Eating Disorders [PDF]
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ICD-10 Mental Health Billable Diagnosis Codes in Alphabetical
ICD-10 Mental Health Billable Diagnosis Codes in Alphabetical Order by Description IICD-10 Mental Health Billable Diagnosis Codes in Alphabetic Order by Description Note: SSIS stores ICD-10 code descriptions up to 100 characters. Actual code description can be longer than 100 characters. ICD-10 Diagnosis Code ICD-10 Diagnosis Description F40.241 Acrophobia F41.0 Panic Disorder (episodic paroxysmal anxiety) F43.0 Acute stress reaction F43.22 Adjustment disorder with anxiety F43.21 Adjustment disorder with depressed mood F43.24 Adjustment disorder with disturbance of conduct F43.23 Adjustment disorder with mixed anxiety and depressed mood F43.25 Adjustment disorder with mixed disturbance of emotions and conduct F43.29 Adjustment disorder with other symptoms F43.20 Adjustment disorder, unspecified F50.82 Avoidant/restrictive food intake disorder F51.02 Adjustment insomnia F98.5 Adult onset fluency disorder F40.01 Agoraphobia with panic disorder F40.02 Agoraphobia without panic disorder F40.00 Agoraphobia, unspecified F10.180 Alcohol abuse with alcohol-induced anxiety disorder F10.14 Alcohol abuse with alcohol-induced mood disorder F10.150 Alcohol abuse with alcohol-induced psychotic disorder with delusions F10.151 Alcohol abuse with alcohol-induced psychotic disorder with hallucinations F10.159 Alcohol abuse with alcohol-induced psychotic disorder, unspecified F10.181 Alcohol abuse with alcohol-induced sexual dysfunction F10.182 Alcohol abuse with alcohol-induced sleep disorder F10.121 Alcohol abuse with intoxication delirium F10.188 Alcohol -

Title Steatitis and Vitamin E Deficiency in Captive Olive Ridley Turtles
Steatitis and Vitamin E deficiency in captive olive ridley turtles Title (Lepidochelys olivacea) MANAWATTHANA, SONTAYA; KASORNDORKBUA, Author(s) CHAIYAN Proceedings of the 2nd International symposium on Citation SEASTAR2000 and Asian Bio-logging Science (The 6th SEASTAR2000 Workshop) (2005): 85-87 Issue Date 2005 URL http://hdl.handle.net/2433/44090 Right Type Conference Paper Textversion publisher Kyoto University Steatitis and Vitamin E deficiency in captive olive ridley turtles (Lepidochelys olivacea) SONTAYA MANAWATTHANA1 and CHAIYAN KASORNDORKBUA2 1Phuket Marine Biological Center, 51 Sakdidach Rd. Phuket 83000, Thailand. E-mail: [email protected] 2 Veterinary Diagnostic Laboratory, Department of Veterinary Pathology, Faculty of Veterinary Medicine, Kasetsart University, Chatuchak, Bangkok 10903, Thailand. E-mail: [email protected] ABSTRACT Steatitis, which is caused by vitamin E deficiency, was observed in 3 captive Olive Ridley turtles (Lepidochelys olivacea) at Phuket Marine Biological Center, Phuket Province, Thailand during March to August 2005. Clinical findings had only shown depression and emaciation. Necropsy had revealed firm yellowish-brown masses distributed in fat tissues throughout the body. The predisposing cause of the disease is considered to be resulting from feeding these turtles mainly with frozen fish for more than 20 years, which can lead to vitamin E deficiency. Since there has been no effective treatment for chronic vitamin E deficiency, changes of the feeding from frozen fish to fresh fish and vitamin E supplementation of 100 IU/kg of fish fed have been recommended as a preventive treatment for the rest of the sea turtles in the center. KEYWORDS: olive ridley turtle, Lepidochelys olivacea, steatitis, vitamin E INTRODUCTION membranes, by preventing lipid peroxidation of Numerous scientific evidence indicates that reactive unsaturated fatty acids i.e. -
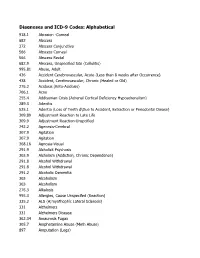
DSM III and ICD 9 Codes 11-2004
Diagnoses and ICD-9 Codes: Alphabetical 918.1 Abrasion -Corneal 682 Abscess 372 Abscess Conjunctiva 566 Abscess Corneal 566 Abscess Rectal 682.9 Abscess, Unspecified Site (Cellulitis) 995.81 Abuse, Adult 436 Accident Cerebrovascular, Acute (Less than 8 weeks after Occurrence) 438 Accident, Cerebrovascular, Chronic (Healed or Old) 276.2 Acidosis (Keto-Acidosis) 706.1 Acne 255.4 Addisonian Crisis (Adrenal Cortical Deficiency Hypoadrenalism) 289.3 Adenitis 525.1 Adentia (Loss of Teeth d\Due to Accident, Extraction or Periodontal Diease) 309.89 Adjustment Reaction to Late Life 309.9 Adjustment Reaction-Unspcified 742.2 Agenesis-Cerebral 307.9 Agitation 307.9 Agitation 368.16 Agnosia-Visual 291.9 Alcholick Psychosis 303.9 Alcholism (Addiction, Chronic Dependence) 291.8 Alcohol Withdrawal 291.8 Alcohol Withdrawal 291.2 Alcoholic Dementia 303 Alcoholism 303 Alcoholism 276.3 Alkalosis 995.3 Allergies, Cause Unspecifed (Reaction) 335.2 ALS (A;myothophic Lateral Sclerosis) 331 Alzheimers 331 Alzheimers Disease 362.34 Amaurosis Fugax 305.7 Amphetamine Abuse (Meth Abuse) 897 Amputation (Legs) 736.89 Amputation, Leg, Status Post (Above Knee, Below Knee) 736.9 Amputee, Site Unspecified (Acquired Deformity) 285.9 Anemia 284.9 Anemia Aplastic (Hypoplastic Bone Morrow) 280 Anemia Due to loss of Blood 281 Anemia Pernicious 280.9 Anemia, Iron Deficiency, Unspecified 285.9 Anemia, Unspecified (Normocytic, Not due to blood loss) 281.9 Anemia, Unspecified Deficiency (Macrocytic, Nutritional 441.5 Aneurysm Aortic, Ruptured 441.1 Aneurysm, Abdominal 441.3 Aneurysm, -

Eating Disorders: About More Than Food
Eating Disorders: About More Than Food Has your urge to eat less or more food spiraled out of control? Are you overly concerned about your outward appearance? If so, you may have an eating disorder. National Institute of Mental Health What are eating disorders? Eating disorders are serious medical illnesses marked by severe disturbances to a person’s eating behaviors. Obsessions with food, body weight, and shape may be signs of an eating disorder. These disorders can affect a person’s physical and mental health; in some cases, they can be life-threatening. But eating disorders can be treated. Learning more about them can help you spot the warning signs and seek treatment early. Remember: Eating disorders are not a lifestyle choice. They are biologically-influenced medical illnesses. Who is at risk for eating disorders? Eating disorders can affect people of all ages, racial/ethnic backgrounds, body weights, and genders. Although eating disorders often appear during the teen years or young adulthood, they may also develop during childhood or later in life (40 years and older). Remember: People with eating disorders may appear healthy, yet be extremely ill. The exact cause of eating disorders is not fully understood, but research suggests a combination of genetic, biological, behavioral, psychological, and social factors can raise a person’s risk. What are the common types of eating disorders? Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder. If you or someone you know experiences the symptoms listed below, it could be a sign of an eating disorder—call a health provider right away for help. -

Deep Brain Stimulation in Psychiatric Practice
Clinical Memorandum Deep brain stimulation in psychiatric practice March 2018 Authorising Committee/Department: Board Responsible Committee/Department: Section of Electroconvulsive Therapy and Neurostimulation Document Code: CLM PPP Deep brain stimulation in psychiatric practice The Royal Australian and New Zealand College of Psychiatrists (RANZCP) has developed this clinical memorandum to inform psychiatrists who are involved in using DBS as a treatment for psychiatric disorders. Clinical trials into the use of Deep Brain Stimulation (DBS) to treat psychiatric disorders such as depression, obsessive-compulsive disorder, substance use disorders, and anorexia are occurring worldwide, including within Australia. Although overall the existing literature shows promise for DBS in the treatment of psychiatric disorders, its use is still an emerging treatment and requires a stronger clinical evidence base of randomised control trials to develop a substantial body of evidence to identify and support its efficacy (Widge et al., 2016; Barrett, 2017). The RANZCP supports further research and clinical trials into the use of DBS for psychiatric disorders and acknowledges that it has potential application as a treatment for appropriately selected patients. Background DBS is an established treatment for movement disorders such as Parkinson’s disease, tremor and dystonia, and has also been used in the control of movement disorder associated with severe and medically intractable Tourette syndrome (Cannon et al., 2012). In Australia the Therapeutic Goods Administration has approved devices for DBS. It is eligible for reimbursement under the Medicare Benefits Schedule for the treatment of Parkinson’s disease but not for other neurological or psychiatric disorders. As the use of DBS in the treatment of psychiatric disorders is emerging, it is currently only available in speciality clinics or hospitals under research settings. -

Dsm-5 Diagnostic Criteria for Eating Disorders Anorexia Nervosa
DSM-5 DIAGNOSTIC CRITERIA FOR EATING DISORDERS ANOREXIA NERVOSA DIAGNOSTIC CRITERIA To be diagnosed with anorexia nervosa according to the DSM-5, the following criteria must be met: 1. Restriction of energy intaKe relative to requirements leading to a significantly low body weight in the context of age, sex, developmental trajectory, and physical health. 2. Intense fear of gaining weight or becoming fat, even though underweight. 3. Disturbance in the way in which one's body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or denial of the seriousness of the current low body weight. Even if all the DSM-5 criteria for anorexia are not met, a serious eating disorder can still be present. Atypical anorexia includes those individuals who meet the criteria for anorexia but who are not underweight despite significant weight loss. Research studies have not found a difference in the medical and psychological impacts of anorexia and atypical anorexia. BULIMIA NERVOSA DIAGNOSTIC CRITERIA According to the DSM-5, the official diagnostic criteria for bulimia nervosa are: • Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following: o Eating, in a discrete period of time (e.g. within any 2-hour period), an amount of food that is definitely larger than most people would eat during a similar period of time and under similar circumstances. o A sense of lacK of control over eating during the episode (e.g. a feeling that one cannot stop eating or control what or how much one is eating). -

Nutritional Diseases of Fish in Aquaculture and Their Management: a Review
Acta Scientific Pharmaceutical Sciences (ISSN: 2581-5423) Volume 2 Issue 12 December 2018 Review Article Nutritional Diseases of Fish in Aquaculture and Their Management: A Review Shoaibe Hossain Talukder Shefat1* and Mohammed Abdul Karim2 1Department of Fisheries Management, Faculty of Graduate Studies, Bangabandhu Sheikh Mujibur Rahman Agricultural University, Gazipur, Bangladesh 2Department of Fish Health Management, Faculty of Postgraduate Studies, Sylhet Agricultural University, Bangladesh *Corresponding Author: Shoaibe Hossain Talukder Shefat, Postgraduate Researcher, Department of Fisheries Management, Faculty of Graduate Studies, Bangabandhu Sheikh Mujibur Rahman Agricultural University, Gazipur, Bangladesh. Received: September 26, 2018; Published: November 19, 2018 Abstract aquaculture production and health safety. Information were collected from different secondary sources and then arranged chrono- This review was conducted to investigate the significance, underlying causes and negative effects of nutritional diseases of fish on logically. Investigation reveals that, Aquaculture is the largest single animal food producing agricultural sector that is growing rapidly all over the world. Nutritional disease is one of most devastating threats to aquaculture production because it is very difficult to quality and quantity. Public health hazards are also in dangerous situation due to frequent disease outbreak and treatment involving identify nutritional diseases. Production cost get increased due to investment lost, fish mortality, -

Patients' and Carers' Perspectives of Psychopharmacological
Chapter Patients’ and Carers’ Perspectives of Psychopharmacological Interventions Targeting Anorexia Nervosa Symptoms Amabel Dessain, Jessica Bentley, Janet Treasure, Ulrike Schmidt and Hubertus Himmerich Abstract In clinical practice, patients with anorexia nervosa (AN), their carers and clini- cians often disagree about psychopharmacological treatment. We developed two corresponding questionnaires to survey the perspectives of patients with AN and their carers on psychopharmacological treatment. These questionnaires were dis- tributed to 36 patients and 37 carers as a quality improvement project on a specialist unit for eating disorders at the South London and Maudsley NHS Foundation Trust. Although most patients did not believe that medication could help with AN, the majority thought that medication for AN should help with anxiety (61.1%), con- centration (52.8%), sleep problems (52.8%) and anorexic thoughts (55.6%). Most of the carers shared the view that drug treatment for AN should help with anxiety (54%) and anorexic thoughts (64.8%). Most patients had concerns about potential weight gain, increased appetite, changes in body shape and metabolism during psychopharmacological treatment. By contrast, the majority of carers were not concerned about these specific side effects. Some of the concerns expressed by the patients seem to be AN-related. However, their desire for help with anxiety and anorexic thoughts, which is shared by their carers, should be taken seriously by clinicians when choosing a medication or planning psychopharmacological studies. Keywords: anorexia nervosa, psychopharmacological treatment, treatment effects, side effects, opinion survey, patients, carers 1. Introduction 1.1 Anorexia nervosa Anorexia nervosa (AN) is an eating disorder. According to the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [1], its diagnostic criteria are significantly low body weight, intense fear of weight gain, and disturbed body perception. -

Brain Growth in Children with Marasmus
Upsala J Med Sci 79: 116-128, 1974 Brain Growth in Children with Marasmus A Study Using Head Circumference Measurement, Transillumination and Ultrasonic Echo Ventriculography GUNNAR ENGSNER,2 SHOADAGNE BELETE,' IRENE SJOGREN2 and BO VAHLQUIST' From the Ethiopian Nutrition Institute, Addis Ababa, Ethiopia, I and the Department of Pediatrics, University Hospitals2Uppsala, Sweden ABSTRACT (I) To measure the brain size in marasmic in- Brain growth was studied by making simultaneous meas- fants and children by simultaneously recording the urements of head circumference, transillumination and head circumference and performing transillumina- lateral ventricle indices in 102 children aged 2-24 months tion and echo encephalography. suffering from marasmus. The head circumference was (2) To demonstrate whether or not, in infants significantly reduced, transillumination showed a slight- with marasmus aged less than six months, a re- to-moderate increase in the children 6-24 months of age, and echo encephalography showed a normal lateral ven- cordable improvement in brain size takes place tricle index. The results indicate a reduction of brain during nutrition rehabilitation. size which (particularly after the first 6 months of age) goes slightly beyond what may be inferred from the head circumference per se. The interpretation of the results, MATERIAL especially the relation between head circumference and brain size, is discused. Definition of marasmus The criteria used for including children in the study were as follows: In cases of severe protein-calorie malnutrition (a) Weight for age below 60% of the Boston standard (PCM) of the marasmus type, there is not only a (50% percentile) and no apparent oedema, i.e. -

Importance of Considering Malnutrition and Sarcopenia in Order to Improve the QOL of Elderly Hemodialysis Patients in Japan in the Era of 100-Year Life
nutrients Review Importance of Considering Malnutrition and Sarcopenia in Order to Improve the QOL of Elderly Hemodialysis Patients in Japan in the Era of 100-Year Life Masaaki Inaba 1,2,*, Senji Okuno 3 and Yoshiteru Ohno 2 1 Department of Nephrology, Osaka City University Medical School, 1-4-3 Asahi-machi, Abeno-ku, Osaka 543-8585, Japan 2 Kidney Center, Ohno Memorial Hospital, 1-26-10, Minami-Horie, Nishi-ku, Osaka 550-0015, Japan; [email protected] 3 Kidney Center, Shirasagi Hospital, 7-11-23, Higashisumiyoshi-ku, Osaka 546-0002, Japan; [email protected] * Correspondence: [email protected] Abstract: In the current aging society of Japan, malnutrition and resultant sarcopenia have been widely identified as important symptomatic indicators of ill health and can cause impairments of longevity and quality of life in older individuals. Elderly individuals are recommended to have sufficient calorie and protein intake so as to enjoy a satisfactory quality of life, including maintaining activities of daily living in order to avoid emaciation and sarcopenia. The prevalence of emaciation and sarcopenia in elderly hemodialysis (HD) patients in Japan is higher than in non-HD elderly subjects due to the presence of malnutrition and sarcopenia associated with chronic kidney disease (CKD). Furthermore, comorbidities, such as diabetes and osteoporosis, induce malnutrition Citation: Inaba, M.; Okuno, S.; Ohno, Y. Importance of Considering and sarcopenia in HD patients. This review presents findings regarding the mechanisms of the Malnutrition and Sarcopenia in Order development of these early symptomatic conditions and their significance for impaired QOL and to Improve the QOL of Elderly increased mortality in elderly HD patients. -

The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic Criteria for Research
The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic criteria for research World Health Organization Geneva The World Health Organization is a specialized agency of the United Nations with primary responsibility for international health matters and public health. Through this organization, which was created in 1948, the health professions of some 180 countries exchange their knowledge and experience with the aim of making possible the attainment by all citizens of the world by the year 2000 of a level of health that will permit them to lead a socially and economically productive life. By means of direct technical cooperation with its Member States, and by stimulating such cooperation among them, WHO promotes the development of comprehensive health services, the prevention and control of diseases, the improvement of environmental conditions, the development of human resources for health, the coordination and development of biomedical and health services research, and the planning and implementation of health programmes. These broad fields of endeavour encompass a wide variety of activities, such as developing systems of primary health care that reach the whole population of Member countries; promoting the health of mothers and children; combating malnutrition; controlling malaria and other communicable diseases including tuberculosis and leprosy; coordinating the global strategy for the prevention and control of AIDS; having achieved the eradication of smallpox, promoting mass immunization against a number of other -

Diencephalic Syndrome: a Cause of Failure to Thrive and a Model of Partial Growth Hormone Resistance
Diencephalic Syndrome: A Cause of Failure to Thrive and a Model of Partial Growth Hormone Resistance Amy Fleischman, MD*; Catherine Brue, MD*; Tina Young Poussaint, MD‡; Mark Kieran, MD, PhD§; Scott L. Pomeroy, MD, PhD¶; Liliana Goumnerova, MD#; R. Michael Scott, MD#; and Laurie E. Cohen, MD* ABSTRACT. Diencephalic syndrome is a rare but po- total of 48 similar cases, including the 12 described tentially lethal cause of failure to thrive in infants and by Russell. Since then, several case studies have been young children. The diencephalic syndrome includes reported with similar symptoms, a few with brain clinical characteristics of severe emaciation, normal lin- tumors located in the posterior fossa.2,3 Nystagmus ear growth, and normal or precocious intellectual devel- and vomiting were also noted in the majority of opment in association with central nervous system tu- reported cases.2–5 In 1976, a review of 72 cases by mors. Our group initially described a series of 9 patients 6 with diencephalic syndrome and found a reduced prev- Burr confirmed the clinical characteristics of dience- alence of emesis, hyperalertness, or hyperactivity com- phalic syndrome. Subsequent literature has consisted pared with previous reports. Also, the tumors were found of multiple case series and case reports of this to be larger, occur at a younger age, and behave more syndrome. aggressively than similarly located tumors without dien- We reviewed the 11 cases of diencephalic syn- cephalic syndrome. We have been able to extend our drome that presented to Children’s Hospital Boston follow-up of the original patients, as well as describe 2 and Dana-Farber Cancer Institute between 1970 and additional cases.