Use of Simulation to Aid Design of Clinical Trials During Infectious Disease Outbreaks
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

GCCA the Hidden Crisis Reduced
WATER The hidden climate crisis Martin Atkin “An approach to climate change that recognizes the importance of water can combat both the causes and impacts of climate change.” - UN Climate Change WATER: THE HIDDEN CLIMATE CRISIS Water is one of nature’s great paradoxes. Society Network on Water and Sanitation Essential for life on earth, we suffer if there’s (ANEW) told a recent online conference on not enough and we suffer if there’s too much. accelerating action on water and climate at Climate change is increasingly upsetting this COP26. “These women and girls, and their delicate balance. More and more people face daughters’ daughters, will be locked into a life water insecurity both from extreme drought of ill-health, violence and poverty if we fail to and extreme flooding. address the water crisis.” The data is alarming. Half the world’s Covid-19 has highlighted the gross population live in water-scarce areas. By inequalities of water scarcity. “It’s shocking 2025, two-thirds may face water shortages. that right now, forty percent of the global More than two billion people have no safe, population does not have enough water to do clean, easily accessible water supply. 800 adequate hand washing,” says Betsy Otto, million people - most of them women and Director of the Global Water Program at the girls - have to walk more than a kilometre World Resources Institute (WRI). According from their homes to fetch water. Global water to the International Food Policy Research demand has been rising by one percent a year Institute (IFPRI), “In many communities since the 1980s. -

Bulletin Bimestriel D'informations De La
BULLETIN BIMESTRIEL D’INFORMATIONS DE LA FAO - NIGER FAO Niger-INFOS BULLETIN BIMESTRIEL D’INFORMATIONS DE LA FAO - NIGER N°003 DU 31 JUILLET 2017 Sommaire La FAO appuie le Niger avec 657 tonnes de semences améliorées Trois bonnes pratiques de réponses P. 2 © rapides aux risques de catastrophes FAO et à la mise en place de 50 000 tonnes d’engrais. développées au Niger À la fin du mois de juin 2017, seulement 20 606 tonnes La FAO appuie la vulgarisation de P. 2 sont obtenues. l’acte uniforme relatif au droit des sociétés coopératives Dans le cadre de la lutte phytosanitaire, 200 000 litres La FAO appuie le CORESA à dispo- P. 3 sont prévus mais seulement 56 098 litres sont dispo- ser d’un outil d’évaluation des poli- nibles dans les magasins de la Direction Générale des tiques et stratégies de sécurité alimentaire et nutritionnelle dans Produits Vivriers correspondant à une capacité d’interven- quatre pays du Sahel tion de 64 704 ha pour une prévision de 250 000 ha, soit La FAO soutient la production du P.3 une couverture de plus de 26%. riz au profit de 4 000 bénéficiaires nigériens Pour cette campagne pluviale 2017, la contribution de la Le Niger institutionnalise l’approche P. 4 FAO est de 657 tonnes de semences améliorées de mil et champs écoles paysans introduite niébé en faveur des ménages ruraux les plus vulnérables. dans le pays par la FAO Les principaux partenaires financiers de la FAO dans la L’approche champs écoles agro- P.4 pastoraux de la FAO donne satis- mobilisation de ce tonnage sont le Fonds des Nations faction au Niger Unies pour les opérations d’urgence (CERF) et la France. -

F:\Niger En Chiffres 2014 Draft
Le Niger en Chiffres 2014 Le Niger en Chiffres 2014 1 Novembre 2014 Le Niger en Chiffres 2014 Direction Générale de l’Institut National de la Statistique 182, Rue de la Sirba, BP 13416, Niamey – Niger, Tél. : +227 20 72 35 60 Fax : +227 20 72 21 74, NIF : 9617/R, http://www.ins.ne, e-mail : [email protected] 2 Le Niger en Chiffres 2014 Le Niger en Chiffres 2014 Pays : Niger Capitale : Niamey Date de proclamation - de la République 18 décembre 1958 - de l’Indépendance 3 août 1960 Population* (en 2013) : 17.807.117 d’habitants Superficie : 1 267 000 km² Monnaie : Francs CFA (1 euro = 655,957 FCFA) Religion : 99% Musulmans, 1% Autres * Estimations à partir des données définitives du RGP/H 2012 3 Le Niger en Chiffres 2014 4 Le Niger en Chiffres 2014 Ce document est l’une des publications annuelles de l’Institut National de la Statistique. Il a été préparé par : - Sani ALI, Chef de Service de la Coordination Statistique. Ont également participé à l’élaboration de cette publication, les structures et personnes suivantes de l’INS : les structures : - Direction des Statistiques et des Etudes Economiques (DSEE) ; - Direction des Statistiques et des Etudes Démographiques et Sociales (DSEDS). les personnes : - Idrissa ALICHINA KOURGUENI, Directeur Général de l’Institut National de la Statistique ; - Ibrahim SOUMAILA, Secrétaire Général P.I de l’Institut National de la Statistique. Ce document a été examiné et validé par les membres du Comité de Lecture de l’INS. Il s’agit de : - Adamou BOUZOU, Président du comité de lecture de l’Institut National de la Statistique ; - Djibo SAIDOU, membre du comité - Mahamadou CHEKARAOU, membre du comité - Tassiou ALMADJIR, membre du comité - Halissa HASSAN DAN AZOUMI, membre du comité - Issiak Balarabé MAHAMAN, membre du comité - Ibrahim ISSOUFOU ALI KIAFFI, membre du comité - Abdou MAINA, membre du comité. -

CAP 2012 Niger FR.Pdf
QUELQUES ORGANISATIONS PARTICIPANT AUX APPELS GLOBAUX AARREC Humedica CRS MENTOR TGH ACF IA CWS MERLIN UMCOR ACTED ILO DanChurchAid Muslim Aid UNAIDS ADRA IMC DDG NCA UNDP Africare INTERMON Diakonie Emerg. Aid NPA UNDSS AMI-France Internews DRC NRC UNEP ARC INTERSOS EM-DH OCHA UNESCO ASB IOM/ OIM FAO OHCHR UNFPA ASI IPHD FAR OXFAM UN-HABITAT AVSI IR FHI PA UNHCR CARE IRC FinnChurchAid PACT UNICEF CARITAS IRD FSD PAI UNIFEM CEMIR International IRIN GAA Plan UNJLC CESVI IRW GOAL PMU-I UNMAS CFA Islamic Relief GTZ Première Urgence UNOPS CHF JOIN GVC RC/Germany UNRWA CHFI JRS Handicap International RCO VIS CISV LWF HealthNet TPO Samaritan's Purse WFP CMA Malaria Consortium HELP Save the Children WHO CONCERN Malteser HelpAge International SECADEV World Concern COOPI Mercy Corps HKI Solidarités World Relief CORDAID MDA Horn Relief SUDO WV COSV MDM HT TEARFUND ZOA MEDAIR Table des matières 1. RESUME ....................................................................................................................................................... 1 Tableau de bord humanitaire .......................................................................................................................... 3 Table I. Besoins totaux de financement (groupés par groupe sectoriel) .............................................. 7 Table II. Besoins totaux de financement (groupés par niveau de priorité) ............................................ 7 Table III. Besoins totaux de financement (groupés par agence) ............................................................ -

World Bank Document
REPUBLIQUE DU NIGER Fraternité – Travail – Progrès MINISTERE DE L’EQUIPEMENT DIRECTION GENERALE DES ROUTES RURALES DIRECTION DES ETUDES TECHNIQUES Public Disclosure Authorized Unité de Coordination du Projet d’Appui au Désenclavement des Zones Agricoles (PADEZA) Public Disclosure Authorized . RAPPORT D’ETUDE D’IMPACT ENVIRONNEMENTAL ET SOCIAL (REIES) DES ROUTES FINANCEES DANS LE CADRE DU PROJET Public Disclosure Authorized D’APPUI AU DESENCLAVEMENT DES ZONES AGRICOLES (PADEZA) DOSSO-TAHOUA-MARADI AU NIGER Septembre 2018 Public Disclosure Authorized 1 Table des matières Table des matières 2 Liste des Acronymes 6 Liste des tableaux 7 Liste des cartes 9 Liste des photos 9 1. Résumé Non Technique 10 2. Introduction 27 3. Description complète du projet PADEZA 31 3.1. Contexte de la zone du projet 33 3.1.1. Région de Dosso 33 3.1.2. Région de Tahoua 34 3.1.3. Région de Maradi 35 3.2 Etat actuel des routes étudiées 36 3.2.1 Région de Dosso 36 3.2.2 Région de Tahoua 38 3.2.3 Région de Maradi 40 3.4- Caractéristiques des pistes rurales (routes en terre) à construire 42 3.5 Activités du projet 43 3.6 Estimation sommaire des coûts 44 3.7 Recherche de matériaux de chaussée 46 3.7.1 Tronçons de la région de Dosso 48 3.7.2 Tronçons de la région de Tahoua 49 3.7.3 Tronçons de la région de Maradi 49 3.8 Sources d’approvisionnement en eau 51 3.9 Principaux enjeux environnementaux et sociaux du projet 51 4. Description de la situation de référence ou état initial des zones d’études 52 4.1 Situation administrative et géographique 52 2 4.2 Géomorphologie 53 4.3 Hydrographie 54 4.4 Climat et végétation 54 4.5 Faune 56 4.6 Qualité de l’air 56 4.7. -
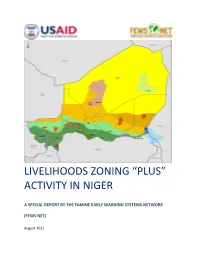
Livelihoods Zoning “Plus” Activity in Niger
LIVELIHOODS ZONING “PLUS” ACTIVITY IN NIGER A SPECIAL REPORT BY THE FAMINE EARLY WARNING SYSTEMS NETWORK (FEWS NET) August 2011 Table of Contents Introduction .................................................................................................................................................. 3 Methodology ................................................................................................................................................. 4 National Livelihoods Zones Map ................................................................................................................... 6 Livelihoods Highlights ................................................................................................................................... 7 National Seasonal Calendar .......................................................................................................................... 9 Rural Livelihood Zones Descriptions ........................................................................................................... 11 Zone 1: Northeast Oases: Dates, Salt and Trade ................................................................................... 11 Zone 2: Aïr Massif Irrigated Gardening ................................................................................................ 14 Zone 3 : Transhumant and Nomad Pastoralism .................................................................................... 17 Zone 4: Agropastoral Belt ..................................................................................................................... -

Analysis of a Meningococcal Meningitis Outbreak in Niger – Potential Effectiveness of Reactive
bioRxiv preprint doi: https://doi.org/10.1101/496299; this version posted December 13, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Analysis of a meningococcal meningitis outbreak in Niger – potential effectiveness of reactive 2 prophylaxis 3 Matt D.T. Hitchings1,*, Matthew E. Coldiron2, Rebecca F. Grais2, Marc Lipsitch3 4 1 Center for Communicable Disease Dynamics and Department of Epidemiology, Harvard T. H. Chan 5 School of Public Health, Boston, MA, USA. 6 2 Epicentre, Paris, France. 7 3 Center for Communicable Disease Dynamics and Departments of Epidemiology and Immunology 8 and Infectious Diseases, Harvard T. H. Chan School of Public Health, Boston, MA, USA. 9 * Email [email protected] 1 bioRxiv preprint doi: https://doi.org/10.1101/496299; this version posted December 13, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 10 Abstract 11 Background 12 Seasonal epidemics of bacterial meningitis in the African Meningitis Belt carry a high burden of 13 disease and mortality. Reactive mass vaccination is used as a control measure during epidemics, but 14 the time taken to gain immunity from the vaccine reduces the flexibility and effectiveness of these 15 campaigns. Highly targeted reactive antibiotic prophylaxis could be used to supplement reactive 16 mass vaccination and further reduce the incidence of meningitis, and the potential effectiveness and 17 efficiency of these strategies should be explored. -

BROCHURE Dainformation SUR LA Décentralisation AU NIGER
REPUBLIQUE DU NIGER MINISTERE DE L’INTERIEUR, DE LA SECURITE PUBLIQUE, DE LA DECENTRALISATION ET DES AFFAIRES COUTUMIERES ET RELIGIEUSES DIRECTION GENERALE DE LA DECENTRALISATION ET DES COLLECTIVITES TERRITORIALES brochure d’INFORMATION SUR LA DÉCENTRALISATION AU NIGER Edition 2015 Imprimerie ALBARKA - Niamey-NIGER Tél. +227 20 72 33 17/38 - 105 - REPUBLIQUE DU NIGER MINISTERE DE L’INTERIEUR, DE LA SECURITE PUBLIQUE, DE LA DECENTRALISATION ET DES AFFAIRES COUTUMIERES ET RELIGIEUSES DIRECTION GENERALE DE LA DECENTRALISATION ET DES COLLECTIVITES TERRITORIALES brochure d’INFORMATION SUR LA DÉCENTRALISATION AU NIGER Edition 2015 - 1 - - 2 - SOMMAIRE Liste des sigles .......................................................................................................... 4 Avant propos ............................................................................................................. 5 Première partie : Généralités sur la Décentralisation au Niger ......................................................... 7 Deuxième partie : Des élections municipales et régionales ............................................................. 21 Troisième partie : A la découverte de la Commune ......................................................................... 25 Quatrième partie : A la découverte de la Région .............................................................................. 53 Cinquième partie : Ressources et autonomie de gestion des collectivités ........................................ 65 Sixième partie : Stratégies et outils -
Report 2020 2
Communities Regreen Half year the Sahel report 2020 2 Half year report 2020 Content 04 Map of Sahel 26 Milestones Burkina Faso 06 Introduction 28 Results Burkina Faso 08 Niger 34 Senegal 10 Map Niger 36 Map Senegal 12 Milestones Niger 38 Milestones Senegal 14 Results Niger 40 Results Senegal 22 Burkina Faso 44 Evaluation and next steps 24 Map Burkina Faso 47 Colophon 3 4 Sahara Sahel NIGER SENEGAL BURKINA FASO 5 Sahel Icons Milestones Collaborations Preview Budget / Finance Specials Policy XOF Personal stories Region Market 6 Introduction Dear reader, 2020. What a ‘year’ this has been already, even REGREENING DURING COVID-19 though we are only halfway! We all started Many African countries, including Burkina Faso, this year with loads of good energy. We were Niger and Senegal, closed their international looking forward to evaluating the first phase of borders and areas around the big cities because of Communities Regreen the Sahel, to attending some the global pandemic. This meant that our partners very interesting international conferences and to could not leave their own region or city for months. continue working with increasingly better equipped As frustrating as this was, our partners kept finding and attuned teams. Fortunately, we had the ways to keep the work going. In fact, this crisis chance to attend and participate in two important pushed the whole consortium to think out of the international conferences on agroecology, box and to come up with creative ways both held in Senegal. At the strategic to keep doing what needed to be regional 3AO meeting (Alliance done. -

«Fichier Electoral Biométrique Au Niger»
«Fichier Electoral Biométrique au Niger» DIFEB, le 16 Août 2019 SOMMAIRE CEV Plan de déploiement Détails Zone 1 Détails Zone 2 Avantages/Limites CEV Centre d’Enrôlement et de Vote CEV: Centre d’Enrôlement et de Vote Notion apparue avec l’introduction de la Biométrie dans le système électoral nigérien. ▪ Avec l’utilisation de matériels sensible (fragile et lourd), difficile de faire de maison en maison pour un recensement, C’est l’emplacement physique où se rendront les populations pour leur inscription sur la Liste Electorale Biométrique (LEB) dans une localité donnée. Pour ne pas désorienter les gens, le CEV servira aussi de lieu de vote pour les élections à venir. Ainsi, le CEV contiendra un ou plusieurs bureaux de vote selon le nombre de personnes enrôlées dans le centre et conformément aux dispositions de création de bureaux de vote (Art 79 code électoral) COLLECTE DES INFORMATIONS SUR LES CEV Création d’une fiche d’identification de CEV; Formation des acteurs locaux (maire ou son représentant, responsable d’état civil) pour le remplissage de la fiche; Remplissage des fiches dans les communes (maire ou son représentant, responsable d’état civil et 3 personnes ressources); Centralisation et traitement des fiches par commune; Validation des CEV avec les acteurs locaux (Traitement des erreurs sur place) Liste définitive par commune NOMBRE DE CEV PAR REGION Région Nombre de CEV AGADEZ 765 TAHOUA 3372 DOSSO 2398 TILLABERY 3742 18 400 DIFFA 912 MARADI 3241 ZINDER 3788 NIAMEY 182 ETRANGER 247 TOTAL 18 647 Plan de Déploiement Plan de Déploiement couvrir tous les 18 647 CEV : Sur une superficie de 1 267 000 km2 Avec une population électorale attendue de 9 751 462 Et 3 500 kits (3000 kits fixes et 500 tablettes) ❖ KIT = Valise d’enrôlement constitués de plusieurs composants (PC ou Tablette, lecteur d’empreintes digitales, appareil photo, capteur de signature, scanner, etc…) Le pays est divisé en 2 zones d’intervention (4 régions chacune) et chaque région en 5 aires. -

Département De Abala Pour Usage Humanitaire Uniquement CARTE DE REFERENCE Date De Production : 21 Mars 2018
Niger - Région de Tillabéri - Département de Abala Pour Usage Humanitaire Uniquement CARTE DE REFERENCE Date de production : 21 mars 2018 3°20'0"E 4°10'0"E "Eknewane "Tagaza Mali " " " "Assagueyguey " Tillia Tahamou " Tillia "Tadroupt " I Karafan Ii Ikarffane I "Tafougaye "Zindar "Maitallakiya "Intedene "Banna Kouara "Tabalolt I "Sine Godar "Langa Kouara "Targuaitamoun " Ta"balolt Ii " Tiguezefan Issa "Bourgett Tiguezefantabre " Ban" izoumbou Saidou Kouara Afantam Tigueze Fan Raoufi " Mai Bado Banibangou " " " Miel " Dan Dabagui "Chimbarkawane " Mimandey "Garin Dogo " Komakoukou Wedo" u Bangou Peulh " N'Bili"bass " " "Agai Agai " " " Garin Ousmane " Weidou Bangou Djerma Indiguini Mali Koara " " Taka Lafia " Darey Tinni "Darey Sossi " Tare Tare " " " Tamalolo "Agaginey " Bouka Balla" "Tillimoune Dogon Dadji "Kabey Bangou " "Fakkata Banibangou Tanagamat Tingar " " " " Tine Greguef Dan "Tare Alwafi Kou"ara " Amouloua "Kizamou Kabouna Abala "Malala "Fadama " " " "Garin Oumba Kontantchi " "Keltizenbet Vi Kizamou Zarma " Tamattey "Adidan Abeyok Tawinass "Tekou Kizamou " " Falanzad" an "Imirizane " Falanzadan Goroutche "Dogon Dadji Amouloua "Dallogi I Et Ii " Fandou Banda " "Arawa "Tsaouna Marafa(Garin Kess " Chrim Elh Moumouni" "Ohitanne Bakin Zango" "Ezza " "Tinigamat Tabotaikit " Abeyok Kim" ba Keltizembei Iii Chrim Elh Salouhou Wiye "Garin Sama Takanamat " " " " Tsalle "Fadama " " "Dogafa Reye Reye Aboye Zada "Matserga " Moza Peulh " Chrim Sarkin Noma Garin Bizo Mandaba " Tagoujel Ga"rin Mai Gari " " "Keltizenbet Ii Dogaga Innaridan I"ntiguidi -

Avis D'appel D'offres NIG017 15
Programme NIG/017 Appui au Programme National de Formation Professionnelle et Technique et d’Insertion des Ministère des Enseignements Jeunes Sortants Professionnels et Technique AVIS D’APPEL D’OFFRES N° NIG/017•15 248 TITRE : Acquisition de matériels de froid (climatiseurs) pour les CFDC-CFPT Dans le cadre du Programme NIG/017 financé sur des ressources des Gouvernements du Grand-Duché de Luxembourg et du Niger Cet avis est lancé par l’Agence luxembourgeoise pour la Coopération au Développement (LuxDev), pour le compte du Programme NIG/017 recevant un appui financier des Gouvernements du Niger et du Grand-Duché de Luxembourg. 1°) Identification et financement du programme a) Intitulé : NIG/017 - Appui au Programme National de Formation Professionnelle et Technique et d’Insertion des Jeunes Sortants b) Numéro : NIG/017•15 248 c) Source de financement : le Gouvernement du Niger et le Gouvernement du Grand-Duché de Luxembourg comme défini dans le Protocole de Programme NIG/017 du 8 juillet 2011. d) Situation du financement : Approuvé 2°) Identification du marché a) Type de marché : biens b) Objet : Acquisition de matériels de froid (climatiseurs) pour les CFDC-CFPT. c) Nombre de lots : Un (1) 3°) Critères d'éligibilité et d'évaluation a) Origine : pas de restriction. b) Éligibilité : les entreprises qui satisfont aux critères inclus dans la Déclaration sur l’honneur et dans les clauses déontologiques de la Réglementation Générale. c) Évaluation : l’attribution sera faite à l’offre évaluée administrativement conforme et techniquement substantiellement conforme, la moins disante. d) Variantes : aucune variante ne sera prise en compte 4°) Lieux et délais a) Localisation du Programme : Niamey, annexe du Ministère des Enseignements Professionnels et Techniques.