Fracture Management “Oh Snap!”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical Policy Ultrasound Accelerated Fracture Healing Device
Medical Policy Ultrasound Accelerated Fracture Healing Device Table of Contents Policy: Commercial Coding Information Information Pertaining to All Policies Policy: Medicare Description References Authorization Information Policy History Policy Number: 497 BCBSA Reference Number: 1.01.05 Related Policies Electrical Stimulation of the Spine as an Adjunct to Spinal Fusion Procedures, #498 Electrical Bone Growth Stimulation of the Appendicular Skeleton, #499 Bone Morphogenetic Protein, #097 Policy Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Members Low-intensity ultrasound treatment may be MEDICALLY NECESSARY when used as an adjunct to conventional management (i.e., closed reduction and cast immobilization) for the treatment of fresh, closed fractures in skeletally mature individuals. Candidates for ultrasound treatment are those at high risk for delayed fracture healing or nonunion. These risk factors may include either locations of fractures or patient comorbidities and include the following: Patient comorbidities: Diabetes, Steroid therapy, Osteoporosis, History of alcoholism, History of smoking. Fracture locations: Jones fracture, Fracture of navicular bone in the wrist (also called the scaphoid), Fracture of metatarsal, Fractures associated with extensive soft tissue or vascular damage. Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of delayed union of bones, including delayed union** of previously surgically-treated fractures, and excluding the skull and vertebra. 1 Low-intensity ultrasound treatment may be MEDICALLY NECESSARY as a treatment of fracture nonunions of bones, including nonunion*** of previously surgically-treated fractures, and excluding the skull and vertebra. Other applications of low-intensity ultrasound treatment are INVESTIGATIONAL, including, but not limited to, treatment of congenital pseudarthroses, open fractures, fresh* surgically-treated closed fractures, stress fractures, arthrodesis or failed arthrodesis. -

Greenstick Fracture Soft Cast No FU
Orthopaedic Department York Teaching Hospital This is a follow-up letter to your recent telephone consultation with the fracture care team explaining the ongoing management of your injury. Your case has been reviewed by an Orthopaedic Consultant (Bone Specialist) and Fracture Care Physiotherapist. You have sustained a greenstick fracture to your distal radius and/or ulna (forearm just before the wrist). This is a specific type of fracture that occurs in children’s bones Healing: This normally takes approximately 4 - 6 weeks to heal. It is normal for it to continue to ache a bit for a few weeks after this. Pain and swelling: Take pain killers as needed. The plaster backslab helps healing by keeping the bones in a good position. Elevate the arm to reduce swelling for the first few days Using your arm: You may use the arm as pain allows. It is important to keep the elbow moving to prevent stiffness. Follow up: There is a small chance that this fracture can displace (move). Therefore we routinely recommend a repeat x ray at 1 week after the injury and a new plaster cast. Arrangements for this appointment should have been made during your telephone consultation. Should you need to reschedule this appointment please see contact details at the top of this letter. Area of injury: If you are worried that you are unable to follow this rehabilitation plan, Or, if you are experiencing pain or symptoms, other than at the site of the original injury or surrounding area, or have any questions, then please phone the Fracture Care Team for advice. -
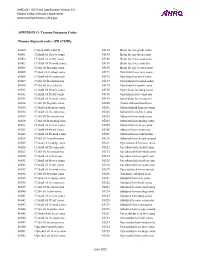
PSI Appendix G Version 6.0 Patient Safety Indicators Appendices
AHRQ QI™ ICD-9-CM Specification Version 6.0 Patient Safety Indicators Appendices www.qualityindicators.ahrq.gov APPENDIX G: Trauma Diagnosis Codes Trauma diagnosis codes: (TRAUMID) 80000 Closed skull vault fx 85184 Brain lac nec-proln coma 80001 Cl skull vlt fx w/o coma 85185 Brain lac nec-deep coma 80002 Cl skull vlt fx-brf coma 85186 Brain lacer nec-coma nos 80003 Cl skull vlt fx-mod coma 85189 Brain lacer nec-concuss 80004 Cl skl vlt fx-proln coma 85190 Brain lac nec w open wnd 80005 Cl skul vlt fx-deep coma 85191 Opn brain lacer w/o coma 80006 Cl skull vlt fx-coma nos 85192 Opn brain lac-brief coma 80009 Cl skl vlt fx-concus nos 85193 Opn brain lacer-mod coma 80010 Cl skl vlt fx/cerebr lac 85194 Opn brain lac-proln coma 80011 Cl skull vlt fx w/o coma 85195 Open brain lac-deep coma 80012 Cl skull vlt fx-brf coma 85196 Opn brain lacer-coma nos 80013 Cl skull vlt fx-mod coma 85199 Open brain lacer-concuss 80014 Cl skl vlt fx-proln coma 85200 Traum subarachnoid hem 80015 Cl skul vlt fx-deep coma 85201 Subarachnoid hem-no coma 80016 Cl skull vlt fx-coma nos 85202 Subarach hem-brief coma 80019 Cl skl vlt fx-concus nos 85203 Subarach hem-mod coma 80020 Cl skl vlt fx/mening hem 85204 Subarach hem-prolng coma 80021 Cl skull vlt fx w/o coma 85205 Subarach hem-deep coma 80022 Cl skull vlt fx-brf coma 85206 Subarach hem-coma nos 80023 Cl skull vlt fx-mod coma 85209 Subarach hem-concussion 80024 Cl skl vlt fx-proln coma 85210 Subarach hem w opn wound 80025 Cl skul vlt fx-deep coma 85211 Opn subarach hem-no coma 80026 Cl skull vlt fx-coma nos 85212 -

5Th Metatarsal Fracture
FIFTH METATARSAL FRACTURES Todd Gothelf MD (USA), FRACS, FAAOS, Dip. ABOS Foot, Ankle, Shoulder Surgeon Orthopaedic You have been diagnosed with a fracture of the fifth metatarsal bone. Surgeons This tyPe of fracture usually occurs when the ankle suddenly rolls inward. When the ankle rolls, a tendon that is attached to the fifth metatarsal bone is J. Goldberg stretched. Because the bone is weaker than the tendon, the bone cracks first. A. Turnbull R. Pattinson A. Loefler All bones heal in a different way when they break. This is esPecially true J. Negrine of the fifth metatarsal bone. In addition, the blood suPPly varies to different I. PoPoff areas, making it a lot harder for some fractures to heal without helP. Below are D. Sher descriPtions of the main Patterns of fractures of the fifth metatarsal fractures T. Gothelf and treatments for each. Sports Physicians FIFTH METATARSAL AVULSION FRACTURE J. Best This fracture Pattern occurs at the tiP of the bone (figure 1). These M. Cusi fractures have a very high rate of healing and require little Protection. Weight P. Annett on the foot is allowed as soon as the Patient is comfortable. While crutches may helP initially, walking without them is allowed. I Prefer to Place Patients in a walking boot, as it allows for more comfortable walking and Protects the foot from further injury. RICE treatment is initiated. Pain should be exPected to diminish over the first four weeks, but may not comPletely go away for several months. Follow-uP radiographs are not necessary if the Pain resolves as exPected. -

BSUH VFC Initial Management Guidelines Dec 2014
BSUH VFC initial management guidelines Dec 2014 Contents Page Elbow injuries: Radial head / Radial neck fractures 3 Elbow dislocations 3 Shoulder Injuries: Shoulder dislocation 4 ACJ dislocation 4 Proximal Humerus fractures 5 Greater Tuberosity fractures 5 Midshaft Humerus 6 Mid-shaft clavicle fractures 7 Lateral 1/3 Clavicle fractures 8 Medial 1/3 clavicle fractures 9 Soft tissue injury shoulder 11 Calcific tendinitis 11 Common lower limb injuries Foot injuries: 5th Metatarsal fracture 12 Stress fractures 12 5th Midshaft fractures 12 Single Metatarsal fractures 12 Single phalanx fractures 12 Multiple Metatarsal fractures 13 Mid-foot fractures 13 Calcaneal fractures 14 Ankle injuries: Page 1 of 18 Weber A ankle fractures 15 Weber B 15 Weber C 15 Medial malleolus / and Posterior malleolus fractures 15 Bi-tri malleolus fractures 16 Soft tissue ankle injury / Avulsion lateral malleolus 16 TA ruptures 16 Knee injuries Locked Knee 17 Soft tissue knee injury 17 Patella Dislocation 17 Patella fractures 17 Possible Tumours 18 Page 2 of 18 Upper Limb Injuries Elbow injuries Radial head / neck fractures Mason 1 head / borderline Mason 1-2 protocol BAS for comfort only 2/52 and early gentle ROM DC VFC. Patient to contact VFC at 3/52 post injury if struggling to regain ROM Mason 2 >2mm articular step off discuss case with consultant on hot week likely conservative management if unsure d/w upper limb consultants opinion for 2/52 repeat x-ray and review in VFC Mason 3 head # or >30degrees neck angulation = Urgent Ref to UL clinic (LL or LT) for discussion with regards to surgical management. -

Management of Pediatric Forearm Torus Fractures: a Systematic
ORIGINAL ARTICLE Management of Pediatric Forearm Torus Fractures A Systematic Review and Meta-Analysis Nan Jiang, MD,*† Zhen-hua Cao, MD,*‡ Yun-fei Ma, MD,*† Zhen Lin, MD,§ and Bin Yu, MD*† many disadvantages, such as heavy, bulky, and requires a second Objectives: Pediatric forearm torus fracture, a frequent reason for emer- visit to the hospital for removal. These flaws of cast may bring gency department visits, can be immobilized by both rigid cast and non- inconvenience to children as well as their families. In recent years, rigid methods. However, controversy still exists regarding the optimal many pediatric clinicians reported other methods to instead tradi- treatment of the disease. The aim of this study was to compare, in a system- tionally used cast, including soft cast,9,10 Futuro wrist splint,8,11 atic review, clinical efficacy of rigid cast with nonrigid methods for immo- and double Tubigrip.11 Although patients that suffered from fore- bilization of the pediatric forearm torus fractures. arm torus fractures can be immobilized by both rigid cast and non- Methods: Literature search was performed of PubMed and Cochrane Li- rigid materials, controversy still exists in the optimal treatment of brary by 2 independent reviewers to identify randomized controlled trials this fracture. comparing rigid cast with nonrigid methods for pediatric forearm torus The aim of this study was to, in a systematic review and fractures from inception to December 31, 2013, without limitation of publi- meta-analysis, compare clinical efficacy of recently used nonrigid cation language. Trial quality was assessed using the modified Jadad scale. immobilization methods with rigid cast. -

Vanderbilt Sports Medicine
Alabama AAP Fall Meeting Sept.19-20, 2009 Pediatric Fracture Care for the Pediatrician Andrew Gregory, MD, FAAP, FACSM Assistant Professor Orthopedics & Pediatrics Program Director, Sports Medicine Fellowship Vanderbilt University Vanderbilt Sports Medicine Disclosure No conflict of interest - unfortunately for me, I have no financial relationships with companies making products regarding this topic to disclose Objectives Review briefly the differences of pediatric bone Review Pediatric Fracture Classification Discuss subtle fractures in kids Discuss a few other pediatric only conditions 1 Pediatric Skeleton Bone is relatively elastic and rubbery Periosteum is quite thick & active Ligaments are strong relative to the bone Presence of the physis - “weak link” Ligament injuries & dislocations are rare – “kids don’t sprain stuff” Fractures heal quickly and have the capacity to remodel Anatomy of Pediatric Bone Epiphysis Physis Metaphysis Diaphysis Apophysis Pediatric Fracture Classification Plastic Deformation – Bowing usually of fibula or ulna Buckle/ Torus – compression, stable Greenstick – unicortical tension Complete – Spiral, Oblique, Transverse Physeal – Salter-Harris Apophyseal avulsion 2 Plastic deformation Bowing without fracture Often deformed requiring reduction Buckle (Torus) Fracture Buckled Periosteum – Metaphyseal/ diaphyseal junction Greenstick Fracture Cortex Broken on Only One Side – Incomplete 3 Complete Fractures Transverse – Perpendicular to the bone Oblique – Across the bone at 45-60 o – Unstable Spiral – Rotational -

Pediatric Orthopedic Injuries… … from an ED State of Mind
Traumatic Orthopedics Peds RC Exam Review February 28, 2019 Dr. Naminder Sandhu, FRCPC Pediatric Emergency Medicine Objectives to cover today • Normal bone growth and function • Common radiographic abnormalities in MSK diseases • Part 1: Atraumatic – Congenital abnormalities – Joint and limb pain – Joint deformities – MSK infections – Bone tumors – Common gait disorders • Part 2: Traumatic – Common pediatric fractures and soft tissue injuries by site Overview of traumatic MSK pain Acute injuries • Fractures • Joint dislocations – Most common in ED: patella, digits, shoulder, elbow • Muscle strains – Eg. groin/adductors • Ligament sprains – Eg. Ankle, ACL/MCL, acromioclavicular joint separation Chronic/ overuse injuries • Stress fractures • Tendonitis • Bursitis • Fasciitis • Apophysitis Overuse injuries in the athlete WHY do they happen?? Extrinsic factors: • Errors in training • Inappropriate footwear Overuse injuries Intrinsic: • Poor conditioning – increased injuries early in season • Muscle imbalances – Weak muscle near strong (vastus medialus vs lateralus patellofemoral pain) – Excessive tightness: IT band, gastroc/soleus Sever disease • Anatomic misalignments – eg. pes planus, genu valgum or varum • Growth – strength and flexibility imbalances • Nutrition – eg. female athlete triad Misalignment – an intrinsic factor Apophysitis • *Apophysis = natural protruberance from a bone (2ndary ossification centres, often where tendons attach) • Examples – Sever disease (Calcaneal) – Osgood Schlatter disease (Tibial tubercle) – Sinding-Larsen-Johansson -

Ankle Injuries
Pediatric Fractures of the Ankle Nicholas Frane DO Zucker/Hofstra School of Medicine Northwell Health Core Curriculum V5 Disclosure • Radiographic Images Courtesy of: Dr. Jon-Paul Dimauro M.D or Christopher D Souder, MD, unless otherwise specified Core Curriculum V5 Outline • Epidemiology • Anatomy • Classification • Assessment • Treatment • Outcomes Core Curriculum V5 Epidemiology • Distal tibial & fibular physeal injuries 25%-38% of all physeal fractures • Ankle is the 2nd most common site of physeal Injury in children • Most common mechanism of injury Sports • 58% of physeal ankle fractures occur during sports activities • M>F • Commonly seen in 8-15y/o Hynes D, O'Brien T. Growth disturbance lines after injury of the distal tibial physis. Their significance in prognosis. J Bone Joint Surg Br. 1988;70:231–233 Zaricznyj B, Shattuck LJ, Mast TA, et al. Sports-related injuries in school-aged children. Am J Sports Med. 1980;8:318–324. Core Curriculum V5 Epidemiology Parikh SN, Mehlman CT. The Community Orthopaedic Surgeon Taking Trauma Call: Pediatric Ankle Fracture Pearls and Pitfalls. J Orthop Trauma. 2017;31 Suppl 6:S27-S31. doi:10.1097/BOT.0000000000001014 Spiegel P, et al. Epiphyseal fractures of the distal ends of the tibia and fibula. J Bone Joint Surg Am. 1978;60(8):1046-50. Core Curriculum V5 Anatomy • Ligamentous structures attach distal to the physis • Growth plate injury more likely than ligament failure secondary to tensile weakness in physis • Syndesmosis • Anterior Tibio-fibular ligament (AITFL) • Posterior Inferior Tibio-fibular -

Torus (Buckle) Fracture Discharge Advice
Torus (Buckle) Fracture Discharge Advice Information for you Follow us on Twitter @NHSaaa Find us on Facebook at www.facebook.com/nhsaaa Visit our website: www.nhsaaa.net All our publications are available in other formats What has happened? Your child has sustained a torus fracture, also known as a “buckle” fracture, of the radius and/or ulna (the long bones at the wrist). The bone “buckles” on one side rather than actually breaks and is commonly seen in children as their bones are soft and flexible. Will my child need a cast? Torus fractures heal well without any long-term complications. They do not require any operations or to be placed in a cast. However, using a wrist splint provides comfort and reduces the risk of further injury. It should be worn at all times but can be removed for washing and showering without any risk to the fracture. Simple painkillers such as paracetamol and/or ibuprofen can also be used to reduce discomfort. How long should my child wear the splint for? In general, the older the child is, the longer they will need to wear the splint. We recommend that children under five years old should wear the splint for one week, those age five to ten years should wear it for two weeks and those over ten years should wear it for three weeks. If your child removes the splint before this time but is comfortable and moving their wrist freely then there is no need to insist that they wear the splint for longer. However, if your child is still sore and reluctant to use their wrist when the splint is removed, then you 2 may reapply the splint. -

Musculoskeletal System Imaging
SUMPh “N. Testemitanu” Radiology and Medical imaging department MUSCULOSKELETAL SYSTEM IMAGING M. Crivceanschii, assistant professor GOALS AND OBJECTIVES • to be aware of the role of modern diagnostic imaging modalities • to be familiar with main radiological signs and syndromes • tips and tricks in musculoskeletal imaging IMAGING MODALITIES • that every student should now IMAGING MODALITIES • Conventional Radiography • Fluoroscopy • Arthrography • Computed Tomography • Magnetic Resonance Imaging • Ultrasound • Scintigraphy PLAIN X-RAY FILM • First line study for most medical issues • Excellent for fractures/bony detail • Very limited for soft tissues (ligaments, tendons, muscles) • Only a screening tool in the spine • The radiologist should obtain at least two (2) views of the bone involved at 90° angles to each other • with each view including two adjacent joints FLUOROSCOPY • Arthrography • Tenography • Arteriography • Percutaneous Bone or Soft Tissue Biopsy CT SCANNING • Excellent for bony structural anatomy in the setting of complicated fracture • Less effective than MR for soft tissues and active processes • High radiation Dose • Interventional options MRI SCANNING • Excellent for soft tissue pathology • Good-excellent for bone pathology • No ionizing radiation • NOT patient friendly • Some absolute and relative contraindications ULTRASOUND • Reproducible in trained hands • Excellent for superficial soft tissue elements including tendons and muscles • No ionizing radiation • Patient friendly SCINTIGRAPHY • Image the entire skeleton at once • It provides a metabolic picture • It is particularly helpful in condition such as fibrous dysplasia, Langerhans Cell Histocytosis or metastatic cancer. CONGENITAL SKELETAL ANOMALIES CONGENITAL SKELETAL ANOMALIES • Chromosomal disorders (e. g. Down’s syndrome, Marfan syndrome, Turner’s syndrome, etc.) • Dwarfism (rhizomelic – proximal segments shortening, mesomelic – middle segments, acromelic – distal segments) • Skeletal dysplasias (e. -

Basic Principles of Fracture Treatment in Children
Eklem Hastalıkları ve Eklem Hastalik Cerrahisi Cerrahisi 2018;29(1):52-57 Joint Diseases and Related Surgery Review / Derleme doi: 10.5606/ehc.2018.58165 Basic principles of fracture treatment in children Çocuklarda kırık tedavisinin temel prensipleri Hakan Ömeroğlu, MD1 Department of Orthopedics and Traumatology, TOBB University of Economics and Technology, Faculty of Medicine, Ankara, Turkey ABSTRACT ÖZ This review aims to summarize the basic treatment principles Bu derlemede çocuklarda tiplerine göre kırıkların temel of fractures according to their types and general management tedavi prensipleri ve fizis kırıkları, çoklu kırıklar, açık principles of special conditions including physeal fractures, kırıklar ve patolojik kırıkları içeren özel durumların genel multiple fractures, open fractures, and pathologic fractures yönetim prensipleri özetlendi. Yaralanma mekanizmasını in children. Definition of the fracture is needed for better daha iyi anlamak, uygun bir tedavi stratejisi belirlemek ve understanding the injury mechanism, planning a proper prognozu tahmin etmek için kırığın tanımlanması gereklidir. treatment strategy, and estimating the prognosis. As the İyileşme süreci daha az komplike, yeniden şekillenme healing process is less complicated, remodeling capacity is kapasitesi daha yüksek ve kaynamama seyrek olduğu için higher and non-union is rare, the fractures in children are çocuklarda kırıklar çoğunlukla cerrahi dışı yöntemlerle commonly treated by non-surgical methods. Surgical treatment tedavi edilir. Çoklu yaralanması olan