The Differential Diagnosis of the Breathless Patient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Musculoskeletal Diagnosis Utilizing History and Physical Examination: Focus on Spine
NYU Long Island School of Medicine MUSCULOSKELETAL DIAGNOSIS UTILIZING HISTORY AND PHYSICAL EXAMINATION: FOCUS ON SPINE Ralph K. Della Ratta, MD, FACP Kevin J. Curley, MD, FACP Division of General Internal Medicine, NYU Winthrop Hospital NYU Long Island School of Medicine, SUNY Stony Brook School of Medicine Board Certified in IM and Primary Care Sports Medicine Learning Objectives 1. Identify components of the focused history and physical examination that will guide musculoskeletal diagnosis 2. Utilize musculoskeletal examination provocative maneuvers to aide differential diagnosis 3. Review the evidence base (likelihood ratios etc.) that is known about musculoskeletal physical examination 2 NYU Long Island School of Medicine * ¾ of medical diagnoses are still made on history and exam despite technological Musculoskeletal Physical Exam advances of modern medicine • Physical examination is key to musculoskeletal diagnosis • Unlike many other organ systems, the diagnostic standard for many musculoskeletal disorders is the exam finding (e.g. diagnosis of epicondylitis, see below) • “You may think you have not seen it, but it has seen you!” Lateral Epicondylitis confirmed on exam by reproducing pain at lateral epicondyle with resisted dorsiflexion at wrist **not diagnosed with imaging** 3 NYU Long Island School of Medicine Musculoskeletal Physical Exam 1. Inspection – symmetry, swelling, redness, deformity 2. Palpation – warmth, tenderness, crepitus, swelling 3. Range of motion *most sensitive for joint disease Bates Pocket Guide to Physical -

Clinical Features of Acute Epiglottitis in Adults in the Emergency Department
대한응급의학회지 제 27 권 제 1 호 � 원저� Volume 27, Number 1, February, 2016 Eye, Ear, Nose & Oral Clinical Features of Acute Epiglottitis in Adults in the Emergency Department Department of Emergency Medicine, Seoul National University College of Medicine, Seoul, Dongguk University Ilsan Hospital, Goyang, Gyeonggi-do1, Korea Kyoung Min You, M.D., Woon Yong Kwon, M.D., Gil Joon Suh, M.D., Kyung Su Kim, M.D., Jae Seong Kim, M.D.1, Min Ji Park, M.D. Purpose: Acute epiglottitis is a potentially fatal condition Key Words: Epiglottitis, Emergency medical services, Fever, that can result in airway obstruction. The aim of this study is Intratracheal Intubation to examine the clinical features of adult patients who visited the emergency department (ED) with acute epiglottitis. Methods: This retrospective observational study was con- Article Summary ducted at a single tertiary hospital ED from November 2005 What is already known in the previous study to October 2015. We searched our electronic medical While the incidence of acute epiglottitis in children has records (EMR) system for a diagnosis of “acute epiglottitis” shown a marked decrease as a result of vaccination for and selected those patients who visited the ED. Haemophilus influenzae type b, the incidence of acute Results: A total of 28 patients were included. There was no epiglottitis in adults has increased. However, in Korea, few pediatric case with acute epiglottitis during the study period. studies concerning adult patients with acute epiglottitis The mean age of the patients was 58.0±14.8 years. The who present to the emergency department (ED) have been peak incidences were in the sixth (n=7, 25.0%) and eighth reported. -

EPA Quick Reference Guide
EPA Quick Reference Guide EPAs 1 & 2 – Professionalism Unacceptable • Unreliable • Dishonest • Avoids responsibility • Commitment uncertain • Dresses inappropriately • Unexplained absences • Verbal and non-verbal disrespect towards preceptor • Does not recognize own limitations and the need to seek assistance • Unable to comprehend the point of view and emotional state of other people • Judgmental of others • Fails to recognize and respect cross-cultural and gender differences Minimally Competent • Sometimes late • Not consistently able to complete assignments or tasks • Not consistently considerate of the feelings and emotional needs of others • Sometimes judgmental Competent • Punctual • Dependable • Accepts responsibilities • Demonstrates a willingness to accept feedback regarding necessary change(s) • Appropriately shows concern for others’ feelings and interacts accordingly • Recognizes and respects cross-cultural and gender differences Office of Medical Education 306 Liberty View Lane, Lynchburg, Va. 24502 [email protected] EPAs 3 & 4 – Data Gathering / Interviewing & Physical Examination Skills Unacceptable • Inefficient, disorganized • Weak prioritization skills • Misses major findings • Fails to appreciate physical findings and pertinent information • History and/or physical exam incomplete or inaccurate • Insufficient attention to psychosocial issues • Needs to work on establishing rapport with patients • Needs to work on awareness of appropriate boundaries with patients • Needs to improve demonstration of compassion • -
Clinical Reasoning - the Process of Thinking and Decision Making, Consciously & Unconsciously Guide Practice Actions
Diagnostic Reasoning “DR” Toolbox for Hospitalist Faculty Heather Hofmann, MD Department of Medicine 2017-18 2 Goal Increase faculty familiarity with diagnostic reasoning principles and tools so as to improve its teaching. Three Parts: I: Introduction to Diagnostic Reasoning II: DR Toolbox III: Structured Reflection Exercise (SRE) 4 Part I: Introduction to Diagnostic Reasoning Learning Objectives - Understand the “what” and “why” of Diagnostic Reasoning - Recognize dual-process theory’s role in “how” we reason 6 What is Diagnostic Reasoning? - Clinical reasoning - The process of thinking and decision making, consciously & unconsciously guide practice actions 25yo female G1P0, 2m gestation returns from Rio. - Diagnostic reasoning: - The process of collecting & analyzing information establish a diagnosis chest pain STEMI in proximal LAD abdominal pain acute appendicitis 7 Why teach diagnostic reasoning? - Incorrect diagnoses are often at the root of medical errors - DR is a means to apply basic science to clinical problems - Central to being a physician 8 Patient’s perspective What’s wrong with me? Is it bad? What can we do about it? 9 Why now? Never too early for practice 10 From Novice to Expert 11 How do we reason? Information processing theory 12 How do we reason? Information processing theory: Dual process theory. Analytical Non-analytical Conscious Unconscious Type/System 2 Type/System 1 Slow Fast Effortful Automatic Deliberative Involuntary Logical Emotional Requires attention, Executes skilled self-control, time. response and -

Table of Contents
viii Contents Chapter 1. Taking the Certification Examination . 1 General Suggestions for Preparing for the Exam About the Certification Exams Chapter 2. Developmental and Behavioral Sciences . 11 Mary Jo Gilmer, PhD, MBA, RN-BC, FAAN, and Paula Chiplis, PhD, RN, CPNP Psychosocial, Cognitive, and Ethical-Moral Development Behavior Modification Physical Development: Normal Growth Expectations and Developmental Milestones Family Concepts and Issues Family-Centered Care Cultural and Spiritual Diversity Chapter 3. Communication . 23 Mary Jo Gilmer, PhD, MBA, RN-BC, FAAN, and Karen Corlett, MSN, RN-BC, CPNP-AC/PC, PNP-BC Culturally Sensitive Communication Components of Therapeutic Communication Communication Barriers Modes of Communication Patient Confidentiality Written Communication in Nursing Practice Professional Communication Advocacy Chapter 4. The Nursing Process . 33 Clara J. Richardson, MSN, RN–BC Nursing Assessment Nursing Diagnosis and Treatment Chapter 5. Basic and Applied Sciences . 49 Mary Jo Gilmer, PhD, MBA, RN-BC, FAAN, and Paula Chiplis, PhD, RN, CPNP Trauma and Diseases Processes Common Genetic Disorders Common Childhood Diseases Traction Pharmacology Nutrition Chemistry Clinical Signs Associated With Isotonic Dehydration in Infants ix Chapter 6. Educational Principles and Strategies . 69 Mary Jo Gilmer, PhD, MBA, RN-BC, FAAN, and Karen Corlett, MSN, RN-BC, CPNP-AC/PC, PNP-BC Patient Education Chapter 7. Life Situations and Adaptive and Maladaptive Responses . 75 Mary Jo Gilmer, PhD, MBA, RN-BC, FAAN, and Karen Corlett, MSN, RN-BC, CPNP-AC/PC, PNP-BC Palliative Care End-of-Life Care Response to Crisis Chapter 8. Sensory Disorders . 87 Clara J. Richardson, MSN, RN–BC Developmental Characteristics of the Pediatric Sensory System Hearing Disorders Vision Disorders Conjunctivitis Otitis Media and Otitis Externa Retinoblastoma Trauma to the Eye Chapter 9. -

Risk of Acute Epiglottitis in Patients with Preexisting Diabetes Mellitus: a Population- Based Case–Control Study
RESEARCH ARTICLE Risk of acute epiglottitis in patients with preexisting diabetes mellitus: A population- based case±control study Yao-Te Tsai1,2, Ethan I. Huang1,2, Geng-He Chang1,2, Ming-Shao Tsai1,2, Cheng- Ming Hsu1,2, Yao-Hsu Yang3,4,5, Meng-Hung Lin6, Chia-Yen Liu6, Hsueh-Yu Li7* 1 Department of Otorhinolaryngology-Head and Neck Surgery, Chang Gung Memorial Hospital, Chiayi, Taiwan, 2 College of Medicine, Chang Gung University, Taoyuan, Taiwan, 3 Department of Traditional Chinese Medicine, Chang Gung Memorial Hospital, Chiayi, Taiwan, 4 Institute of Occupational Medicine and a1111111111 Industrial Hygiene, National Taiwan University College of Public Health, Taipei, Taiwan, 5 School of a1111111111 Traditional Chinese Medicine, College of Medicine, Chang Gung University, Taoyuan, Taiwan, 6 Health a1111111111 Information and Epidemiology Laboratory, Chang Gung Memorial Hospital, Chiayi, Taiwan, 7 Department of a1111111111 Otolaryngology±Head and Neck Surgery, Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan a1111111111 * [email protected] Abstract OPEN ACCESS Citation: Tsai Y-T, Huang EI, Chang G-H, Tsai M-S, Hsu C-M, Yang Y-H, et al. (2018) Risk of acute Objective epiglottitis in patients with preexisting diabetes Studies have revealed that 3.5%±26.6% of patients with epiglottitis have comorbid diabetes mellitus: A population-based case±control study. PLoS ONE 13(6): e0199036. https://doi.org/ mellitus (DM). However, whether preexisting DM is a risk factor for acute epiglottitis remains 10.1371/journal.pone.0199036 unclear. In this study, our aim was to explore the relationship between preexisting DM and Editor: Yu Ru Kou, National Yang-Ming University, acute epiglottitis in different age and sex groups by using population-based data in Taiwan. -
Problems in Family Practice
problems in Family Practice Coughing in Childhood Hyman Sh ran d , M D Cambridge, M assachusetts Coughing in childhood is a common complaint involving a wide spectrum of underlying causes which require a thorough and rational approach by the physician. Most children who cough have relatively simple self-limiting viral infections, but some may have serious disease. A dry environment, allergic factors, cystic fibrosis, and other major illnesses must always be excluded. A simple clinical approach, and the sensible use of appropriate investigations, is most likely to succeed in finding the cause, which can allow precise management. The cough reflex as part of the defense mechanism of the respiratory tract is initiated by mucosal changes, secretions or foreign material in the pharynx, larynx, tracheobronchial Table 1. Persistent Cough — Causes in Childhood* tree, pleura, or ear. Acting as the “watchdog of the lungs,” the “good” cough prevents harmful agents from Common Uncommon Rare entering the respiratory tract; it also helps bring up irritant material from Environmental Overheating with low humidity the airway. The “bad” cough, on the Allergens other hand, serves no useful purpose Pollution Tobacco smoke and, if persistent, causes fatigue, keeps Upper Respiratory Tract the child (and parents) awake, inter Recurrent viral URI Pertussis Laryngeal stridor feres with feeding, and induces vomit Rhinitis, Pharyngitis Echo 12 Vocal cord palsy Allergic rhinitis Nasal polyp Vascular ring ing. It is best suppressed. Coughs and Prolonged use of nose drops Wax in ear colds constitute almost three quarters Sinusitis of all illness in young children. The Lower Respiratory Tract Asthma Cystic fibrosis Rt. -
Diagnosis and Management of Chlamydia: a Guide for Gps
■ PRESCRIBING IN PRACTICE Diagnosis and management of chlamydia: a guide for GPs ELEANOR DRAEGER SPL Chlamydia is a common sexually- transmitted infection caused by Chlamydia trachomatis bacteria. This article discusses its diagnosis and treatment, and considers the GP’s role in management. hlamydia is the most common sexually-transmitted infection C(STI) in the UK, with 203,116 new diagnoses in England in 2017, of which 126,828 (62%) were in young people aged 15–24 years.1 Chlamydia is transmitted primarily through penetrative sex and infects the urethra and endocervix. It can also infect the throat and the rectum, and in some cases the conjunctiva. It is very infectious, with a concordance of up to 75% between sexual partners. There are many risk factors for chlamydia infection, including being under the age of 25 years, having a new sexual partner and inconsistent use of condoms. If a woman contracts chlamydia during pregnancy it can be transmitted to the baby at delivery, causing conjunctivitis or pneumonia. Classification of chlamydia infections There are three species of chlamydia bacteria that can cause disease in humans: • Chlamydia psittaci – the natural host is birds, especially par- rots, but it can be transmitted to humans, causing psittacosis • Chlamydia pneumoniae – causes respiratory disease in humans • Chlamydia trachomatis – several different serovars can cause disease (including STIs) in humans, as detailed in Figure 1. Symptoms The majority of genital chlamydia infections are asymptomatic, but they can cause significant symptoms. In women, chlamydia can cause vaginal discharge, dysuria, abdominal and pelvic pain, post-coital and intermenstrual bleeding, and deep dys- pareunia. -

The Contribution of the Medical History for the Diagnosis of Simulated Cases by Medical Students
International Journal of Medical Education. 2012;3:78-82 ISSN: 2042-6372 DOI: 10.5116/ijme.4f8a.e48c The contribution of the medical history for the diagnosis of simulated cases by medical students Tomoko Tsukamoto, Yoshiyuki Ohira, Kazutaka Noda, Toshihiko Takada, Masatomi Ikusaka Department of General Medicine, Chiba University Hospital, Japan Correspondence: Tomoko Tsukamoto, Department of General Medicine, Chiba University Hospital, 1-8-1 Inohana, Chuo-ku, Chiba city, Chiba, 260-8677 Japan. Email: [email protected] Accepted: April 15, 2012 Abstract Objectives: The case history is an important part of diag- rates were compared using analysis of the χ2-test. nostic reasoning. The patient management problem method Results: Sixty students (63.8%) made a correct diagnosis, has been used in various studies, but may not reflect the which was based on the history in 43 students (71.7%), actual reasoning process because a list of choices is given to physical findings in 11 students (18.3%), and laboratory the subjects in advance. This study investigated the contri- data in 6 students (10.0%). Compared with students who bution of the history to making the correct diagnosis by considered the correct diagnosis in their differential diagno- using clinical case simulation, in which students obtained sis after taking a history, students who failed to do so were clinical information by themselves. 5.0 times (95%CI = 2.5-9.8) more likely to make a final Methods: A prospective study was conducted. Ninety-four misdiagnosis (χ2(1) = 30.73; p<0.001). fifth-year medical students from Chiba University who Conclusions: History taking is especially important for underwent supervised clinical clerkships in 2009 were making a correct diagnosis when students perform clinical surveyed. -

Peripheral Arterial Disease | Piedmont Healthcare
Peripheral Arterial Disease CLAUDICATION TO LIMB THREATENING ISCHEMIA THE HOW AND WHEN TO EVALUATE AND TREAT Brian M Freeman MD FACS Nothing to Disclose PAD: Peripheral Arterial Disease Obstruction of any “peripheral artery” Causes – Atherosclerosis – Emboli – Extrinsic compression – Vasculitis PAD Effects more than 15 million Americans Majority of patients are asymptomatic African Americans and Hispanics are at risk Diabetics with PAD are at significant risk for amputations (Neuropathy + PAD) PAD Risk Factors PAD: PREVALENCE vs AGE PAD: More Prevalent and More Deadly Than Many Leading Diseases Disease Prevalence (Millions) Five-Year Mortality Rate 5 50% 17.0 4 40% 39% 30% 3 30% 28% 12.6 12.0 8.9 21% 2 4.8 20% 5.0 14% 4.0 1 10% 0 0% Diabetes Coronary PAD Cancer CHF Stroke Alzheimers Colorectal PAD Stroke CAD Breast Heart Cancer Cancer Disease Source: American Cancer Society, American Heart Association, Alzheimers Disease Education/Referral Center, American Diabetes Association, SAGE Group PAD: LONG-TERM MORTALITY Atherosclerosis is a Systemic Disease Lesion Location Consequence Carotid, cerebral Stroke Aorta, arch Aneurysm Coronary artery MI Renal artery HTN, CRF Mesenteric Bowel infarct Iliac artery Impotence Femoral artery Claudication Tibial artery Limb loss PAD There is a 5 fold increase in the relative risk of a Cardiovascular ischemic event Total Mortality is increased 2-3 X Visual Cues to PAD and Arterial Insufficiency Cool, dry, atrophic skin on legs Thickened or deformed nails-dystrophic Hair loss or uneven distribution on legs -

The Oral Presentation Nersi Nikakhtar, M.D
Guidelines for the Oral Presentation Nersi Nikakhtar, M.D. University of Minnesota Medical School !1 Table of Contents The Oral Presentation: An Introduction ..................................3 Why Worry About the Oral Presentation? ...............................4 Presenting the New Patient .....................................................5 The Opening Statement ......................................................5 History of Present Illness ....................................................5 Past Medical History ...........................................................6 Medications/Allergies ..........................................................7 Social and Family History ...................................................7 Review of Systems ..............................................................7 Vitals .....................................................................................8 Physical Exam .....................................................................8 Labs and Studies .................................................................8 Summary Statement ............................................................8 Assessment and Plan ..........................................................9 The Follow Up (or Daily) Presentation: What's Different? ...................................................................11 The Outpatient (Known Patient) Presentation: What's Different? ...................................................................12 !2 The Oral Presentation: An Introduction The -
Neurology History and Physical Guidelines
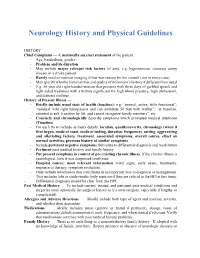
Neurology History and Physical Guidelines HISTORY Chief Complaint — A maximally succinct statement of the patient: - Age, handedness, gender - Problem and its duration - May include major relevant risk factors (if any), e.g. hypertension, coronary artery disease in a stroke patient. - Rarely need to mention imaging if that was reason for the consult (not in every case) - May specify who the historian was and quality of informant’s history if different from usual - E.g: 56 year old right-handed woman that presents with three days of garbled speech and right sided weakness with a history significant for high blood pressure, high cholesterol, and diabetes mellitus History of Present Illness — - Briefly include usual state of health (baseline): e.g: “normal, active, fully functional”; “residual mild right hemiparesis and can ambulate 50 feet with walker”; “at baseline, oriented to self, transfers by lift, and cannot recognize family members”, etc. - Concisely and chronologically describe symptoms which prompted medical attentions (Timeline) - For each try to include as many details: location, quality/severity, chronology (when it first began, mode of onset, mode of ending, duration, frequency), setting, aggravating and alleviating factors, treatment, associated symptoms, overall course, effect on normal activities, previous history of similar symptoms - Include pertinent negative symptoms that relate to differential diagnosis and localization - Pertinent past medical history and family history - Put present symptoms in context of pre-existing chronic illness. If the chronic illness is neurological, how it was diagnosed/confirmed - Hospital course: most relevant information (vital signs, early exam, treatments, response to therapy, symptom evolution) - Only include information that contributes in an important way to diagnosis or management.