HHOSC SEP1919R03 Appendix A- CLU Trust Replies (Final)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Quarter 7 Duplicate Removal Process
Quarter 7 Duplicate Removal Process Guidance Total number of records submitted via the web tool (ie Stroke / All records (of any diagnosis) for patients who arrived at hospital TIA / Other) between 1 October 2012 and 31 December 2013 which were locked on the SINAP web tool by 21 January 2013. Number of stroke records submitted via the web tool As above, except that stroke was the diagnosis (as opposed to TIA/Other). Total number of records after cleaning (ie duplicate removals) Records assumed to be duplicates are those that have all of the following fields identical: hospital, date of patient arrival at hospital, gender, age and diagnosis. This may mean that some records that were not real duplicates are removed, but this is proportionally only a small number of those removed, whereas the vast majority will be duplicates. This has been identified as the most appropriate method for removing duplicate records. Percentage of records submitted included after cleaning The percentage represents the proportion of records included in the quarter 7 report after the data cleaning process, this is listed below as total records and stroke records. Total Percentage Percentage Stroke Stroke Total number of number of of stroke of all records records records records submitted records records submitted submitted included SHA Trust Hospital via the webtool in included submitted included in via the after Quarter 7 after included in Quarter 7 webtool in cleaning (Stroke/TIA/Other) cleaning Quarter 7 Report Quarter 7 Quarter 7 Quarter 7 Report East Chesterfield -

Bath's 'Foundered Strata' - a Re-Interpretation
Bath's 'foundered strata' - a re-interpretation Physical Hazards Programme Research Report OR/08/052 BRITISH GEOLOGICAL SURVEY PHYSICAL HAZARDS PROGRAMME RESEARCH REPORT OR/08/052 Bath's 'foundered strata' – a re-interpretation P.R.N. Hobbs and G.O. Jenkins The National Grid and other Ordnance Survey data are used Contributor with the permission of the Controller of Her Majesty’s Stationery Office. A. Forster Ordnance Survey licence number Licence No:100017897/2004. Keywords Bath, landslides, cambering, foundering, geohazards, slope stability, mass movement. Front cover Cover picture details, delete if no cover picture. Bibliographical reference P.R.N. HOBBS AND G.O. JENKINS. 2008 Bath's 'foundered strata' - a re-interpretation. British Geological Survey Research Report, OR/08/052. 40pp. Copyright in materials derived from the British Geological Survey’s work is owned by the Natural Environment Research Council (NERC) and/or the authority that commissioned the work. You may not copy or adapt this publication without first obtaining permission. Contact the BGS Intellectual Property Rights Section, British Geological Survey, Keyworth, e-mail [email protected] You may quote extracts of a reasonable length without prior permission, provided a full acknowledgement is given of the source of the extract. © NERC 2008. All rights reserved Keyworth, Nottingham British Geological Survey 2008 BRITISH GEOLOGICAL SURVEY The full range of Survey publications is available from the BGS British Geological Survey offices Sales Desks at Nottingham, Edinburgh and London; see contact details below or shop online at www.geologyshop.com Keyworth, Nottingham NG12 5GG The London Information Office also maintains a reference collection of BGS publications including maps for consultation. -

Pacman TEMPLATE
Updated May 2020 National Cardiac Arrest Audit Participating Hospitals The total number of hospitals signed up to participate in NCAA is 194. England Birmingham and Black Country Participant Alexandra Hospital Worcestershire Acute Hospitals NHS Trust Birmingham Heartlands Hospital University Hospital Birmingham NHS Foundation Trust City Hospital Sandwell and West Birmingham Hospitals NHS Trust Good Hope Hospital University Hospital Birmingham NHS Foundation Trust Hereford County Hospital Wye Valley NHS Trust Manor Hospital Walsall Healthcare NHS Trust New Cross Hospital The Royal Wolverhampton Hospitals NHS Trust Russells Hall Hospital The Dudley Group of Hospitals NHS Trust Sandwell General Hospital Sandwell and West Birmingham Hospitals NHS Trust Solihull Hospital University Hospital Birmingham NHS Foundation Trust Queen Elizabeth Hospital, Birmingham University Hospital Birmingham NHS Foundation Trust Worcestershire Royal Hospital Worcestershire Acute Hospitals NHS Trust Central England Participant George Eliot Hospital George Eliot Hospital NHS Trust Glenfield Hospital University Hospitals of Leicester NHS Trust Kettering General Hospital Kettering General Hospital NHS Foundation Trust Leicester General Hospital University Hospitals of Leicester NHS Trust Leicester Royal Infirmary University Hospitals of Leicester NHS Trust Northampton General Hospital Northampton General Hospital NHS Trust Hospital of St Cross, Rugby University Hospitals Coventry and Warwickshire NHS Trust University Hospital Coventry University Hospitals Coventry -

2001 Census Report for Parliamentary Constituencies
Reference maps Page England and Wales North East: Counties, Unitary Authorities & Parliamentary Constituencies 42 North West: Counties, Unitary Authorities & Parliamentary Constituencies 43 Yorkshire & The Humber: Counties, Unitary Authorities & Parliamentary Constituencies 44 East Midlands: Counties, Unitary Authorities & Parliamentary Constituencies 45 West Midlands: Counties, Unitary Authorities & Parliamentary Constituencies 46 East of England: Counties, Unitary Authorities & Parliamentary Constituencies 47 London: County & Parliamentary Constituencies 48 South East: Counties, Unitary Authorities & Parliamentary Constituencies 49 South West: Counties, Unitary Authorities & Parliamentary Constituencies 50 Wales: Unitary Authorities & Parliamentary Constituencies 51 Scotland Scotland: Scottish Parliamentary Regions 52 Central Scotland Region: Parliamentary Constituencies 53 Glasgow Region: Parliamentary Constituencies 54 Highlands and Islands Region: Parliamentary Constituencies 55 Lothians Region: Parliamentary Constituencies 56 Mid Scotland and Fife Region: Parliamentary Constituencies 57 North East Scotland Region: Parliamentary Constituencies 58 South of Scotland Region: Parliamentary Constituencies 59 West of Scotland Region: Parliamentary Constituencies 60 Northern Ireland Northern Ireland: Parliamentary Constituencies 61 41 Reference maps Census 2001: Report for Parliamentary Constituencies North East: Counties, Unitary Authorities & Parliamentary Constituencies Key government office region parliamentary constituencies counties -

Point of Entry
DESIGNATED POINTS OF ENTRY FOR PLANT HEALTH CONTROLLED PLANTS/ PLANT PRODUCTS AND FORESTRY MATERIAL POINT OF ENTRY CODE PORT/ ADDRESS DESIGNATED POINT OF ENTRY AIRPORT FOR: ENGLAND Avonmouth AVO P The Bristol Port Co, St Andrew’s House, Plants/plant products & forestry St Andrew’s Road, Avonmouth , Bristol material BS11 9DQ Baltic Wharf LON P Baltic Distribution, Baltic Wharf, Wallasea, Forestry material Rochford, Essex, SS4 2HA Barrow Haven IMM P Barrow Haven Shipping Services, Old Ferry Forestry material Wharf, Barrow Haven, Barrow on Humber, North Lincolnshire, DN19 7ET Birmingham BHX AP Birmingham International Airport, Birmingham, Plants/plant products B26 3QJ Blyth BLY P Blyth Harbour Commission, Port of Blyth, South Plants/plant products & forestry Harbour, Blyth, Northumberland, NE24 3PB material Boston BOS P The Dock, Boston, Lincs, PE21 6BN Forestry material Bristol BRS AP Bristol Airport, Bristol, BS48 3DY Plants/plant products & forestry material Bromborough LIV P Bromborough Stevedoring & Forwarding Ltd., Forestry material Bromborough Dock, Dock Road South, Bromborough, Wirral, CH62 4SF Chatham (Medway) MED P Convoys Wharf, No 8 Berth, Chatham Docks, Forestry Material Gillingham, Kent, ME4 4SR Coventry Parcels Depot CVT P Coventry Overseas Mail Depot, Siskin Parkway Plants/plant products & forestry West, Coventry, CV3 4HX material Doncaster/Sheffield Robin DSA AP Robin Hood Airport Doncaster, Sheffield, Plants/plant products & forestry Hood Airport Heyford House, First Avenue, material Doncaster, DN9 3RH Dover Cargo Terminal, -
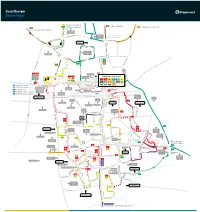
Scunthorpe Route Map
Scunthorpe Route Map 7 Continues as service 8 60 to Burton, Whitton 8 Continues as service 7 350 to Winterton, Barton, Hull 60 to Flixborough, Burton, Whitton Skippingdale Retail Park Ferry Road West Foxhills Outbound morning journeys Phoenix Parkway Industrial Estate Inbound evening journeys L Orbital Rd u rg n Mannabe Way e 8 b 7 u Crosby r g 7 8 W res N C a eedw l Portman Rd o p el y r a F S m er 8 ry CrosbyAv R n oa b d y W e Outwood R s d t Academy The Poplars Foxhills Foxhills Rd Warren Rd 8 Ferry Rd Rd Ferry 4 D 60 e w 8 350 Frodingham Rd s Winterton Rd 60 b u r y A A1077 Orbital Rd v UTC Brigg Rd Scotter Rd Lidl 1 1a Vivian Avenue Marsden Dv Sainsburys Gallagher Stanley Rd 1 1a Scunthorpe Town Centre Retail Park 7 Burn Rd St Lawrences Doncaster Rd 7 35 Academy Bus Station Tesco 1 1a 3 4 x4 7 7 90 60 HiltonAve 8 9 12 35 60 90 Doncaster Rd 360 361 399 350 35 to Amcotts, Crowle Doncaster Rd Cli Gardens d Moors Rd Mary St R d R 90 to Amcotts, Crowle North Lincolnshire r on e Kingsway ati Shopping Park v St to Crowle, Goole o Gardens 360 s Glanford Park 9 Hospital Scunthorpe Scunthorpe ol 361 to Westwoodside, Doncaster B United FC Minster Rd Church Lane Rowland Rd Kingsway 9 399 to Westwoodside, Doncaster Golf Course Midland Brumby Wood Lane Industrial Lodge Moor Brumby Wood Lane eck Rd Estate Steel Scotter Rd B Cottage Works A18 Kingsway The Brumby Pods 1 Wood Rd Ashby Cemetery Rd Quibell Park Brumby Frodingham Central Park UCNL Lilac A Crematorium ve Warwick Rd S a North n The Common Outward d Lindsey h College Academy o P 1a u lymouth -

Name of Deceased
Date before which Name of Deceased - Address, description and date of death of Names, addresses and descriptions of Persons to whom notices of claims are to be notices of claims (Surname first) Deceased given and names, in parentheses, of Personal Representatives to be given SYLVESTER, Derek 31 Albert Marson Court, Scunthorpe, South Beverley & Wood, 99 Mary Street, Scunthorpe. (Anne Jones and Christine 25th August 1982 Wilfred. Humberside, Steelworks Welder. llth Sylvester.) (026) November 1981. THEUNISSEN, Cecil 42 St. Peter Avenue, Bottesford, Scunthprpe, Island Trustees Limited, Hill House, 1 Little New Street, London EC4A 3TR 29th August 1982 Norman. South Humbersides, Headmaster (Retired). (Ref. VJW). (027) 8th April 1982. POWELL, Phyllis '..: Ticehurst House, Ticehurst, Wadhurst, East Jolly & Co., 2lA Palmeira Avenue Mansions, Church Road, Hove, East Sussex 20th August 1982 Sussex, Spinster. 10th July 1981. BN3 2FZ, Solicitors. (Audrey Neale Hardcastle.) (028) BAILEY, Gladys May ... Strathmore, West Hill, Wadebridge, Cornwall, Macmillans, Manor House, Wadebridge, Cornwall PL27 6BS, Solicitors. (Nancy 31st August 1982. Widow of Thomas Howard Bailey. 4th Bate.) (029) March 1982. 15th August 1982 HAZELL, Roland George 29 Birchfield Road, Arnold, Nottingham, Office Robinsons, Market Place, Ilkeston, Derbyshire, Solicitors. (Herbert Arthur (030) Worker. 6th May 1982. Brewer and Arthur Hugh Walford.) BILLANY, Gladys Muriel 4 Springwater Close, Red Lion Lane, London Rich & Carr, 86 Charles Street, Leicester, Solicitors 18th August 1982 S.E.18, Widow. 9th May 1982. (031) PONTING, Albert Eric ... 37 Wildern Square, Stratton St. Margaret, Bevir & Co., 36 Regent Circus, Swindon, Wiltshire SN1 1UQ, Solicitors. 16th August 1982 Swindon, Wiltshire, Crane Driver. 20th (Peter Brian Stanbury and Roger Morcumb.) (032) April 1982. -

Information for Patients
Information for patients Breast Care Service Name: _______________________________ Who to contact and how: _______________________________ Notes: _______________________________ _______________________________ _______________________________ _______________________________ Diana, Princess of Wales Scunthorpe General Goole & District Hospital Hospital Hospital Scartho Road Cliff Gardens Woodland Avenue Grimsby Scunthorpe Goole DN33 2BA DN15 7BH DN14 6RX 03033 306999 03033 306999 03033 306999 www.nlg.nhs.uk www.nlg.nhs.uk www.nlg.nhs.uk For more information about our Trust and the services we provide please visit our website: www.nlg.nhs.uk Information for patients Hello, my name is ………………………………... and I have been identified as your support and contact (key worker). The Macmillan Clinical Nurse Specialists (CNS) for breast cancer have undertaken further studies to develop knowledge within this area of care. We have a practical nursing background of both Breast Surgery and Oncology along with years of experience in both fields. The Team We work within a team of consultants who include: • Consultant Oncoplastic Breast Surgeons • Consultant Breast Surgeons specialising in Breast Surgery • Consultant Breast Surgeons • Consultant Plastic surgeon working at Castle Hill Hospital, Hull, linking with the service locally • Consultant Oncologists • Consultant Radiologists • Consultant Radiographic Practitioner Your named surgeon is:………………………………………………… Your key worker / specialist nurse is:………………………………………………… Your oncologist is:………………………………………………… We are also part of a much larger team of many disciplines and professionals known as the multidisciplinary team (MDT) and also work closely with colleagues in Hull and East Yorkshire Hospitals Trust. Professionals such as advanced nurse practitioners, x-ray specialists and pathologists, as well as the staff within the assessment unit, clinic and reception staff all work together to combine all the necessary expertise to provide you with the best care for your treatment. -

DATASHEET DAT2321/4 Hospital Allocation for Abdominal
DATASHEET DAT2321/4 Effective: 11/02/19 Hospital Allocation for Abdominal NORS Teams - by hospital Copy No: Week 1 scenario - Birmingham (BHAM), Cambridge (CAMB), Edinburgh (EDIN), King's College (KINGS), Manchester (MANC), Newcastle (NEWC), Oxford (OXF) on rota Hospital 1st 2nd ABERDEEN, ABERDEEN ROYAL INFIRMARY EDIN NEWC ABERGAVENNY, NEVILL HALL HOSPITAL BHAM OXF ABERYSTWYTH, BRONGLAIS HOSPITAL BHAM MANC AIRDRIE, MONKLANDS DISTRICT GENERAL HOSPITAL EDIN NEWC ASHFORD, WILLIAM HARVEY HOSPITAL KINGS CAMB ASHINGTON, WANSBECK GENERAL HOSPITAL NEWC EDIN ASHTON-UNDER-LYNE, TAMESIDE GENERAL HOSPITAL MANC BHAM AYLESBURY, STOKE MANDEVILLE HOSPITAL OXF KINGS AYR, THE AYR HOSPITAL EDIN NEWC BANBURY, HORTON GENERAL HOSPITAL OXF BHAM BANGOR, YSBYTY GWYNEDD DISTRICT GENERAL HOSPITAL MANC BHAM BARNET, BARNET GENERAL HOSPITAL CAMB OXF BARNSLEY, BARNSLEY DISTRICT GENERAL HOSPITAL MANC BHAM BARNSTAPLE, NORTH DEVON DISTRICT HOSPITAL BHAM OXF BARROW-IN-FURNESS, FURNESS GENERAL HOSPITAL MANC NEWC BASILDON, BASILDON HOSPITAL CAMB OXF BASINGSTOKE, NORTH HAMPSHIRE HOSPITAL OXF KINGS BATH, ROYAL UNITED HOSPITAL OXF BHAM BEDFORD, BEDFORD HOSPITAL CAMB OXF BELFAST, ANTRIM HOSPITAL EDIN NEWC BELFAST, BELFAST CITY HOSPITAL EDIN NEWC BELFAST, MATER INFIRMORUM HOSPITAL EDIN NEWC BELFAST, ROYAL BELFAST HOSPITAL FOR SICK CHILDREN EDIN NEWC BELFAST, ROYAL VICTORIA HOSPITAL EDIN NEWC BELFAST, THE ULSTER HOSPITAL EDIN NEWC BIRMINGHAM, BIRMINGHAM CHILDREN'S HOSPITAL BHAM OXF BIRMINGHAM, BIRMINGHAM HEARTLANDS HOSPITAL BHAM OXF BIRMINGHAM, CITY HOSPITAL BHAM OXF BIRMINGHAM, -
Scunthorpe & Grimsby
Scunthorpe & Grimsby Group No. 7080 Charity No. 106312 February/Winter Contents Hello and Welcome 1 Where’s the Ad Lad? For Your 2021 Diary Social Nights via Zoom SAGAM Committee Members 2 Composition of Group Chairman’s Annual Report 3 Visit the IAM Shop Associate Extensions A little bit of what you fancy! 4 Caught My Eye 5 History of the Royal Automobile Club Slice of Life – Terry Heath 7 Arctic Quad 8 Laughter is still the Best Medicine It’s Good to Talk 9 Slice of Life – Allen Hardman 11 Are You As Old As You Feel 12 Older Than Grandmas Mouldy Bread! 13 Whatever the Weather – Tyres 14 We Got Mail 15 Support Family and Friends 16 Advertising In Response: Rusty Old Petrol Pumps 17 Sudoku How Well Do You Remember 2020? 18 And Finally To access links, hold down ctrl button and double click. Hello and welcome to the February Edition of the SAGAM Newsletter Well once again, we find ourselves in lockdown. The new variant of the virus seems to be gaining momentum and we have seen the NHS becoming overwhelmed in the last few weeks in some areas. The government seems to have things in hand regarding the vaccination programme so hopefully, we will be able to return to some sort of normal in the near future. Once most of the population have had their vaccination, we just might, be able to return to our social nights. I hope you are managing to keep safe and well and are finding plenty to do to pass the time. -

Local Authority District Codes
UK Data Archive Study Number 6028 - British Household Panel Survey, Waves 1-18, 1991-2009: Conditional Access, Local Authority District Codes British Household Panel Survey, waves 1-18 (1991-2009) User Documentation: Local Authority District Codes (LADISTC) 05 November 2008 For more information contact: Birgitta Rabe [email protected] ++44-1206-874594 Institute for Social and Economic Research University of Essex Wivenhoe Park Colchester Essex CO4 3SQ Local Authority District Codes (wLADISTC) The local authority districts within the database are aggregated if their population falls below 120,000. This aggregation is on the same basis as that for the Census Sample of Anonymised (Individual) Records, and the codes used are the same as those given in Marsh, C. and Teague, A. 'Samples of anonymised records from the 1991 Census', Population Trends, 69, 17-26, 1992. Note that, for wLADISTC, only codes up to 278 are relevant. 1: City; Westminster 53: Newcastle upon Tyne 2: Camden 54: North Tyneside 3: Hackney 55: South Tyneside 4: Hammersmith & Fulham 56: Sunderland 5: Haringey 57: Birmingham 6: Islington 58: Coventry 7: Kensington & Chelsea 59: Dudley 8: Lambeth 60: Sandwell 9: Lewisham 61: Solihull 10: Newham 62: Walsall 11: Southwark 63: Wolverhampton 12: Tower Hamlets 64: Bradford 13: Wandsworth 65: Calderdale 14: Barking and Dagenham 66: Kirklees 15: Barnet 67: Leeds 16: Bexley 68: Wakefield 17: Brent 69: Bath; Kingswood; Wansdyke 18: Bromley 70: Bristol 19: Croydon 71: Northavon 20: Ealing 72: Woodspring 21: Enfield 73: Luton 22: Greenwich -

The Football V Homophobia Fanzine
FANZINE ISSUE: 3 THE FOOTBALL V HOMOPHOBIA FANZINE INSIDE: NOTES FROM THE EDITOR REVIEW OF #FVH2014 HATE ON THE TERRACES FANS’ GROUPS: TOTTENHAM HOTSPUR FANS’ OPINION: CLUBS NEED TO PLAY THEIR PART SUSSEX COUNTY FA FVH IN EUROPE JOURNALISTS’ SEMINAR @FvHtweets Thank you to the Esmée Fairbairn Foundation for funding the fanzine. WELCOME TO STAND OUT! NOTES FROM THE EDITOR What a fabulous February! Our campaign month was The Swedish media have reported the violent assault the most successful in our history, with unprecedented as an anti-Jewish hate crime rather than a homophobic levels of support throughout the game, and this has attack, but the fact remains that a leading anti- provided a fantastic boost for everyone who wants homophobia campaigner has suffered at the hands of to see homophobia, and all other forms of prejudice, those in society who are violently opposed to anyone eradicated from football. different to them. Everyone at FvH wishes Showan the very best in his battle against the injuries that he Over half of the 92 professional league clubs supported suffered, and hope that he makes a full and speedy the campaign, including 15 of the 20 Premier League recovery. teams, alongside a strong number of County FAs, non-league and women’s clubs. In this issue, we have I’m grateful to Ian Cusack and Pete Marshall (Issue 2) highlighted some of those who got involved, but FvH and Joe Taylor (page 13) for submitting their articles for would like to thank everyone who participated and publication this year. I would like this to be a fanzine for made the month such a success.