Dissertation TYPESET V2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Club Cultures Music, Media and Subcultural Capital SARAH THORNTON Polity
Club Cultures Music, Media and Subcultural Capital SARAH THORNTON Polity 2 Copyright © Sarah Thornton 1995 The right of Sarah Thornton to be identified as author of this work has been asserted in accordance with the Copyright, Designs and Patents Act 1988. First published in 1995 by Polity Press in association with Blackwell Publishers Ltd. Reprinted 1996, 1997, 2001 Transferred to digital print 2003 Editorial office: Polity Press 65 Bridge Street Cambridge CB2 1UR, UK Marketing and production: Blackwell Publishers Ltd 108 Cowley Road Oxford OX4 1JF, UK All rights reserved. Except for the quotation of short passages for the purposes of criticism and review, no part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the publisher. Except in the United States of America, this book is sold subject to the condition that it shall not, by way of trade or otherwise, be lent, re-sold, hired out, or otherwise circulated without the publisher’s prior consent in any 3 form of binding or cover other than that in which it is published and without a similar condition including this condition being imposed on the subsequent purchaser. ISBN: 978-0-7456-6880-2 (Multi-user ebook) A CIP catalogue record for this book is available from the British Library. Typeset in 10.5 on 12.5 pt Palatino by Best-set Typesetter Ltd, Hong Kong Printed and bound in Great Britain by Marston Lindsay Ross International -
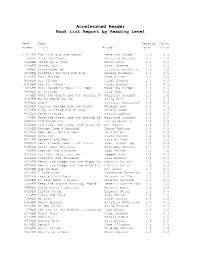
Accelerated Reader Book List Report by Reading Level
Accelerated Reader Book List Report by Reading Level Test Book Reading Point Number Title Author Level Value -------------------------------------------------------------------------- 27212EN The Lion and the Mouse Beverley Randell 1.0 0.5 330EN Nate the Great Marjorie Sharmat 1.1 1.0 6648EN Sheep in a Jeep Nancy Shaw 1.1 0.5 9338EN Shine, Sun! Carol Greene 1.2 0.5 345EN Sunny-Side Up Patricia Reilly Gi 1.2 1.0 6059EN Clifford the Big Red Dog Norman Bridwell 1.3 0.5 9454EN Farm Noises Jane Miller 1.3 0.5 9314EN Hi, Clouds Carol Greene 1.3 0.5 9318EN Ice Is...Whee! Carol Greene 1.3 0.5 27205EN Mrs. Spider's Beautiful Web Beverley Randell 1.3 0.5 9464EN My Friends Taro Gomi 1.3 0.5 678EN Nate the Great and the Musical N Marjorie Sharmat 1.3 1.0 9467EN Watch Where You Go Sally Noll 1.3 0.5 9306EN Bugs! Patricia McKissack 1.4 0.5 6110EN Curious George and the Pizza Margret Rey 1.4 0.5 6116EN Frog and Toad Are Friends Arnold Lobel 1.4 0.5 9312EN Go-With Words Bonnie Dobkin 1.4 0.5 430EN Nate the Great and the Boring Be Marjorie Sharmat 1.4 1.0 6080EN Old Black Fly Jim Aylesworth 1.4 0.5 9042EN One Fish, Two Fish, Red Fish, Bl Dr. Seuss 1.4 0.5 6136EN Possum Come a-Knockin' Nancy VanLaan 1.4 0.5 6137EN Red Leaf, Yellow Leaf Lois Ehlert 1.4 0.5 9340EN Snow Joe Carol Greene 1.4 0.5 9342EN Spiders and Webs Carolyn Lunn 1.4 0.5 9564EN Best Friends Wear Pink Tutus Sheri Brownrigg 1.5 0.5 9305EN Bonk! Goes the Ball Philippa Stevens 1.5 0.5 408EN Cookies and Crutches Judy Delton 1.5 1.0 9310EN Eat Your Peas, Louise! Pegeen Snow 1.5 0.5 6114EN Fievel's Big Showdown Gail Herman 1.5 0.5 6119EN Henry and Mudge and the Happy Ca Cynthia Rylant 1.5 0.5 9477EN Henry and Mudge and the Wild Win Cynthia Rylant 1.5 0.5 9023EN Hop on Pop Dr. -

Reading the Surface: the Danish Gothic of B.S. Ingemann, H.C
Reading the Surface: The Danish Gothic of B.S. Ingemann, H.C. Andersen, Karen Blixen and Beyond Kirstine Marie Kastbjerg A dissertation submitted in partial fulfilment of the requirements for the degree of Doctor of Philosophy University of Washington 2013 Reading Committee: Marianne Stecher. Chair Jan Sjaavik Marshall Brown Program Authorized to Offer Degree: Scandinavian Studies ©Copyright 2013 Kirstine Marie Kastbjerg Parts of chapter 7 are reprinted by permission of the publishers from “The Aesthetics of Surface: the Danish Gothic 1820-2000,” in Gothic Topographies ed. P.M. Mehtonen and Matti Savolainen (Farnham: Ashgate, 2013), pp. 153–167. Copyright © 2013 University of Washington Abstract Reading the Surface: The Danish Gothic of B.S. Ingemann, H.C. Andersen, Karen Blixen and Beyond Kirstine Marie Kastbjerg Chair of the Supervisory Committee: Professor in Danish Studies Marianne Stecher Department of Scandinavian Studies Despite growing ubiquitous in both the popular and academic mind in recent years, the Gothic has, perhaps not surprisingly, yet to be examined within the notoriously realism-prone literary canon of Denmark. This dissertation fills that void by demonstrating an ongoing negotiation of Gothic conventions in select works by canonical Danish writers such as B.S. Ingemann, Hans Christian Andersen, and Karen Blixen (Isak Dinesen), as well as contemporary writers such as Peter Høeg and Leonora Christina Skov. This examination does not only broaden our understanding of these culturally significant writers and the discourses they write within and against, it also adds to our understanding of the Gothic – an infamously malleable and indefinable literary mode – by redirecting attention to a central feature of the Gothic that has not received much critical attention: the emphasis on excess, spectacle, clichéd conventions, histrionic performances, its hyperbolic rhetorical style, and hyper-visual theatricality. -

“The Greatest Gift Is the Realization That Life Does Not Consist Either In
“The greatest gift is the realization that life does not consist either in wallowing in the past or peering anxiously into the future; and it is appalling to contemplate the great number of often painful steps by which ones arrives at a truth so old, so obvious, and so frequently expressed. It is good for one to appreciate that life is now. Whatever it offers, little or much, life is now –this day-this hour.” Charles Macomb Flandrau Ernest Hemingway drank here. Cuban revolutionaries Fidel Castro and Che Guevera drank here. A longhaired young hippie musician named Jimmy Buffett drank and performed here, too. From the 1930’s through today this rustic dive bar has seen more than its share of the famous and the infamous. It’s a little joint called Capt. Tony’s in Key West, Florida. Eighty-seven-year-old Anthony ‘Capt. Tony’ Tarracino has been the owner and proprietor of this boozy establishment since 1959. It seems Tony, as a young mobster, got himself into some serious trouble with ‘the family’ back in New Jersey and needed to lay low for a while. In those days, the mosquito invested ‘keys’ (or islands) on the southernmost end of Florida’s coastline was a fine place for wise guys on the lam to hide out. And this was well before the tee-shirt shops, restaurants, bars, art galleries, charming B&B’s and quaint hotels turned Key West into a serious year-round tourist destination. Sure, there were some ‘artsy’ types like Hemingway and Tennessee Williams living in Key West during the late 50’s when Tony bought the bar, but it was a seaside shanty town where muscular hard-working men in shrimp boats and cutters fished all day for a living. -

Prometheus and Pandora and Macedonian Rag, Two Plays
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 1971 Prometheus and Pandora and Macedonian rag, two plays Gerald D. Giss The University of Montana Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Giss, Gerald D., "Prometheus and Pandora and Macedonian rag, two plays" (1971). Graduate Student Theses, Dissertations, & Professional Papers. 3323. https://scholarworks.umt.edu/etd/3323 This Thesis is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. PROMETHEUS AND PANDORA and MACEDONIAN RAG, TWO PLAY3 By Gerald D. Giss B.S., Northern Arizona University, 1969 Presented in partial fulfillment of the requirements for the drgree of Master of Fine Arts UNIVERSITY OF MONTANA 1971 Approved by: Chairman, Board of Examiners G ra d ua/€^e<^ c h oo1 Date UMI Number: EP34956 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. UMT Dis89rtation Publishing UMI EP34956 Published by ProQuest LLC (2012). Copyright in the Dissertation held by the Author. -

Pandora's Playhouse by Sananda Maitreya Track by Track Volume 1
Interviews By Carl Wiser Pandora’s PlayHouse by Sananda Maitreya Track by Track Sananda Maitreya goes though the songs on his album Pandora’s PlayHouse, explaining the themes and concepts. March 12 , 2021 Life is like a SPOILED SUPERMODEL WHO KNOWS THAT EVERYONE wants TO BE WITH HER Sananda Maitreya could have relaxed into his celebrity, but has instead pushed forward on a quest for meaning and enlightenment, expressed in his music and his words. As Terence Trent D’Arby, he became a huge star, with a #1 hit (“Wishing Well”) and endless adulation (his supermodel analogy certainly comes from first-hand experience). In the ‘00s, he took his new name, and with it, became a new person. Here’s what he told us in 2007: TTD had died. His psyche had been shot full of so many Volume 1 arrows that he could no longer hold his spirit. After intense pain I meditated for a new spirit, a new will, a new identity. 1. Pandora’s Plight (02:09) Sananda Maitreya is an opportunity for me, this spirit, to live with a new psyche and use it to continue my work, the “PANDORA’S PLIGHT” Is simply that HER POWER work I came to earth for. WILL ALWAYS BE FEARED and RESENTED INSTEAD OF PRAISED. She will have attached to her image all of That work continues with Pandora’s PlayHouse, a musical the things we fail to understand and accept, while being journey of 28 tracks across two volumes. It’s steeped in denied the fruits of her glory. -
![1990 by ARTIST ] [ No of Tunes = 985 ]](https://docslib.b-cdn.net/cover/3232/1990-by-artist-no-of-tunes-985-6523232.webp)
1990 by ARTIST ] [ No of Tunes = 985 ]
[ 1990 by ARTIST ] [ No of Tunes = 985 ] 4 THE CAUSE >> AIN'T NO SUNSHINE 4 THE CAUSE >> STAND BY ME {K} 4PM >> SUKIYAKI 702 >> WHERE'S MY GIRL AT 98 DEGREES >> I DO CHERISH YOU 98 DEGREES >> THE HARDEST THING A T B >> 9PM ( TILL I COME ) A TEENS >> MAMMA MIA {K} A+ >> ENJOY YOURSELF AARON CARTER >> CRUSH ON YOU AC DC >> BIG GUN AC DC >> MONEY TALKS AC DC >> THUNDERSTRUCK {K} ACE OF BASE >> ALL THAT SHE WANTS {K} ACE OF BASE >> THE SIGN ADAM SANDLER >> I WANT TO GROW OLD WITH YOU ADRIANO CELENTANO >> BASTA ADRIANO CELENTANO >> I RAGAZZI DEL JUKE BOX AEROSMITH >> AMAZING AEROSMITH >> CRAZY AEROSMITH >> CRYING AEROSMITH >> FALLING IN LOVE AEROSMITH >> I DON'T WANT TO MISS A THING {K} AEROSMITH >> LIVIN' ON THE EDGE AEROSMITH >> PINK ALAN JACKSON >> DON'T ROCK THE JUKEBOX ALAN JACKSON >> EVERYTHING I LOVE ALAN JACKSON >> GONE COUNTRY ALAN JACKSON >> GONE CRAZY ALAN JACKSON >> I'LL GO ON LOVING YOU ALAN JACKSON >> LITTLE BITTY ALAN JACKSON >> LITTLE MAN ALAN JACKSON >> RIGHT ON THE MONEY ALAN JACKSON >> SUMMERTIME BLUES ALAN JACKSON >> TALL TALL TREES ALAN JACKSON >> THERE GOES ALANIS MORISETTE >> HAND IN MY POCKET ALANIS MORISSETTE >> THANK U {K} ALBERTO CHELI >> MARILENA ALEESHA ROME >> ONE OF US HAS CHANGED ALEESHA ROME >> SEARCH MY HEAVEN ALEXIA >> UH LA LA LA ALICE DEEJAY >> BETTER OFF ALONE {K} ALL SAINTS >> BOOTY CALL ALL SAINTS >> I KNOW WHERE IT'S AT ALL SAINTS >> LADY MARMALADE ALL SAINTS >> NEVER EVER ALL- 4- ONE >> I SWEAR AMBER >> SEXUAL ANDREA BOCELLI >> CON TE PARTIRO ANGEL FABIANI >> VIVA L'ALLEGRIA ANGELI BLU >> LONTANI ANGELO -

Heartland Music Project
The Music of Heartland A complete list of the songs that appear on episodes of Heartland on CBC. Last Update: April 1, 2021 SEASON FOURTEEN 1410 - Staying the Course "Girl" by SYML 1409 - Find Me in the Dark "Already Home" by Michael Logen 1408 - Changing Gears "City of Blues" by Cree Rider Family Band "All That You Got" by Cree Rider Family Band "Call to Arms" by Evan Olson 1407 - Courage "The Way That I What to Be" by Cree Rider Family Band "The Times They Are A-Changin'" by Fort Nowhere 1406 - The New Normal "Second Thought" by Bill Anschell "Something Better Coming" by Aardwolves 1405 - Outsiders "Not Alone" by Aardwolves 1404 - Through the Smoke 1403 - Making Amends 1402 - The Last Goodbye "Ready For the Fall" by Six Corners "Quitting You" by Arkells 1401 - Keep Me In Your Heart "Forever More" by Crystal Plamondon "All We Have" by 100 Mile House SEASON THIRTEEN 1310 - The Passing of the Torch "Call to Arms" by Evan Olson "I'm Boring" by Jacob John "I'll Be There For You" by Philip Larue 1309 - Fight or Flight "The One I Need" by Amy Stroup "Another Lie" by Jacob John 1308 - Legacy "Long Wet Day" by Sunday Jones "Without" by Sunday Jones "Lean on Somebody" by Caution Cat "Frank, AB" by The Rural Alberta Advantage 1307 - The Art of Trust "Moment (acoustic)" by Roses & Revolutions 1306 - A Time To Remember "This Little Town" by Chloe Collins "There Goes My Heart" by Aplusa "Never Enough" by Jayme Davis 1305 - Fairytale "Get Found" by The Heart Of 1304 - The Eye of the Storm "Family Name" by Peter Bradley Adams "Child Be Still" by Joe -

Behind the Smile: Negotiating and Transforming the Tourism-Imposed Identity of Bahamian Women
BEHIND THE SMILE: NEGOTIATING AND TRANSFORMING THE TOURISM-IMPOSED IDENTITY OF BAHAMIAN WOMEN Dellareese M. Higgs A Dissertation Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY August 2008 Committee: Radhika Gajalla, Advisor Bonnibeth Beale Fonseca-Greber Graduate Faculty Representative Lara Lengel-Martin Kamala Kempadoo ii ABSTRACT Radhika Gajalla, Advisor This research seeks to describe the links between whiteness and tourism in the construction of ‘Othered’ identities. It adds to the challenge of theorizing identity as posed by Frantz Fanon and Stuart Hall, and presents sociopolitical and theoretical insights informed by the historical constructions of whiteness from the lived experiences of black Bahamian women’s struggles for agency. Throughout this dissertation, I use Frantz Fanon’s inquiry into black identity formation—that is, as a construct in opposition to whiteness—as a framework to examine the development of tourism and identity negotiations in the Bahamas. Fanon himself— colonized French, black, expatriate, and activist—knew all too well the pitfalls of being at the margins of many identities. Moreover, with the advent and development of tourism throughout the Bahamas, whiteness became the protracted mode by which Bahamian progress was assessed. The minority white elites in the Bahamas benefited financially from the tourist industry, building an economy and a country where rich wealthy whites are served by the majority black populace, hence the development of a ‘white tourist culture.’ I use the term ‘white tourist culture’ in this dissertation to describe how Bahamian national identity is constructed through our dependency on a tourist economy that has built its financial system on a myth of paradise, where white tourists are catered to, and black Bahamians serve, entertain and cultivate the exotic. -

C3939 Peter Tamony Collection
C3939 Peter Tamony Collection A-Z WORD LIST A Abdication A [combining forms] Abdulla Bulbul Amir A 1 *A Number One Abecedarium A 3 Aberastus A. A. +Alcoholics Anonymous Abie Aaah Abie's Irish Rose Aaargh Abilities A A Bloc Abilities Incorporated AAC. Abilitism A Age Ability A And R Man Ability [combining forms] Aardvark A B ing +A Aasis A Blast A. A. U. +Amateur Athletic Union Ablation Aaugh Able AB Able Baker Abab Able Baker Charlie Abacus Able Day Abadaba Able To Go *Go A.B.A.G. Abner Abalone Abnormal Abalone Baseball Abo +Abos Abandon Ship Aboard Abaria A Bomb +Atom Bomb Abasicky *Anbasicky A Bomb Blast Abate A Bombs Abatement A Bomb Test Abba Abominable Abba Dabba Abominable Showmen Abba Zaba Abominable Snowman Abbie Hoffman Abomunist Manifesto Abbo Aboo [combining forms] Abbondanza Abort Abbott and Costello +Whos On First Abortion Abbreviations +Acronyms Abortionist Abby Abortion Mill *Mill A B C Abos +Abo A B C D About ABCDisms About [combining forms] Ab Ced About Face Abcess *AB Abouts [combining forms] ABC Governments About Town ABCing Above All ABC Stone Above Board ABC War Above The Line +Line ABDA Abplanalp Ab Dabs Abracadabra Abraham Lincoln Brigade Absent Abrasive Absenteeism Abraxes Absent Minded Abrazo ABSIE Abri Absinth Abroad Absolutely, Mr. Gallagher Abscam Absolutely Positively Absolutes Accents Absolutism Accentuate Absolutist Accentuates Absolutist Absurdities *Ahab Accentuate the Positive Absorbine Junior Acceptance +Age of Acceptance Absotively Acceptance Ring Absquatulate Access Abstinyl +Antabus Access Fees Abstract