Medicaid and CHIP in the Territories
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Women and Medicaid in the District of Columbia (DC) (As of February 2010)
Women and Medicaid in the District of Columbia (DC) (As of February 2010) Medicaid, the national health insurance program for low-income people, plays a critical role in providing health coverage for women. Nationally, nearly 17 million nonelderly women— including 18 percent of those living in DC—are covered through Medicaid.1,2 In fact, women comprise the majority (60 percent) of DC’s adult Medicaid beneficiaries.3 Women are more likely than men to qualify for Medicaid because they tend to be poorer and are more likely to meet the program’s stringent eligibility criteria. Women are also more likely to hold low-wage or part-time jobs that do not offer employer-sponsored health benefits, so Medicaid may be their only possible source of coverage.4,5 Medicaid is jointly funded by the federal and state Eligibility Limits for Medicaid and governments and is administered by the states. State Coverage Programs in 1 Though states must comply with a host of federal the District of Columbia 2010 Medicaid requirements, they can exercise Women with dependent children: 207% of the flexibility with regards to certain program Federal Poverty Level (FPL)2 elements. There is considerable state variation, Women without dependent children: A more for instance, in who is able to get coverage limited benefit package is available to those through Medicaid, the income level needed to with incomes up to 211% of the FPL qualify, and the services that the program covers. Pregnant women: 300% of the FPL Disabled and aged women: 74% of the FPL Nearly one in five women in DC receives 6 Women who have breast and cervical cancer: health care coverage through Medicaid. -

California Policy Needs During and After COVID: Eligibility, Enrollment, and Retention
National Health Law Program December 23, 2020 California Policy Needs During and After COVID: Eligibility, Enrollment, and Retention Alicia Emanuel & Skyler Rosellini I. Introduction The COVID-19 public health emergency (PHE) has fundamentally altered how California’s Medi-Cal program is administered. At the start of the pandemic, the state worked swiftly to seek waivers and other flexibilities of federal Medicaid requirements and to implement these COVID-19 flexibilities, including significant changes intended to streamline Medi-Cal eligibility and enrollment. In order to preserve Medi-Cal coverage for low-income Californians once the pandemic ends, California’s Medicaid agency, the Department of Health Care Services (DHCS), needs to plan now for its end. This issue brief highlights various policies the state put in place during the pandemic that should be continued after the pandemic, as well as other policies it needs to put in place now to mitigate harm to the Medi-Cal population once the pandemic is over. A. Overview of Federal Guidance and the Moratorium on Negative Actions The Families First Coronavirus Response Act (FFCRA) increased the federal government’s share of Medicaid costs (also known as the federal medical assistance percentage, or FMAP) by 6.2 percent to help states manage increased enrollment and state budget shortfalls due to the COVID-19 PHE.1 The increase lasts through the end of the calendar year quarter in which the PHE ends. As of the date of this publication, the Secretary of Health & Humans Services has extended the existing PHE through January 20, 2021 and therefore, the FMAP increase 1 Families First Coronavirus Response Act [hereinafter FFCRA], Pub. -

District of Columbia Statehood and Voting Representation
Updated June 29, 2020 District of Columbia Statehood and Voting Representation On June 26, 2020, the U.S. House of Representatives have included full statehood or more limited methods of considered and passed the Washington, D.C. Admission providing DC residents the ability to vote in congressional Act, H.R. 51. This marked the first time in 27 years a elections. Some Members of Congress have opposed these District of Columbia (DC) statehood bill was considered on legislative efforts and recommended maintaining the status the floor of the House of Representatives, and the first time quo. Past legislative proposals have generally aligned with in the history of Congress a DC statehood bill was passed one of the following five options: by either the House or the Senate. 1. a constitutional amendment to give DC residents voting representation in This In Focus discusses the political status of DC, identifies Congress; concerns regarding DC representation, describes selected issues in the statehood process, and outlines some recent 2. retrocession of the District of Columbia DC statehood or voting representation bills. It does not to Maryland; provide legal or constitutional analysis on DC statehood or 3. semi-retrocession (i.e., allowing qualified voting representation. It does not address territorial DC residents to vote in Maryland in statehood issues. For information and analysis on these and federal elections for the Maryland other issues, please refer to the CRS products listed in the congressional delegation to the House and final section. Senate); 4. statehood for the District of Columbia; District of Columbia and When ratified in 1788, the U.S. -

Environmental Assessment for the Replacement of the Pier and Boat Ramp at the U.S
Draft Environmental Assessment for the Repairs and Replacement of the Boat Ramp and Pier at the US Border Patrol Air and Marine Facility, Ponce, Puerto Rico Environmental Assessment for the Replacement of the Pier and Boat Ramp at the U.S. Border Patrol & Air and Marine Facility, Ponce, Puerto Rico U.S. Customs and Border Protection February 2019 Draft Environmental Assessment for the Repairs and Replacement of the Boat Ramp and Pier at the US Border Patrol Air and Marine Facility, Ponce, Puerto Rico Environmental Assessment for the Replacement of the Pier and Boat Ramp at the U.S. Border Patrol & Air and Marine Facility, Ponce, Puerto Rico Environmental Assessment for the Replacement of the Pier and Boat Ramp at the U.S. Border Patrol & Air and Marine Facility, Ponce, Puerto Rico Lead Agency: U.S. Customs and Border Protection (CBP) Proposed Action: The demolition and removal of the temporary structure, removal of the original pier, construction of a new pier, and replacement of the boat ramp at 41 Bonaire Street in the municipality of Ponce, Puerto Rico. The replacement boat ramp would be constructed in the same location as the existing boat ramp, and the pier would be constructed south of the Ponce Marine Unit facility. For Further Information: Joseph Zidron Real Estate and Environmental Branch Chief Border Patrol & Air and Marine Program Management Office 24000 Avila Road, Suite 5020 Laguna Niguel, CA 92677 [email protected] Date: February 2019 Abstract: CBP proposes to remove the original concrete pier, demolish and remove the temporary structure, construct a new pier, replace the existing boat ramp, and continue operation and maintenance at its Ponce Marine Unit facility at 41 Bonaire Street, Ponce, Puerto Rico. -
Ruling America's Colonies: the Insular Cases Juan R
YALE LAW & POLICY REVIEW Ruling America's Colonies: The Insular Cases Juan R. Torruella* INTRODUCTION .................................................................. 58 I. THE HISTORICAL BACKDROP TO THE INSULAR CASES..................................-59 11. THE INSULAR CASES ARE DECIDED ......................................... 65 III. LIFE AFTER THE INSULAR CASES.......................... .................. 74 A. Colonialism 1o ......................................................... 74 B. The Grinding Stone Keeps Grinding........... ....... ......................... 74 C. The Jones Act of 1917, U.S. Citizenship, and President Taft ................. 75 D. The Jones Act of 1917, U.S. Citizenship, and ChiefJustice Taft ............ 77 E. Local Self-Government v. Colonial Status...........................79 IV. WHY THE UNITED STATES-PUERTO Rico RELATIONSHIP IS COLONIAL...... 81 A. The PoliticalManifestations of Puerto Rico's Colonial Relationship.......82 B. The Economic Manifestationsof Puerto Rico's ColonialRelationship.....82 C. The Cultural Manifestationsof Puerto Rico's Colonial Relationship.......89 V. THE COLONIAL STATUS OF PUERTO Rico Is UNAUTHORIZED BY THE CONSTITUTION AND CONTRAVENES THE LAW OF THE LAND AS MANIFESTED IN BINDING TREATIES ENTERED INTO BY THE UNITED STATES ............................................................. 92 CONCLUSION .................................................................... 94 * Judge, United States Court of Appeals for the First Circuit. The substance of this Article was presented in -
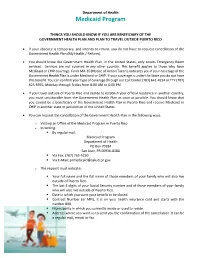
Medicaid Program
Department of Health Medicaid Program THINGS YOU SHOULD KNOW IF YOU ARE BENEFICIARY OF THE GOVERNMENT HEALTH PLAN AND PLAN TO TRAVEL OUTSIDE PUERTO RICO If your absence is temporary, and intends to return, you do not have to request cancellation of the Government Health Plan (My Health / Reform). You should know the Government Health Plan, in the United States, only covers Emergency Room services. Services are not covered in any other country. This benefit applies to those who have Medicaid or CHIP coverage. Form MA-10 (Notice of Action Taken), indicates you if your coverage of the Government Health Plan is under Medicaid or CHIP. If your coverage is under the State you do not have this benefit. You can confirm your type of coverage through our Call Center (787) 641-4224 or TTY (787) 625-6955, Monday through Friday from 8:00 AM to 6:00 PM. If you travel outside of Puerto Rico and decide to establish your official residence in another country, you must unsubscribe from the Government Health Plan as soon as possible. You should know that you cannot be a beneficiary of the Government Health Plan in Puerto Rico and receive Medicaid or CHIP in another state or jurisdiction of the United States. You can request the cancellation of the Government Health Plan in the following ways: o Visiting an Office of the Medicaid Program in Puerto Rico o In writing: . By regular mail: Medicaid Program Department of Health PO Box 70184 San Juan, PR 00936-8184 . Via Fax: (787) 763-5250 . Via E-Mail: [email protected] o The request must indicate: . -

Testimony Medicaid and CHIP in the U.S. Territories
Statement of Anne L. Schwartz, PhD Executive Director Medicaid and CHIP Payment and Access Commission Before the Health Subcommittee Committee on Energy and Commerce U.S. House of Representatives March 17, 2021 i Summary Medicaid and CHIP play a vital role in providing access to health services for low-income individuals in the five U.S. territories: American Samoa, the Commonwealth of the Northern Mariana Islands, Guam, Puerto Rico, and the U.S. Virgin Islands. The territories face similar issues to those in the states: populations with significant health care needs, an insufficient number of providers, and constraints on local resources. With some exceptions, they operate under similar federal rules and are subject to oversight by the Centers for Medicare & Medicaid Services. However, the financing structure for Medicaid in the territories differs from state programs in two key respects. First, territorial Medicaid programs are constrained by an annual ceiling on federal financial participation, referred to as the Section 1108 cap or allotment (§1108(g) of the Social Security Act). Territories receive a set amount of federal funding each year regardless of changes in enrollment and use of services. In comparison, states receive federal matching funds for each state dollar spent with no cap. Second, the federal medical assistance percentage (FMAP) is statutorily set at 55 percent rather than being based on per capita income. If it were set using the state formula, the matching rate for all five territories would be significantly higher, and for most, would likely be the maximum of 83 percent. These two policies have resulted in chronic underfunding of Medicaid in the territories, requiring Congress to step in at multiple points to provide additional resources. -

Excavations at Maruca, a Preceramic Site in Southern Puerto Rico
EXCAVATIONS AT MARUCA, A PRECERAMIC SITE IN SOUTHERN PUERTO RICO Miguel Rodríguez ABSTRACT A recent set of radiocarbon dated shows that the Maruca site, a preceramic site located in the southern coastal plains of Puerto Rico, was inhabited between 5,000 and 3,000 B.P. bearing the earliest dates for human habitation in Puerto Rico. Also the discovery in the site of possible postmolds, lithic and shell workshop areas and at least eleven human burials strongly indicate the possibility of a permanent habitation site. RESUME Recientes fechados indican una antigüedad entre 5,000 a 3000 años antes de del presente para Maruca, una comunidad Arcaica en la costa sur de Puerto Rico. Estos son al momento los fechados más antiguos para la vida humana en Puerto Rico. El descubrimiento de socos, de posible talleres líticos, de áreas procesamiento de moluscos y por lo menos once (11) enterramientos humanos sugieren la posibilidad de que Maruca sea un lugar habitation con cierta permanence. KEY WORDS: Human Remains, Marjuca Site, Preceramic Workshop. INTRODUCTION During the 1980s archaeological research in Puerto Rico focused on long term multidisciplinary projects in early ceramic sites such as Sorcé/La Hueca, Maisabel and Punta Candelera. This research significantly expanded our knowledge of the life ways and adaptive strategies of Cedrosan and Huecan Saladoid cultures. Although the interest in these early ceramic cultures has not declined, it seems that during the 1990s, archaeological research began to develop other areas of interest. With the discovery of new preceramic sites of the Archaic age found during construction projects, the attention of specialists has again been focused on the first in habitants of Puerto Rico. -

Puerto Rico, Colonialism In
University at Albany, State University of New York Scholars Archive Latin American, Caribbean, and U.S. Latino Latin American, Caribbean, and U.S. Latino Studies Faculty Scholarship Studies 2005 Puerto Rico, Colonialism In Pedro Caban University at Albany, State Univeristy of New York, [email protected] Follow this and additional works at: https://scholarsarchive.library.albany.edu/lacs_fac_scholar Part of the Latin American Studies Commons Recommended Citation Caban, Pedro, "Puerto Rico, Colonialism In" (2005). Latin American, Caribbean, and U.S. Latino Studies Faculty Scholarship. 19. https://scholarsarchive.library.albany.edu/lacs_fac_scholar/19 This Encyclopedia Entry is brought to you for free and open access by the Latin American, Caribbean, and U.S. Latino Studies at Scholars Archive. It has been accepted for inclusion in Latin American, Caribbean, and U.S. Latino Studies Faculty Scholarship by an authorized administrator of Scholars Archive. For more information, please contact [email protected]. 516 PUERTO RICO, COLONIALISM IN PUERTO RICO, COLONIALISM IN. Puerto Rico They automatically became subjects of the United States has been a colonial possession of the United States since without any constitutionally protected rights. Despite the 1898. What makes Puerto Rico a colony? The simple an humiliation of being denied any involvement in fateful swer is that its people lack sovereignty and are denied the decisions in Paris, most Puerto Ricans welcomed U.S. fundamental right to freely govern themselves. The U.S. sovereignty, believing that under the presumed enlight Congress exercises unrestricted and unilateral powers over ened tutelage of the United States their long history of Puerto Rico, although the residents of Puerto Rico do not colonial rule would soon come to an end. -

Kentucky Medicaid Eligibility Determinations for the Adult Expansion Population
Department of Health and Human Services Centers for Medicare & Medicaid Services Center for Program Integrity Kentucky Medicaid Eligibility Determinations for the Adult Expansion Population Review Period: October 2017 through March 2018 Eligibility Review Final Report September 2020 Table of Contents Executive Summary ........................................................................................................................ 3 Kentucky Correctly Determined Medicaid Eligibility for 95 Percent of the Adult Expansion Population.................................................................................................................................... 3 Results of the Review .................................................................................................................. 4 Eligibility Review: Kentucky Medicaid Eligibility Determinations for the Adult Expansion Population ....................................................................................................................................... 5 Background ................................................................................................................................. 5 Medicaid Coverage for Newly Eligible Beneficiaries under the Affordable Care Act (ACA) ................................................................................................................................................. 5 Medicaid Adult Expansion Population in Kentucky .............................................................. 7 Kentucky’s Medicaid -

O Le Fogavaʻa E Tasi: Claiming Indigeneity Through Western Choral Practice in the Sāmoan Church
O Le Fogavaʻa e Tasi: Claiming Indigeneity through Western Choral practice in the Sāmoan Church Jace Saplan University of Hawai‘i, Mānoa Abstract Indigenous performance of Native Sāmoa has been constructed through colonized and decolonized systems since the arrival of western missionaries. Today, the western choral tradition is considered a cultural practice of Sāmoan Indigeniety that exists through intersections of Indigenous protocol and eurocentric performance practice. This paper will explore these intersections through an analysis of Native Sāmoan understandings of gender, Indigenous understandings and prioritizations of western vocal pedagogy, and the Indigenization of western choral culture. Introduction Communal singing plays a significant role in Sāmoan society. Much like in the greater sphere of Polynesia, contemporary Sāmoan communities are codified and bound together through song. In Sāmoa, sa (evening devotions), Sunday church services, and inter-village festivals add to the vibrant propagation of communal music making. These practices exemplify the Sāmoan values of aiga (family) and lotu (church). Thus, the communal nature of these activities contributes to the cultural value of community (Anae, 1998). European missionaries introduced hymn singing and Christian theology in the 1800s; this is acknowledged as a significant influence on the paralleled values of Indigenous thought, as both facets illustrate the importance of community (McLean, 1986). Today, the church continues to amplify the cultural importance of community, and singing remains an important activity to propagate these values. In Sāmoa, singing is a universal activity. The vast majority of Native Sāmoans grow up singing in the church choir, and many Indigenous schools require students to participate in the school choir. -

Kentucky Medicaid Model Enrollee Handbook
Kentucky Department for Medicaid Services Medicaid Enrollee Handbook KENTUCKY MEDICAID MODEL ENROLLEE HANDBOOK Plan Year 2021 1022559KYMENABS 12/20 Approved December 7, 2020 Kentucky Department for Medicaid Services Medicaid Enrollee Handbook You can get this handbook and other plan information in large print for free. To get materials in large print, call Member Services at 855-690-7784 (TTY 711). If English is not your first language (or if you are reading this on behalf of someone who doesn’t read English), we can help. Call 855-690-7784 (TTY 711). You can ask us for the information in this handbook in your language. We have access to interpreter services and can help answer your questions in your language. ATENCIÓN: Si habla español, tiene a su disposición servicios gratuitos de asistencia lingüística. Llame al 502-564-7770 (TTY: 502-573-2604). 注意:如果您使用繁體中文,您可以免費獲得語言援助服務。請致電 502-564-7770 (TTY:1502-573-2604)。 ACHTUNG: Wenn Sie Deutsch sprechen, stehen Ihnen kostenlos sprachliche Hilfsdienstleistungen zur Verfügung. Rufnummer: 502-564-7770 (TTY: 502-573-2604). CHÚ Ý: Nếu bạn nói Tiếng Việt, có các dịch vụ hỗ trợ ngôn ngữ miễn phí dành cho bạn. Gọi số 502-564-7770 (TTY: 502-573-2604). 502-564-ᒃᏸፅᑰᎏቨ ͘ᒇቲዱᑿᑢቲᗷᑃᑢፅᏕቨᓗኤᓀᗫᖔᎼᑩᑢቨᒻጤᎳቲ፭ᑿᑢቨቺቲᑻጤዡᒇቱᏕᅩᓀᎼᑩᑢቨፅᐛቨቻጤዲኤኹᒙᐛቨቧ ͗ᓀᎠᓗዲᑩᑻ (502-573-2604͗ᒃᜓᘘᑢቨᓆᒃᎏᑢቨᏩቲᒯᒃᏸጳͿ 7770 OBAVJEŠTENJE: Ako govorite srpsko-hrvatski, usluge jezičke pomoći dostupne su vam besplatno. Nazovite 502-564-7770 (TTY- Telefon za osobe sa oštećenim govorom ili sluhom: 502-573-2604). 注意事項:日本語を話される場合、無料の言語支援をご利用いただけます。502-564- 7770(TTY: 502-573-2604)まで、お電話にてご連絡ください。 ATTENTION : Si vous parlez français, des services d'aide linguistique vous sont proposés gratuitement.