GbRp 1.100.000 Huawei Huawei P30Rp 3.850.000 Huawei Huawei P30 LiteRp 1.650.000 Huawei Huawei P30 ProRp 6.050.000 Lenovo Lenovo A7000 PlusRp 300.000 Lenovo Lenovo Vibe K4 NoteRp 350.000 Lenovo Lenovo Vibe P1Rp 350.000 LG Lg G4Rp 450.000 LG Lg G5 SeRp 500.000 Motorola Motorola Moto G5S PlusRp 550.000 Nokia Nokia Nokia 2.2Rp 600.000 Nokia Nokia Nokia 3Rp 400.000 Nokia Nokia Nokia 5.1 PlusRp 750.000 Nokia Nokia Nokia 6Rp 500.000 Nokia Nokia Nokia 6.1 PlusRp 1.000.000 Oppo Oppo A1KRp 850.000 Oppo Oppo A37Rp 550.000 Oppo Oppo A39Rp 600.000 Oppo Oppo A3SRp 950.000 Oppo Oppo -

Daftar-Harga-Tradein-Samsung.Com
Daftar Harga Trade-in www.samsung.com/id Kisaran harga perangkat lama Anda dapat berubah sesuai dengan kondisi perangkat lama Anda Brand Type Harga Max Perangkat Lama Anda Acer Acer Iconia Tab A701Rp 50.000 Acer Acer Liquid E3Rp 350.000 Acer Acer Liquid E700 Triple SimRp 100.000 Acer Acer Liquid JadeRp 200.000 Acer Acer Liquid S1Rp 200.000 Acer Acer Liquid Z160Rp 200.000 Acer Acer Liquid Z2Rp 50.000 Acer Acer Liquid Z220Rp 150.000 Acer Acer Liquid Z320Rp 250.000 Acer Acer Liquid Z500Rp 250.000 Acer Acer Liquid Z520Rp 150.000 Advan Advan Advan I5Rp 250.000 Advan Advan Advan I5CRp 100.000 Advan Advan Advan S4ZRp 200.000 Advan Advan Advan S5ERp 150.000 AdvanAdvan M6Rp 200.000 AdvanAdvan Tab 7Rp 350.000 Advan Advan Vandroid S50KRp 50.000 Advan Advan Vandroid S5JRp 200.000 AdvanAdvan W80Rp 350.000 Alcatel Alcatel Alcatel C7Rp 150.000 Alcatel Alcatel Alcatel Pixi 4Rp 200.000 Asus Asus Asus Zenpad 7.0Rp 250.000 Asus Asus Fonepad 7 Fe170CgRp 100.000 Asus Asus Fonepad 7 Fe375CgRp 200.000 Asus Asus Padfone InfinityRp 500.000 Asus Asus Padfone MiniRp 450.000 Asus Asus Padfone SRp 300.000 Asus Asus Rog Phone Zs600Kl 128GbRp 3.300.000 Asus Asus Rog Phone Zs600Kl 512GbRp 3.950.000 Asus Asus Selfie Zd551KlRp 350.000 Asus Asus Zenfone 2 Laser Ze500KgRp 250.000 Asus Asus Zenfone 2 Laser Ze500KlRp 250.000 Asus Asus Zenfone 2 Laser Ze550KlRp 250.000 Asus Asus Zenfone 2 Laser Ze551Kl 16GbRp 50.000 Asus Asus Zenfone 2 Laser Ze551Kl 32GbRp 50.000 Asus Asus Zenfone 2 Ze500ClRp 200.000 Asus Asus Zenfone 2 Ze550MlRp 200.000 Asus Asus Zenfone 2 Ze551MlRp 350.000