Uganda Work Plan FY 2018 Project Year 7
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HIV/AIDS Treatment and Care in a Long-Term Conflict Setting: Observations from the AIDS Support Organization (TASO) in the Teso Region Emma Smith SIT Study Abroad
SIT Graduate Institute/SIT Study Abroad SIT Digital Collections Independent Study Project (ISP) Collection SIT Study Abroad Spring 2008 HIV/AIDS Treatment and Care in a Long-Term Conflict Setting: Observations From The AIDS Support Organization (TASO) in the Teso Region Emma Smith SIT Study Abroad Follow this and additional works at: https://digitalcollections.sit.edu/isp_collection Recommended Citation Smith, Emma, "HIV/AIDS Treatment and Care in a Long-Term Conflict Setting: Observations From The AIDS Support Organization (TASO) in the Teso Region" (2008). Independent Study Project (ISP) Collection. 99. https://digitalcollections.sit.edu/isp_collection/99 This Unpublished Paper is brought to you for free and open access by the SIT Study Abroad at SIT Digital Collections. It has been accepted for inclusion in Independent Study Project (ISP) Collection by an authorized administrator of SIT Digital Collections. For more information, please contact [email protected]. HIV/AIDS Treatment and Care in a Long-Term Conflict Setting: Observations from The AIDS Support Organization (TASO) in the Teso Region Emma Smith Advisor: Alutia Samuel Academic Directors: Charlotte Mafumbo and Martha Wandera Location: TASO Soroti SIT Uganda Spring 2008 Dedication To all the people living with HIV/AIDS in Teso, who continue to live strongly despite decades of suffering from continuous war, displacement and neglect. May the world come to recognize the struggles that you live with. Acknowledgements There are so many people to whom thanks is owed, it would not be possible to acknowledge them all even if time and space allowed. Primarily, I would like to thank the clients of TASO Soroti, who so willingly welcomed a stranger into their communities and allowed so many questions to be asked of them. -
BETTER GROWTH, BETTER CITIES Achieving Uganda’S Development Ambition
BETTER GROWTH, BETTER CITIES Achieving Uganda’s Development Ambition A paper by the Government of Uganda and the New Climate Economy Partnership November 2016 THE REPUBLIC OF UGANDA THE REPUBLIC OF UGANDA About this paper The analysis in this paper was produced for the New Climate Partnership in Uganda research project, culminating in the report, Achieving Uganda’s Development Ambition: The Economic Impact of Green Growth – An Agenda for Action. This National Urban Transition paper is published as a supporting working paper and provides a fuller elaboration of the urbanisation elements in the broader report. Partners Achieving Uganda’s Development Ambition: The Economic Impact of Green Growth – An Agenda for Action was jointly prepared by the Government of Uganda through the Ministry of Finance, Planning and Economic Development (MFPED), the Ugandan Economic Policy Research Centre (EPRC) Uganda, the Global Green Growth Institute (GGGI), the New Climate Economy (NCE), and the Coalition for Urban Transitions (an NCE Special Initiative). Ministry of Finance, Planning and Economic Development Plot 2/12 Apollo Kaggwa Road P.O.Box 8147 Kampala, Uganda +256-414-707000 COALITION FOR URBAN TRANSITIONS A New Climate Economy Special Initiative Acknowledgements The project team members were Russell Bishop, Nick Godfrey, Annie Lefebure, Filippo Rodriguez and Rachel Waddell (NCE); Madina Guloba (EPRC); Maris Wanyera, Albert Musisi and Andrew Masaba (MPFED); and Samson Akankiza, Jahan-zeb Chowdhury, Peter Okubal and John Walugembe (GGGI). The technical -

Uganda Decentralization: Governance Adrift | 3
African Studies Quarterly | Volume 11, Issue 4 | Summer 2010 Decentralization and Conflict in Uganda: Governance Adrift TERRELL G. MANYAK & ISAAC WASSWA KATONO Abstract: This study examines the challenges that threaten one of Africa’s most ambitious experiments in political, administrative and fiscal decentralization. Based on extensive interviews with local government leaders throughout Uganda, the research uncovered a complex interplay of conflicts that impact decision-making effectiveness. The sources of these conflicts center around (a) the impact of national politics on local government as the country approaches the 2011 election, (b) the inability to meet rising citizen demand for services as the tax base of local governments continues to erode, (c) the corrosive impact of social conflicts stemming mostly from poverty and illiteracy complicated by tribal and ethnic differences, and (d) the challenges of developing honest and effective leadership in local government. Can Uganda unravel this web of conflicts to bring meaningful governance to this young nation? Indeed, many countries within the developing world are watching this experiment with a great deal of interest. Introduction The Uganda experiment in local government was born out of a blend of idealism and practical necessity. The idealism arose from a nation that dedicated itself to building democracy after years of brutal despotism. The practical necessity came from the need to provide basic services in an environment where local government had essentially disintegrated. The result was a multilayered system of directly elected district and lower local councils with significant responsibilities for delivering basic services. The international community strongly supported this action and hailed it as an example of how other developing countries should proceed with nation-building.1 While the local government system was initially well accepted, Ugandans now appear increasingly disenchanted with the corruption, mismanagement, and bitter political conflicts that are regularly reported in local newspapers. -
BUD2-21-Report-On-Th
PARLIAMENT OF UGANDA THE REPORT OF THE COMMITTEE ON BUDGET ON THE APPROPRIATION BILL 2021 OFFICE OF THE CTERK TO PARIIAMENT PARTIAMENT BUILDINGS KAMPAI.A. UGANDA =') Moy 2021 (.., THE REPORT OF THE COMMITTEE ON BUDGET ON THE APPROPRIATION BItL 2O2I I.O INTRODUCTION Rt. Hon. Speoker ond Hon. Members, on lsrApril 2021 the Appropnotion Brll 202lwos reod for lhe first time ond subsequently referred to the Committee on Budgel for considerotion. ln occordonce with rule 170(3) (c), the commiltee considered the Bill ond reports os follows; I.'I MEIHODOLOGY The Commrltee held consullolive meetrngs with the Minrster of Frnonce, Plonning ond Economic Development; ond exomined the Appropriotion Brll to oscertoin lhe consistency ond occurocy of the estimotes os indicoted in the Schedule to the Appropriotion Bill ogoinst ihe Resolution by Porlioment on the some. 1,2 OBJECT OF THE BITL The object of the Bill is to provide for; o) lhe outhorizotron of public expendilure oui of the Consolidoled Fund of o sum of twenty-seven lrillion, six hundred twenty billion, seven hundred ninely six million, lhree hundred sixty lhree lhousond shillings only; ond b) wilhdrowol of Funds from ihe Petroleum Fund into the Consolidoled Fund o sum of two hundred billion shillings only, to meet expendilure for the Finonciol Yeor 2021 /2022 ond to oppropriote the supplies gronted. 2.OLEGAL FRAMEWORK ,l55 2.1 Arlicle ( l ) provides thot; "fhe heods of expendilure confoined in ,he esfimoles, other lhon expendilure chatged on lhe Consolidoted Fund by lhis Conslilulion or ony Act of Porliomenf, sholl be included in o bill lo be known os on Appropriotion Bill which sholl be inlroduced into Porlioment to provide for fhe issue from the Consolidofed Fund of lhe sums necessory meel lhal expenditure ond the oppropriotion of lhose sums for lhe purposes speclfled in the bill." J 2 u 2.2 Additionolly under S. -

A Monthly Newsletter on Food Security and Vulnerability in Uganda
A Monthly Newsletter on Food Security and Vulnerability in Uganda Number 02/2001 15 February, 2001 Summary The NGO, Concern Worldwide, reports that households in Katakwi District (eastern Uganda) are experiencing moderate food insecurity. The most affected people are located in Kapelebyong and Usuk Counties on the border with Moroto District, where there is limited access to food and malnutrition rates are high. Only households in Magoro Sub-County of Usuk, received about 100 kg of maize and beans from another NGO, Hands on Service, in early December. No further assistance has been provided and there are no immediate plans to provide additional food aid to the affected people in the district. Because of the expected increase in demand on meager food supplies and other resources, many residents are worried about the Karimojong pastoralists and their normal dry season migratory pattern into Katakwi District in search of water and pastures for their livestock. Large livestock herds may cause destruction of crops and vegetation, increasing vulnerability to food insecurity and competition for already diminishing pastures. District authorities and local residents also are concerned about the possibility of increasing tensions and civil insecurity due to the presence of armed pastoralists. To ensure peace and security in the district, the Government has increased deployment of Uganda People’s Defence Force personnel. Concern Worldwide affirms that even though the population may require assistance after February 2001 when household food stocks run low, it is imperative for adequate civil security to be maintained to allow proper identification and targeting of the most affected households before carrying out any mitigation program for maximum benefit. -

Thursday, 22 July 2021
PARLIAMENT OF UGANDA Thursday, 22 July 2021 Parliament met at 2.19 p.m. in Parliament House, Kampala. PRAYERS (The Deputy Speaker, Ms Anita Among, in the Chair.) The House was called to order. COMMUNICATION FROM THE CHAIR THE DEPUTY SPEAKER: Honourable members, I welcome you to today’s sitting. This is a reminder about a meeting for the Verification Committee on the by-elections to the East African Legislative Assembly (EALA), pursuant to paragraph 9 of the Rules of Procedure on the election of Members of EALA, contained in Appendix B of the Rules of Procedure of the Parliament of Uganda. This House yesterday duly approved the membership of the Verification Committee to vet the suitability of the candidates for the EALA seat. That committee will sit tomorrow on 23 July 2021 at 10.00 a.m. in the Members’ Lounge, located opposite the parliamentary canteen. The notice of the Monday, 26 July 2021 sitting is about the by-election to fill the vacancy of Uganda’s representative to the EALA. So, I call upon all of you to come and exercise your constitutional rights in choosing that EALA Member of Parliament. This is pursuant to General Notice 875 of 2021 that was published in the Uganda Gazette CX4/114/No. 58 of 19 July 2021; it notified the public about that by- election. We will be sending out the names. Remember, the deadline is Tuesday, 27 July and so, we need to have this by-election on Monday. Today, we have a very short agenda, which involves the House receiving responses to the urgent questions raised by honourable members, prior to us delving into the Prime Minister’s Question Time. -

REPUBLIC of UGANDA Public Disclosure Authorized UGANDA NATIONAL ROADS AUTHORITY
E1879 VOL.3 REPUBLIC OF UGANDA Public Disclosure Authorized UGANDA NATIONAL ROADS AUTHORITY FINAL DETAILED ENGINEERING Public Disclosure Authorized DESIGN REPORT CONSULTANCY SERVICES FOR DETAILED ENGINEERING DESIGN FOR UPGRADING TO PAVED (BITUMEN) STANDARD OF VURRA-ARUA-KOBOKO-ORABA ROAD Public Disclosure Authorized VOL IV - ENVIRONMENTAL AND SOCIAL IMPACT ASSESSMENT Public Disclosure Authorized The Executive Director Uganda National Roads Authority (UNRA) Plot 11 Yusuf Lule Road P.O.Box AN 7917 P.O.Box 28487 Accra-North Kampala, Uganda Ghana Feasibility Study and Detailed Design ofVurra-Arua-Koboko-Road Environmental Social Impact Assessment Final Detailed Engineering Design Report TABLE OF CONTENTS o EXECUTIVE SUMMARY .............................................................................................................. 0-1 1 INTRODUCTION ............................................................................................................................ 1-1 1.1 BACKGROUND OF THE PROJECT ROAD........................................................................................ I-I 1.3 NEED FOR AN ENVIRONMENTAL SOCIAL IMPACT ASSESSMENT STUDy ...................................... 1-3 1.4 OBJECTIVES OF THE ESIA STUDY ............................................................................................... 1-3 2 APPROACH AND METHODOLOGY .......................................................................................... 2-1 2.1 INITIAL MEETINGS WITH NEMA AND UNRA............................................................................ -
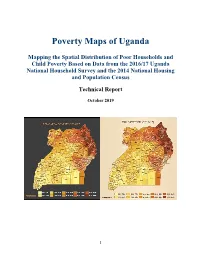
Poverty Map Report
Poverty Maps of Uganda Mapping the Spatial Distribution of Poor Households and Child Poverty Based on Data from the 2016/17 Uganda National Household Survey and the 2014 National Housing and Population Census Technical Report October 2019 1 Acknowledgement This technical report presents the results of the Uganda poverty map update exercise, which was conducted by the Uganda Bureau of Statistics (UBOS) in close collaboration with UNICEF and the World Bank. The core task team at UBOS consisted of Mr. James Muwonge (Director of Socio-Economic Surveys), Mr. Justus Bernard Muhwezi (Manager of Geo-Information Services), Mr. Stephen Baryahirwa (Principal Statistician and Head of the Household Surveys Unit), Mr. Vincent Ssennono (Principal Statistician and Head of the Methodology and Analysis Unit), and Mr. Adriku Charles (Senior Geo-Information Officer). The core task team at the World Bank consisted of Dr. Nobuo Yoshida (Lead Economist), Dr. Carolina Mejia-Mantilla (Uganda Country Poverty Economist), Dr. Minh Cong Nguyen (Senior Economist) and Ms. Miyoko Asai (Consultant). Dr. Nobuo Yoshida and Dr. Minh Cong Nguyen supervised the exercise and ensured that the latest international experience and technical innovations were available to the team. The core task team in UNICEF consisted of Dr. Diego Angemi (Chief Social Policy and Advocacy), Mr. Arthur Muteesasira (Information Management and GIS Officer), and Ms. Sarah Kabaija (Monitoring and Evaluation Specialist). The team benefited from the support and guidance provided by Dr. Robin D. Kibuka(Chairman of the Board, UBOS), Ms. Doreen Mulenga (Country Representative, UNICEF), Mr. Antony Thompson (Country Manager, World Bank), and Dr. Pierella Paci (Practice Manager, World Bank). -

Dairy Development in Uganda
DAIRY DEVELOPMENT IN UGANDA MinistryThe Republic of Agriculture of Uganda Animal Industry and Fisheries (MAAIF) Food and Agriculture A Review of Uganda’s Dairy Industry Organization of the United Nations Dairy Development Authority (DDA) Author: David Balikowa National Consultant, GOU/FAO Dairy Project, TCP/UGA/3202(D); Senior Business Advisor, TechnoServe/East Africa Dairy Development Project (EADD) March 2011 i TABLE OF CONTENTS LIST OF TABLES .................................................................................................................................. v LIST OF FIGURES ................................................................................................................................ v ACRONYMS AND ABBREVIATIONS .....................................................................................................vi EXECUTIVE SUMMARY ...................................................................................................................... vii CHAPTER 1 ........................................................................................................................................ 1 1. INTRODUCTION ......................................................................................................................... 1 1.1 Geographical Location of Uganda ....................................................................................... 1 1.2 Contribution of Agriculture to the National Economy ......................................................... 1 1.3 Historical Overview of -

DOWNLOAD IPC Uganda Acutefi Situation
REPORT OF THE INTEGRATED FOOD SECURITY PHASE CLASSIFICATION ANALYSIS FOR UGANDA PREPARED BY UGANDA IPC TECHNICAL WORKING GROUP January 2016 1 Table of Contents Table of Contents .................................................................................................................................... 2 Acronyms ................................................................................................................................................. 4 CHAPTER ONE .......................................................................................................................................... 6 1.0 FOOD SECURITY ANALYSIS METHODOLOGY AND SCOPE ............................................................ 6 1.1 Background .......................................................................................................................................... 6 1.2 IPC Approach ....................................................................................................................................... 6 1.3 Acute Food Insecurity Analysis- November 2015 to April 2016 ................................................... 7 1.4 Methodology ....................................................................................................................................... 7 1.5 Limitations ........................................................................................................................................... 8 1.6 Summary Findings .............................................................................................................................. -
Emergency Health Fiscal and Growth Stabilization and Development
LIST OF COVID-19 QUARANTINE CENTRES IN WATER AND POWER UTILITIES OPERATION AREAS WATER S/N QUARANTINE CENTRE LOCATION POWER UTILITY UTILITY 1 MASAFU GENERAL HOSPITAL BUSIA UWS-E UMEME LTD 2 BUSWALE SECONDARY SCHOOL NAMAYINGO UWS-E UMEME LTD 3 KATAKWI ISOLATION CENTRE KATAKWI UWS-E UMEME LTD 4 BUKWO HC IV BUKWO UWS-E UMEME LTD 5 AMANANG SECONDARY SCHOOL BUKWO UWS-E UMEME LTD 6 BUKIGAI HC III BUDUDA UWS-E UMEME LTD 7 BULUCHEKE SECONDARY SCHOOL BUDUDA UWS-E UMEME LTD 8 KATIKIT P/S-AMUDAT DISTRICT KATIKIT UWS-K UEDCL 9 NAMALU P/S- NAKAPIRIPIRIT DISTRICT NAMALU UWS-K UEDCL 10 ARENGESIEP S.S-NABILATUK DISTRICT ARENGESIEP UWS-K UEDCL 11 ABIM S.S- ABIM DISTRICT ABIM UWS-K UEDCL 12 KARENGA GIRLS P/S-KARENGA DISTRICT KARENGA UWS-K UMEME LTD 13 NAKAPELIMORU P/S- KOTIDO DISTRICT NAKAPELIMORU UWS-K UEDCL KOBULIN VOCATIONAL TRAINING CENTER- 14 NAPAK UWS-K UEDCL NAPAK DISTRICT 15 NADUNGET HCIII -MOROTO DISTRICT NADUNGET UWS-K UEDCL 16 AMOLATAR SS AMOLATAR UWS-N UEDCL 17 OYAM OYAM UWS-N UMEME LTD 18 PADIBE IN LAMWO DISTRICT LAMWO UWS-N UMEME LTD 19 OPIT IN OMORO OMORO UWS-N UMEME LTD 20 PABBO SS IN AMURU AMURU UWS-N UEDCL 21 DOUGLAS VILLA HOSTELS MAKERERE NWSC UMEME LTD 22 OLIMPIA HOSTEL KIKONI NWSC UMEME LTD 23 LUTAYA GEOFREY NAJJANANKUMBI NWSC UMEME LTD 24 SEKYETE SHEM KIKONI NWSC UMEME LTD PLOT 27 BLKS A-F AKII 25 THE EMIN PASHA HOTEL NWSC UMEME LTD BUA RD 26 ARCH APARTMENTS LTD KIWATULE NWSC UMEME LTD 27 ARCH APARTMENTS LTD KIGOWA NTINDA NWSC UMEME LTD 28 MARIUM S SANTA KYEYUNE KIWATULE NWSC UMEME LTD JINJA SCHOOL OF NURSING AND CLIVE ROAD JINJA 29 MIDWIFERY A/C UNDER MIN.OF P.O.BOX 43, JINJA, NWSC UMEME LTD EDUCATION& SPORTS UGANDA BUGONGA ROAD FTI 30 MAAIF(FISHERIES TRAINING INSTITUTE) NWSC UMEME LTD SCHOOL PLOT 4 GOWERS 31 CENTRAL INN LIMITED NWSC UMEME LTD ROAD PLOT 2 GOWERS 32 CENTRAL INN LIMITED NWSC UMEME LTD ROAD PLOT 45/47 CHURCH 33 CENTRAL INN LIMITED NWSC UMEME LTD RD CENTRAL I INSTITUTE OF SURVEY & LAND PLOT B 2-5 STEVEN 34 NWSC 0 MANAGEMENT KABUYE CLOSE 35 SURVEY TRAINING SCHOOL GOWERS PARK NWSC 0 DIVISION B - 36 DR. -

Minority Rights Group International, Maragoli Community Association
JOINT SUBMISSION TO THE OFFICE OF THE HIGH COMMISSIONER FOR HUMAN RIGHTS ON THE OCCASION OF UGANDA’S 3RD CYCLE UNIVERSAL PERIODIC REVIEW, 40TH SESSION, JANUARY-FEBRUARY 2022 Submission by Minority and Indigenous Groups Report on Health and Education, July 2021 Joint Submission by: Minority Rights Group International, Maragoli Community Association, Benet Lobby Group, North Karamoja Indigenous Minority Group Platform, African International Christian Ministries, United Organization for Batwa Development in Uganda, Action for Batwa Empowerment Group, Eliana R’s and Jamp Banyabindi Foundation, Buliisa District Union of persons with Disabilities, Tapac Integrated Development Organization, Mount Elgon Benet Ogiek Group Organization. 1 CO-SUBMITTING ORGANISATIONS Organization Address Organization Contact Person Maragoli P.O Box 34 Kigumba, Mwale Paul Community Kiryandongo District. 0777 313 677 Association [email protected] (MCA) Maragoli Community Association (MCA) is a non-governmental organization Founded in 1998 and registered as a CBO in 2016. MCA was Formed to Fight For recognition oF the Maragoli as one oF the indigenous communities in Uganda. In addition to citizenship recognition, MCA works towards ensuring that Maragoli community members enjoy Full rights to social services such as health and education and other political rights like any other citizens oF Uganda. MCA currently operates in the districts oF Kiryandongo, Masindi, Hoima, Bugiri and Iganga. African [email protected] Nabimanya Precious Arinda International www.aicmuganda.org 0773 300 302 Christian www.aicm.org.uk Ministries (AICM) P.O. Box: 459 Kampala , Uganda African International Christian Ministry (AICM) is a non-governmental, non-denominational, nonpartisan and a non-proFit making organization which was Founded in 1983.