Autism Guideline Jan2018.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Fragile X Syndrome
AUCD Annual Conference Research Symposium The Rapidly Changing Landscape of Fragile X Elizabeth Berry-Kravis MD PhD Rush University Medical Center Disclosures: EBK has received funding from Neuropharm LTD, Seaside Therapeutics , Novartis and Roche Pharmaceuticals to consult on trial design and conduct clinical trials in FXS Features of Fragile X Syndrome • Physical: large prominent ears, long face, large head, prominent jaw and forehead, midfacial hypoplasia hyperflexible joints, large testis • Intellectual Disability or LD • Behavior problems: hyperactivity distractibility, anxiety, perseveration • Autism: 18-36% AD, 43-67% ASD • Seizures – 15% • Strabismus – 30% • Medical: otitis, sinus, MVP, reflux, sleep apnea, loose stools, allergies FXS Treatment in Clinic - Rush FXS Clinic since 1992 > 450 patients Supportive • Aggressive tx of otitis – • Early intervention tubes/audiology • Intensive speech therapy • Manage sleep apnea – • OT with sensory integration T&A • Inclusion in school as much • Treat sleep dysregulation as possible – melatonin/medications • Educational curriculum, • Yearly eye exams – environment, teaching style patching, surgery, glasses matched to FXS cognitive • Control seizures profile • Orthopedics if needed • Socialization program • Monitor for MVP/heart • Behavior plan • Genetic counseling • Behavior medications for • Discuss reproductive ADD/anxiety options Seizures in Fragile X Syndrome – Recent and Largest Study National Fragile X Survey 1394 FXS full mutation (1090 M, 304 F) 173 (12%) seizures: 154 (14%) -

The Fragile X Syndrome and Infantile Autism: a Prevalence Study Brian Herb Annex Yale University
Yale University EliScholar – A Digital Platform for Scholarly Publishing at Yale Yale Medicine Thesis Digital Library School of Medicine 1985 The fragile X syndrome and infantile autism: a prevalence study Brian Herb Annex Yale University Follow this and additional works at: http://elischolar.library.yale.edu/ymtdl Recommended Citation Annex, Brian Herb, "The fragile X syndrome and infantile autism: a prevalence study" (1985). Yale Medicine Thesis Digital Library. 2345. http://elischolar.library.yale.edu/ymtdl/2345 This Open Access Thesis is brought to you for free and open access by the School of Medicine at EliScholar – A Digital Platform for Scholarly Publishing at Yale. It has been accepted for inclusion in Yale Medicine Thesis Digital Library by an authorized administrator of EliScholar – A Digital Platform for Scholarly Publishing at Yale. For more information, please contact [email protected]. YALE MEDICAL LIBRARY Permission for photocopying or microfilming of " TU (title of thesis) tr for the purpose of individual scholarly consultation or refer¬ ence is hereby granted by the author. This permission is not to be interpreted as affecting publication of this work, or otherwise placing it in the public domain, and the author re¬ serves all rights of ownership guaranteed under common law protection of unpublished manuscripts. (Signature of author) (Printed name) (Date) Digitized by the Internet Archive in 2017 with funding from The National Endowment for the Humanities and the Arcadia Fund https://archive.org/details/fragilexsyndromeOOanne The Fragile X Syndrome and Infantile Autism A Prevalence Study A Thesis Submitted to the Yale University School of Medicine in Partial Fulfillment of the Requirements for the degree of Doctor of Medicine by Brian Herb Annex 1985 Acknowledgments I would like to express my sincere appreciation to all those who advised and assisted me in this thesis project. -

The Fragile X Syndrome–Autism Comorbidity: What Do We Really Know?
REVIEW ARTICLE published: 16 October 2014 doi: 10.3389/fgene.2014.00355 The fragile X syndrome–autism comorbidity: what do we really know? Leonard Abbeduto 1,2*, Andrea McDuffie 1,2 and Angela John Thurman 1,2 1 MIND Institute, University of California, Davis, Sacramento, CA, USA 2 Department of Psychiatry and Behavioral Sciences, University of California, Davis, Sacramento, CA, USA Edited by: Autism spectrum disorder (ASD) is a common comorbid condition in people with fragile Anne C. Wheeler, Carolina Institute X syndrome (FXS). It has been assumed that ASD symptoms reflect the same underlying for Developmental Disabilities; University of North Carolina at psychological and neurobiological impairments in both FXS and non-syndromic ASD, which Chapel Hill, USA has led to the claim that targeted pharmaceutical treatments that are efficacious for core Reviewed by: symptoms of FXS are likely to be beneficial for non-syndromic ASD as well. In contrast, we Molly Losh, Northwestern present evidence from a variety of sources suggesting that there are important differences University, USA in ASD symptoms, behavioral and psychiatric correlates, and developmental trajectories Dejan Budimirovic, Kennedy Krieger Institute/The Johns Hopkins between individuals with comorbid FXS and ASD and those with non-syndromic ASD. We University, USA also present evidence suggesting that social impairments may not distinguish individuals *Correspondence: with FXS with and without ASD. Finally, we present data that demonstrate that the Leonard Abbeduto, MIND Institute, neurobiological substrates of the behavioral impairments, including those reflecting core University of California, Davis, 2825 ASD symptoms, are different in FXS and non-syndromic ASD. Together, these data suggest 50th Street, Sacramento, CA 95817, USA that there are clinically important differences between FXS and non-syndromic ASD e-mail: leonard.abbeduto@ucdmc. -

Clinical Report—Health Supervision for Children with Fragile X Syndrome
Guidance for the Clinician in Rendering Pediatric Care Clinical Report—Health Supervision for Children With Fragile X Syndrome Joseph H. Hersh, MD, Robert A. Saul, MD, and COMMITTEE abstract ON GENETICS Fragile X syndrome (an FMR1–related disorder) is the most commonly KEY WORDS fragile X syndrome, FMR1–related conditions, mental inherited form of mental retardation. Early physical recognition is dif- retardation, health guidelines ficult, so boys with developmental delay should be strongly considered ABBREVIATIONS for molecular testing. The characteristic adult phenotype usually does FMR1—fragile X mental retardation 1 gene not develop until the second decade of life. Girls can also be affected CGG—cytosine-guanine-guanine FMRP—fragile X mental retardation 1 protein with developmental delay. Because multiple family members can be mGluR—metabotropic glutamate receptor affected with mental retardation and other conditions (premature POI—primary ovarian insufficiency ovarian failure and tremor/ataxia), family history information is of FXTAS—fragile X–associated tremor/ataxia syndrome critical importance for the diagnosis and management of affected pa- This document is copyrighted and is property of the American tients and their families. This report summarizes issues for fragile X Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American syndrome regarding clinical diagnosis, laboratory diagnosis, genetic Academy of Pediatrics. Any conflicts have been resolved through counseling, related health problems, behavior management, and age- a process approved by the Board of Directors. The American related health supervision guidelines. The diagnosis of fragile X syn- Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of drome not only involves the affected children but also potentially has this publication. -

Fragile X Syndrome
Fragile X syndrome What is fragile X syndrome? Fragile X syndrome is an X-linked disease of intellectual disability with variable severity.1 Expansions of CGG repeat sequences in the FMR1 gene account for 99% of mutations causing fragile X syndrome. Interpretation of CGG repeat expansion results is based on the following ranges: Negative: <45 repeats; intermediate: 45-54 repeats; premutation: 55-200 repeats; full mutation: >200 repeats. Greater than 99% of males and approximately 50% of females with the full mutation are intellectually disabled.2 What are the symptoms of fragile X syndrome and what treatment is available? Fragile X syndrome is associated with a range of symptoms. Early signs include delayed speech and language skills.1 Intellectual problems vary from mild learning disabilities to severe intellectual disability.3 Behavioral characteristics include autism and hyperactivity.1 Physical features, such as a long face and large or prominent ears, are usually more noticeable in adults than in children, and in males more than females.3 There is no cure for fragile X syndrome. Treatment is supportive and focuses on educational and behavioral support and management of symptoms.2 Individuals with a premutation do not have fragile X syndrome, but may have an increased risk for fragile X-related disorders. Females may have fragile X-associated primary ovarian insufficiency (FXPOI), which can cause infertility or early menopause. Most males with a premutation and some females are at risk for fragile X-associated tremor and ataxia syndrome -

A Functional MRI Study of Facial Emotion-Processing
G C A T T A C G G C A T genes Article Autism in Fragile X Syndrome; A Functional MRI Study of Facial Emotion-Processing Andrew G. McKechanie 1,2,* , Sonya Campbell 1, Sarah E. A. Eley 1 and Andrew C. Stanfield 1,2 1 The Patrick Wild Centre, The University of Edinburgh, Edinburgh EH10 5HF, UK; [email protected] (S.C.); [email protected] (S.E.A.E.); andrew.stanfi[email protected] (A.C.S.) 2 NHS Lothian, Edinburgh EH1 3EG, UK * Correspondence: [email protected]; Tel.: +44-131-537-6000 Received: 1 November 2019; Accepted: 13 December 2019; Published: 17 December 2019 Abstract: Fragile X syndrome (FXS) is the most common inherited cause of intellectual disability and autism spectrum disorder, and among those with fragile X syndrome, approximately 1/3rd meet a threshold for an autism spectrum disorder (ASD) diagnosis. Previous functional imaging studies of fragile X syndrome have typically focused on those with fragile X syndrome compared to either neurotypical or autism spectrum disorder control groups. Further, the majority of previous studies have tended to focus on those who are more intellectually able than is typical for fragile X syndrome. In this study, we examine the impact of autistic traits in individuals with fragile X syndrome on a paradigm looking at facial emotion processing. The study included 17 individuals with fragile X syndrome, of whom 10 met criteria for autism as measured by the Autism Diagnostic Observation Schedule (ADOS). Prior to the scan, participants rehearsed on a mock scanner to help acclimatize to the scanner environment and thus allow more severely affected individuals to participate. -

Understanding Autism
Introduction As a parent, you may have many questions regarding diagnosis. As you look for answers, you may encounter information about autism, its causes, and possible treatments. All of these different opinions can make it challenging for a family to organize options and begin to choose a treatment plan that best fits the family. We hope that this packet will help better prepare you to understand the information you receive about treatments for autism, as well as give you the chance to look over the most recent professional opinions about autism. Westside Regional Center anticipates supporting your family as you proceed from your lifetime. What is Autism? How and why did my child develop autism Unfortunately, no apparent cause exists for most cases, but most experts believe that autism is primarily a genetic condition. For about 10% of cases, experts believe that autism has either a specific genetic (from parent to child) or environmental cause. For example, there is an increased risk for autism from specific genetic disorders such as Fragile X Syndrome, Angelman Syndrome, Tuberous Sclerosis, Rh untreated Phenylketonuria, and some chromosome abnormalities. Known environmental causes include taking thalidomide during pregnancy (a type of sedative now not routinely available in the United States) or having German measles (rubella) during pregnancy. There are three main behaviors that are found in all children with autism: 1. Difficulty with social interaction: Children with autism may not be able to relate easily to people, have a hard time playing with other children, or have certain behaviors, such as avoiding eye contact or making socially inappropriate gestures in conversation. -

UNIVERSITY of CALIFORNIA Los Angeles Social
UNIVERSITY OF CALIFORNIA Los Angeles Social Justice and Autism: Links to Personality and Advocacy A dissertation submitted in partial satisfaction of the requirements for the degree of Doctor of Philosophy in Education by Steven Kenneth Kapp 2016 © Copyright by Steven Kenneth Kapp 2016 ABSTRACT OF THE DISSERTATION Social Justice and Autism: Links to Personality and Advocacy by Steven Kenneth Kapp Doctor of Philosophy in Education University of California, Los Angeles, 2016 Professor Connie L. Kasari, Chair Autism’s history as an independent condition may originate from “autistic psychopathy”, but autism and psychopathy may entail opposite patterns of personality. Autism may incline people toward moral intuitions in the dimensions of care, loyalty, authority, sanctity, and especially fairness. Yet these may play an unconscious and visceral role that in combination with difficulties with moral reasoning and the understanding of one’s own and others’ emotional and mental states, reduces self- and other awareness of autistic people’s moral drives. Conversely, psychopathic people may have low moral values (particularly for care and fairness), yet usually strong moral reasoning skills, cognitive empathy, and mentalizing abilities. This contrast adds to the literature in part through emphasizing basic sensory and motor differences, in transaction with the social environment and life experience, as underlying these personality-relevant ii distinctions between autism and psychopathy. It thus attempts to embody both conditions, with the understanding that all behavior involves motor activity, and to think of both conditions as neurodevelopmental in their origins and early trajectories. Such an analysis raises the importance of strengths, as a matter of individual differences as well as influences from the environment, that can help to distinguish and even cause the conditions. -

Females with Fragile X Syndrome: an Overview
FEMALES WITH FRAGILE X SYNDROME: AN OVERVIEW By Ave M. Lachiewicz, MD Duke University Child Development Center Chapel Hill, NC 919-684-5513 Many articles have been written on females with Fragile X syndrome. The purpose of this article is to summarize some of what we know about females who carry the fragile X gene (or the FMR-1 gene). Early articles on fragile X syndrome reported that up to 30% of mothers of children with fragile X syndrome were mentally retarded. In those days there were no DNA studies, and chromosome studies were not accurate enough to detect all females with fragile X syndrome so the information was limited. The fact that so many mothers of children with fragile X syndrome were mentally retarded may not be surprising to lay people but it was to scientists because females with fragile X syndrome have two X chromosomes and only one of the chromosomes usually have an abnormal gene. Many scientists expected that the chromosome that did not carry the fragile X gene would have offered more protection to these women. This happens to be true for other genetic disorders that are associated with abnormalities of the X chromosome, like hemophilia. For some of us in medicine who have worked with other organ systems besides the brain, this information was very surprising, too -- after all if you lose a kidney you still function well because you have another kidney. If you lose a lobe of a lung, there are others. Clearly the systems in the brain that are affected by fragile X are not as expendable and a high percentage of women with fragile X syndrome have cognitive problems because they do not have two normal FMR1 genes. -
CEC Newsletter (Fall 2008).Pub
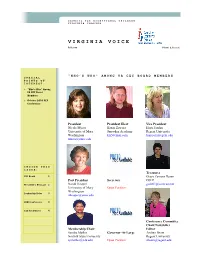
COUNCIL FOR EXCEPTIONAL CHILDREN VIRGINIA CHAPTER VIRGINIA VOICE Fall 2008 Volume 1, Issue 1 “WHO’S WHO” AMONG VA CEC BOARD MEMBERS SPECIAL POINTS OF INTEREST: > “Who’s Who” Among VA CEC Board Members > October 2008 CEC Conference President President Elect Vice President Nicole Myers Karen Zawora Hope Jordan University of Mary Snowden Academy Regent University Washington [email protected] [email protected] [email protected] INSIDE THIS ISSUE: Treasurer CEC Board 1 Grace Zamora Duran Past President Secretary OSEP President’s Message 2 Norah Hooper [email protected] University of Mary Open Position Washington Leadership Roles 3 [email protected] 2008 Conference 4 Call for Articles 4 Conference Committee Chair/Newsletter Membership Chair Editor Sandra Mathis Governor-At-Large Andrea Beam Norfolk State University Regent University [email protected] Open Position [email protected] VIRGINIA VOICE Page 2 PRESIDENT’S MESSAGE BY NICOLE MYERS Welcome to Putting the Severe language prob- Solomon,” where VA Pieces Together: Vir- lems, Severe regulatory CEC members will hear ginia CEC’s 49th Annual problems, Down Syn- Dr. Solomon talk about Conference! drome, Fragile X Syn- autism in the community drome, Fetal Alcohol and include time for par- We are pleased to an- Syndrome, Cerebral ticipant questions. This nounce this year’s con- Palsy, Severe forms of free event co-sponsored ference theme: Putting Attention Deficit Disor- by University of Mary the Pieces Together! Our der, and Autism. Dr. Washington will allow theme serves as a simple Solomon has trained conference participants reminder that special hundreds of profession- and community members education encompasses als and families in work- the opportunity to speak many different issues at ing with children using with Dr. -

Fragile X Syndrome
European Journal of Human Genetics (2008) 16, 666–672 & 2008 Nature Publishing Group All rights reserved 1018-4813/08 $30.00 www.nature.com/ejhg PRACTICAL GENETICS In association with Fragile X syndrome Fragile X syndrome, an X-linked dominant disorder with reduced penetrance, is associated with intellectual and emotional disabilities ranging from learning problems to mental retardation, and mood instability to autism. It is most often caused by the transcriptional silencing of the FMR1 gene, due to an expansion of a CGG repeat found in the 50-untranslated region. The FMR1 gene product, FMRP, is a selective RNA-binding protein that negatively regulates local protein synthesis in neuronal dendrites. In its absence, the transcripts normally regulated by FMRP are over translated. The resulting over abundance of certain proteins results in reduced synaptic strength due to AMPA receptor trafficking abnormalities that lead, at least in part, to the fragile X phenotype. In brief Genetic testing for this repeat expansion is diagnostic for this syndrome, and testing is appropriate in all Fragile X syndrome is a common inherited form of children with developmental delay, mental retardation mental retardation that can be associated with features or autism. of autism. Fragile X syndrome is inherited from individuals, The physical features of fragile X syndrome are subtle usually females, who typically carry an unstable and may not be obvious. premutation allele of the CGG-repeat tract in The vast majority of cases of fragile X syndrome are FMR1. caused by the expansion to over 200 copies of a CGG Premutation carriers are themselves at risk of prema- repeat in the 50-untranslated region of FMR1 that shuts ture ovarian failure and the fragile X-associated tremor/ off transcription of the gene. -

Early Negative Affect in Males and Females with Fragile X Syndrome: Implications for Anxiety and Autism
University of South Carolina Scholar Commons Faculty Publications Psychology, Department of 9-13-2019 Early Negative Affect in Males and Females With Fragile X Syndrome: Implications for Anxiety and Autism Carla A. Will Abigail L. Hogan Elizabeth A. Will Samuel McQuillin Bridgette L. Kelleher See next page for additional authors Follow this and additional works at: https://scholarcommons.sc.edu/psyc_facpub Part of the Psychology Commons Author(s) Carla A. Will, Abigail L. Hogan, Elizabeth A. Will, Samuel McQuillin, Bridgette L. Kelleher, and Jane E. Roberts Wall et al. Journal of Neurodevelopmental Disorders (2019) 11:22 https://doi.org/10.1186/s11689-019-9284-y RESEARCH Open Access Early negative affect in males and females with fragile X syndrome: implications for anxiety and autism Carla A. Wall1* , Abigail L. Hogan1, Elizabeth A. Will1, Samuel McQuillin1, Bridgette L. Kelleher2 and Jane E. Roberts1 Abstract Background: Fragile X syndrome (FXS) is a genetic disorder that is highly comorbid with anxiety and autism spectrum disorder (ASD). Elevated negative affect in young children has been associated with increased risk for both anxiety and ASD; however, these relations remain poorly understood in FXS. Methods: The present prospective longitudinal study examined the trajectory of negative affect from infancy through preschool in males and females with FXS and typical development and its relation to anxiety and ASD. Results: Results indicate a complex association reflecting group, developmental, and sex effects. Specifically, the group with FXS displayed a trajectory of increasing negative affect across age that was distinct from the typical controls. This atypical trajectory of negative affect in FXS was driven by sex effects in that males showed lower negative affect during infancy followed by steep increases across the toddler and preschool years whereas the females displayed a flatter trajectory.