Genetics Evaluation for the Etiologic Diagnosis of Autism Spectrum Disorders G
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Autism Guideline Jan2018.Pdf
DATE: January 2018 TEXAS CHILDREN’S HOSPITAL EVIDENCE-BASED OUTCOMES CENTER Screening and Diagnosis of Autism Spectrum Disorder (ASD) Evidence-Based Guideline Definition: (1) Autism Spectrum Disorder (ASD) per the DSM-5 Early Signs (2,5,6) encompasses four previously separate disorders that are Social Skills Deficits actually a single condition with different levels of symptom Early years severity in two core domains. These four disorders are the - Do not appear to seek connectedness DSM-IV Autistic Disorder (autism), Asperger’s Disorder, - Contentbeingalone Childhood Disintegrative Disorder, and Pervasive - Ignore parents’ bids for attention Developmental Disorder Not Otherwise Specified (PDD-NOS). - Seldom make eye contact or bid for others’ attention ASD is characterized in early childhood by 1) deficits in social with gestures or vocalizations communication and social interaction and 2) restricted - Deficits in joint attention repetitive behaviors, interests, and activities (RRBs). - Fail to follow a point and/or share expression - Failto point to “comment” Etiology: (2) Although ASDs are heritable neurodevelopmental - Failtorespondtoname conditions with strong genetic underpinnings, their exact - Selective hearing etiology is unknown. The etiology is multifactorial with a variety - Less imitation of genetic and, to a lesser extent, environmental factors Later years playing a role. ASDs can be either idiopathic or associated with - Difficulty sharing the emotional state of others in other diagnoses; most are idiopathic. cooperative -

Developmental Delay and the Methyl Binding Genes H Turner, F Macdonald, S Warburton, F Latif, T Webb
1of3 ELECTRONIC LETTER J Med Genet: first published as 10.1136/jmg.40.2.e13 on 1 February 2003. Downloaded from Developmental delay and the methyl binding genes H Turner, F MacDonald, S Warburton, F Latif, T Webb ............................................................................................................................. J Med Genet 2003;40:e13(http://www.jmedgenet.com/cgi/content/full/40/2/e13) he report by Amir et al1 that Rett syndrome (RS) is associ- children referred with a clinical diagnosis of Angelman ated with mutations in the MECP2 gene permitted labora- syndrome (AS) but without an abnormality in 15q11q13 tory diagnosis of this devastating yet common neurode- showed that 4/46 of the girls in one case8 and 5/40 in the T 9 velopmental disorder. Hitherto the paucity of familial cases of other actually had Rett syndrome. Of these nine probands, the syndrome and the failure to identify the syndrome in only one was later found to have a clinical presentation incon- males despite fairly wide clinical criteria had defined it as an sistent with the laboratory diagnosis. This may not be surpris- X linked dominant disorder with male lethality.2 Soon, ing given that in very small girls the two syndromes may however, reports from the few families in which RS is present with overlapping clinical features and so be difficult to segregating showed that male family members who inherited differentiate on clinical grounds alone. the same mutation in the MECP2 gene as their affected female Familial cases of developmental handicap -
Overview of Biomedical Treatments Presentation
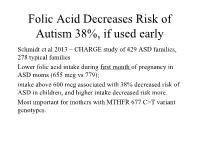
Folic Acid Decreases Risk of Autism 38%, if used early Schmidt et al 2013 – CHARGE study of 429 ASD families, 278 typical families Lower folic acid intake during first month of pregnancy in ASD moms (655 mcg vs 779); intake above 600 mcg associated with 38% decreased risk of ASD in children, and higher intake decreased risk more. Most important for mothers with MTHFR 677 C>T variant genotypes. Folic Acid decreases risk of ASD if taken near conception (cont.) Suren et al 2013 – study of 85,176 Norwegian children, including 270 with ASD. In children whose mothers took folic acid (400 mcg) between 4 weeks prior to conception to 8 weeks after conception, 0.10% (64/61 042) had autistic disorder, compared with 0.21% (50/24 134) in those unexposed to folic acid. 39% lower risk of ASD in those who took prenatal folic acid (400 mcg); Little benefit if taken after 8 weeks Overview of Dietary, Nutritional, and Medical Treatments for Autism James B. Adams, Ph.D. President’s Professor, Arizona State University President, Autism Society of Greater Phoenix President, Autism Nutrition Research Center Chair of Scientific Advisory Board, Neurological Health Foundation Father of a daughter with autism http://autism.asu.edu Our research group is dedicated to finding the causes of autism, how to prevent autism, and how to best help people with autism. Nutrition: vitamins, minerals, fatty acids, amino acids Metabolism: glutathione, methylation, sulfation, oxidative stress Mitochondria – ATP, muscle strength, carnitine Toxic Metals and Chelation Gastrointestinal -

Retted Q&A: Epilepsy Incidence, Treatments and Research Dr. Eric
RettEd Q&A: Epilepsy Incidence, Treatments and Research Dr. Eric Marsh, MD PhD, Medical Director Rett Clinic, NHS Investigator, and Basic Scientist, Children’s Hospital of Philadelphia Webcast 09/11/2018 Facilitator: Paige Nues, Rettsyndrome.org Recording link: https://attendee.gotowebinar.com/recording/2303318923907771398 ATTENDEE QUESTIONS RESPONSE REFERENCES AED Questions: Treatments and Triggers I want to know what about relation between Stressors are anecdotally reported to lower the seizure pain, digestive pain, apnea and seizure threshold- these would all be stressful features that could discharge. lower seizure threshold and theoretically increase seizure frequency. Any opinions on fycompa? Very limited experience so far to make a clear judgment. I have tried it in 2 Rett patients without great success, both in patients with very severe seizures. Is there a way to tell the difference between There is a slide in the talk that goes over some features, such a seizure and a “Rett spell” other than EEG? as retained awareness, repetitive nature of the events, that can give some hints as to the nature of the event, but only EEG can definitively discern the difference. My daughter has epilepsy and always has Without knowing all of her clinical details, it is hard for me to seizures. She takes medication Onfi and give recommendations. Depending on seizure types, EEG, Keppra and still have seizures. What should and previous medications tried, I would suggest other meds I do? I need help and ideas thanks. such as Rufinamide, valproic acid or trying the ketogenic diet. Do you see seizures connected to puberty or You can look at Jane Lane’s RettEd about puberty. -

Communication Intervention in Rett Syndrome: a Systematic Review Research in Autism Spectrum Disorders
Research in Autism Spectrum Disorders 3 (2009) 304–318 Contents lists available at ScienceDirect Research in Autism Spectrum Disorders Journal homepage: http://ees.elsevier.com/RASD/default.asp Review Communication intervention in Rett syndrome: A systematic review Jeff Sigafoos a,*, Vanessa A. Green a, Ralf Schlosser b, Mark F. O’eilly c, Giulio E. Lancioni d, Mandy Rispoli c, Russell Lang c a Victoria University of Wellington, New Zealand b Northeastern University, Boston and Childrens Hospital Boston at Waltham, MA, USA c Meadows Center for Preventing Educational Risk, The University of Texas at Austin, Austin, TX, USA d University of Bari, Bari, Italy ARTICLE INFO ABSTRACT Article history: We reviewed communication intervention studies involving people Received 25 September 2008 with Rett syndrome. Systematic searches of five electronic databases, Accepted 26 September 2008 selected journals, and reference lists identified nine studies meeting the inclusion criteria. These studies were evaluated in terms of: (a) Keywords: participant characteristics, (b) target skills, (c) procedures, (d) main Communication intervention findings, and (e) certainty of evidence. Across the nine studies, Rett syndrome intervention was provided to a total of 31 participants aged 2:7–17:0 Systematic review (years:months). Communication modes included speech, gestures, communication boards, and computer-based systems. Targeted communication functions included imitative speech, requesting, naming/commenting, and various receptive language skills (e.g., respond to requests, answer questions, receptively identify symbols). Intervention approaches included early intensive behavioral inter- vention, systematic instruction, and music therapy. Positive out- comes were reported for 26 (84%) of the 31 participants. However, these outcomes must be interpreted with caution because the certainty of evidence was inconclusive for all but one of the studies. -

Measuring the Effectiveness of Play As an Intervention to Support
Measuring the Effectiveness of Play as an Intervention to Support Language Development in Young Children with Autism Spectrum Disorder: A Hierarchically- Modeled Meta-Analysis by Gregory V. Boerio Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Education in the Educational Leadership Program Youngstown State University May, 2021 Measuring the Effectiveness of Play as an Intervention to Support Language Development in Young Children with Autism Spectrum Disorder: A Hierarchically- Modeled Meta-Analysis Gregory V. Boerio I hereby release this dissertation to the public. I understand that this dissertation will be made available from the OhioLINK ETD Center and the Maag Library Circulation Desk for public access. I also authorize the University or other individuals to make copies of this thesis as needed for scholarly research. Signature: _______________________________________________________________ Gregory V. Boerio, Student Date Approvals: _______________________________________________________________ Dr. Karen H. Larwin, Dissertation Chair Date _______________________________________________________________ Dr. Patrick T. Spearman, Committee Member Date _______________________________________________________________ Dr. Carrie R. Jackson, Committee Member Date _______________________________________________________________ Dr. Matthew J. Erickson, Committee Member Date _______________________________________________________________ Dr. Salvatore A. Sanders, Dean of Graduate Studies Date ii © G. Boerio 2021 iii Abstract The purpose of the current investigation is to analyze extant research examining the impact of play therapy on the development of language skills in young children with autism spectrum disorder (ASD). As rates of ASD diagnoses continue to increase, families and educators are faced with making critical decisions regarding the selection and implementation of evidence-based practices or therapies, including play-based interventions, to support the developing child as early as 18 months of age. -

New Microdeletion and Microduplication Syndromes: a Comprehensive Review
Genetics and Molecular Biology, 37, 1 (suppl), 210-219 (2014) Copyright © 2014, Sociedade Brasileira de Genética. Printed in Brazil www.sbg.org.br Review Article New microdeletion and microduplication syndromes: A comprehensive review Julián Nevado1,2*, Rafaella Mergener3*, María Palomares-Bralo1,2, Karen Regina Souza3, Elena Vallespín1,2, Rocío Mena1,2, Víctor Martínez-Glez1,2, María Ángeles Mori1,2, Fernando Santos1,4, Sixto García-Miñaur1,4, Fé García-Santiago1,5, Elena Mansilla1,5, Luis Fernández1,6, María Luisa de Torres1,5, Mariluce Riegel3,7$ and Pablo Lapunzina1,4,8$ 1Centro de Investigación Biomédica en Red de Enfermedades Raras, Instituto de Salud Carlos III, Madrid, Spain. 2Section of Functional and Structural Genomics, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. 3Programa de Pós-graduação em Genética e Biologia Molecular, Universidade Federal do Rio Grande do Sul, Porto Alegre,RS, Brazil. 4Section of Clinical Genetics, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. 5Section of Cytogenetics, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. 6Section of Preanalytics, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. 7Serviço de Genética Médica, Hospital de Clínicas de Porto Alegre, Porto Alegre ,RS, Brazil. 8Section of Molecular Endocrinology, Overgrowth Disordes Laboratory, Instituto de Genética Médica y Molecular, Hospital Universitario la Paz, Madrid, Spain. Abstract Several new microdeletion and microduplication syndromes are emerging as disorders that have been proven to cause multisystem pathologies frequently associated with intellectual disability (ID), multiple congenital anomalies (MCA), autistic spectrum disorders (ASD) and other phenotypic findings. In this paper, we review the “new” and emergent microdeletion and microduplication syndromes that have been described and recognized in recent years with the aim of summarizing their main characteristics and chromosomal regions involved. -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -

LEO KANNER (1894-1981) PAPERS to Many As "Kanner's Syndrome")
Kanner Papers (1 of 3) student, Kanner taught himself pediatric psychiatry--and went on to teach generations of students what he learned. He published the first American textbook to bear the title "Child Psychiatry." In separate prefaces to the first edition, Adolf Meyer wrote, "it will serve as a safe starting point and an incentive to proceed from what is well tried to the ever new ground to be conquered" and Edwards Parks added, "the book is full of wisdom and common sense, no other book is quite like it. It brings to the pediatrician much needed aid." Dr. Kanner is best known for his delineation in 1943 of the syndrome he described as "autistic disturbances of affective contact" but later designated as early infantile autism (and known LEO KANNER (1894-1981) PAPERS to many as "Kanner's syndrome"). Less well known but deserving of as much remembrance is Leo Kanner's concern for mentally ARCHIVES FINDING AID [Processed by W. E. Baxter, 12 November, 1985.] retarded children at a time when most psychiatrists excluded them from the purview of their clinics. Presentation of a paper on this subject resulted in a double row of inch-high headlines across the BIOGRAPHY Baltimore Sun on April 8, 1938, and led to community action to end a foul practice generated by the collusion of attorneys and Leo Kanner was born on June 13, 1894, in Klekotow, Austria. judges over the valiant opposition of the superintendent of the The young Kanner proved to be an extraordinary student and began Training School. The practice had been to obtain the release of to write poetry when he was only ten. -
Fragile X Syndrome
AUCD Annual Conference Research Symposium The Rapidly Changing Landscape of Fragile X Elizabeth Berry-Kravis MD PhD Rush University Medical Center Disclosures: EBK has received funding from Neuropharm LTD, Seaside Therapeutics , Novartis and Roche Pharmaceuticals to consult on trial design and conduct clinical trials in FXS Features of Fragile X Syndrome • Physical: large prominent ears, long face, large head, prominent jaw and forehead, midfacial hypoplasia hyperflexible joints, large testis • Intellectual Disability or LD • Behavior problems: hyperactivity distractibility, anxiety, perseveration • Autism: 18-36% AD, 43-67% ASD • Seizures – 15% • Strabismus – 30% • Medical: otitis, sinus, MVP, reflux, sleep apnea, loose stools, allergies FXS Treatment in Clinic - Rush FXS Clinic since 1992 > 450 patients Supportive • Aggressive tx of otitis – • Early intervention tubes/audiology • Intensive speech therapy • Manage sleep apnea – • OT with sensory integration T&A • Inclusion in school as much • Treat sleep dysregulation as possible – melatonin/medications • Educational curriculum, • Yearly eye exams – environment, teaching style patching, surgery, glasses matched to FXS cognitive • Control seizures profile • Orthopedics if needed • Socialization program • Monitor for MVP/heart • Behavior plan • Genetic counseling • Behavior medications for • Discuss reproductive ADD/anxiety options Seizures in Fragile X Syndrome – Recent and Largest Study National Fragile X Survey 1394 FXS full mutation (1090 M, 304 F) 173 (12%) seizures: 154 (14%) -

The Fragile X Syndrome and Infantile Autism: a Prevalence Study Brian Herb Annex Yale University
Yale University EliScholar – A Digital Platform for Scholarly Publishing at Yale Yale Medicine Thesis Digital Library School of Medicine 1985 The fragile X syndrome and infantile autism: a prevalence study Brian Herb Annex Yale University Follow this and additional works at: http://elischolar.library.yale.edu/ymtdl Recommended Citation Annex, Brian Herb, "The fragile X syndrome and infantile autism: a prevalence study" (1985). Yale Medicine Thesis Digital Library. 2345. http://elischolar.library.yale.edu/ymtdl/2345 This Open Access Thesis is brought to you for free and open access by the School of Medicine at EliScholar – A Digital Platform for Scholarly Publishing at Yale. It has been accepted for inclusion in Yale Medicine Thesis Digital Library by an authorized administrator of EliScholar – A Digital Platform for Scholarly Publishing at Yale. For more information, please contact [email protected]. YALE MEDICAL LIBRARY Permission for photocopying or microfilming of " TU (title of thesis) tr for the purpose of individual scholarly consultation or refer¬ ence is hereby granted by the author. This permission is not to be interpreted as affecting publication of this work, or otherwise placing it in the public domain, and the author re¬ serves all rights of ownership guaranteed under common law protection of unpublished manuscripts. (Signature of author) (Printed name) (Date) Digitized by the Internet Archive in 2017 with funding from The National Endowment for the Humanities and the Arcadia Fund https://archive.org/details/fragilexsyndromeOOanne The Fragile X Syndrome and Infantile Autism A Prevalence Study A Thesis Submitted to the Yale University School of Medicine in Partial Fulfillment of the Requirements for the degree of Doctor of Medicine by Brian Herb Annex 1985 Acknowledgments I would like to express my sincere appreciation to all those who advised and assisted me in this thesis project. -

Level Estimates of Maternal Smoking and Nicotine Replacement Therapy During Pregnancy
Using primary care data to assess population- level estimates of maternal smoking and nicotine replacement therapy during pregnancy Nafeesa Nooruddin Dhalwani BSc MSc Thesis submitted to the University of Nottingham for the degree of Doctor of Philosophy November 2014 ABSTRACT Background: Smoking in pregnancy is the most significant preventable cause of poor health outcomes for women and their babies and, therefore, is a major public health concern. In the UK there is a wide range of interventions and support for pregnant women who want to quit. One of these is nicotine replacement therapy (NRT) which has been widely available for retail purchase and prescribing to pregnant women since 2005. However, measures of NRT prescribing in pregnant women are scarce. These measures are vital to assess its usefulness in smoking cessation during pregnancy at a population level. Furthermore, evidence of NRT safety in pregnancy for the mother and child’s health so far is nebulous, with existing studies being small or using retrospectively reported exposures. Aims and Objectives: The main aim of this work was to assess population- level estimates of maternal smoking and NRT prescribing in pregnancy and the safety of NRT for both the mother and the child in the UK. Currently, the only population-level data on UK maternal smoking are from repeated cross-sectional surveys or routinely collected maternity data during pregnancy or at delivery. These obtain information at one point in time, and there are no population-level data on NRT use available. As a novel approach, therefore, this thesis used the routinely collected primary care data that are currently available for approximately 6% of the UK population and provide longitudinal/prospectively recorded information throughout pregnancy.