Hereditary Ataxias: Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Rehabilitating Individuals with Spinocerebellar Ataxia: Experiences from Impairment-Based Rehabilitation Through Multidisciplinary Care Approach
Neurology Asia 2020; 25(1) : 75 – 80 Rehabilitating individuals with spinocerebellar ataxia: Experiences from impairment-based rehabilitation through multidisciplinary care approach 1,2Fatimah Ahmedy MBBCh MRehabMed, 1Yuen Woei Neoh MBBS, MRehabMed, 1Lydia Abdul Latiff MBBS MRehabMed 1Department of Rehabilitation Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur; 2Department of Surgery, Faculty of Medicine & Health Sciences, Universiti Malaysia Sabah, Kota Kinabalu, Sabah, Malaysia Abstract Spinocerebellar ataxia (SCA) is a rare neurodegenerative disease with progressive course and poor expected outcomes. Therefore, rehabilitation remains the principal form of management especially in advanced disease. Impairment-based rehabilitation through multidisciplinary care approach has proven benefits for functional improvement in individuals with advancing SCA. This concept is based on comprehensive assessments of individualised impairments and functional limitations while exploring contributing environmental and personal factors affecting the person as a whole. From this assessment, individualised rehabilitation goals can be formulated through a multidisciplinary care approach. Neurologists, rehabilitation physicians, physiotherapists, occupational therapists and speech and language pathologists are key individuals involved in the multidisciplinary care for individuals with SCA rehabilitation. Two cases of individuals at different stages of SCA are presented to highlight the rehabilitation approach in providing focused interventions -

Spinocerebellar Ataxia Genetic Testing
Lab Management Guidelines V1.0.2020 Spinocerebellar Ataxia Genetic Testing MOL.TS.311.A v1.0.2020 Introduction Spinocerebellar ataxia (SCA) genetic testing is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline ATXN1 gene analysis, evaluation to detect 81178 abnormal (eg,expanded) allele ATXN2 gene analysis, evaluation to detect 81179 abnormal (eg,expanded) allele ATXN3 gene analysis, evaluation to detect 81180 abnormal (eg,expanded) allele ATXN7 gene analysis, evaluation to detect 81181 abnormal (eg,expanded) allele ATXN8 gene analysis, evaluation to detect 81182 abnormal (eg, expanded) alleles ATXN10 gene analysis, evaluation to 81183 detect abnormal (eg, expanded) alleles CACNA1A gene analysis; evaluation to 81184 detect abnormal (eg, expanded) alleles CACNA1A gene analysis; full gene 81185 sequence CACNA1A gene analysis; known familial 81186 variant PPP2R2B gene analysis, evaluation to 81343 detect abnormal (eg, expanded) alleles TBP gene analysis, evaluation to detect 81344 abnormal (eg, expanded) alleles Unlisted molecular pathology procedure 81479 © 2020 eviCore healthcare. All Rights Reserved. 1 of 15 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2020 What is spinocerebellar ataxia Definition Spinocerebrallar ataxias (SCA) are a group of autosomal dominant ataxias that have a range of phenotypes. There are various subtypes of SCA, which are denoted by numbers (e.g. SCA1, SCA3, etc.) Incidence and Prevalence The prevalence of autosomal dominant cerebellar ataxias, as a whole, is 1-5:100,000.1 SCA3 is the most common autosomal dominant form of ataxia. -

Friedreich Ataxia Mouse Models with Progressive Cerebellar and Sensory Ataxia Reveal Autophagic Neurodegeneration in Dorsal Root Ganglia
The Journal of Neuroscience, February 25, 2004 • 24(8):1987–1995 • 1987 Neurobiology of Disease Friedreich Ataxia Mouse Models with Progressive Cerebellar and Sensory Ataxia Reveal Autophagic Neurodegeneration in Dorsal Root Ganglia Delphine Simon,1 Herve´ Seznec,1 Anne Gansmuller,1 Nade`ge Carelle,1 Philipp Weber,1 Daniel Metzger,1 Pierre Rustin,2 Michel Koenig,1 and He´le`ne Puccio1 1Institut de Ge´ne´tique et de Biologie Mole´culaire et Cellulaire, Centre National de la Recherche Scientifique/Institut National de la Sante´ et de la Recherche Me´dicale (INSERM)/Universite´ Louis Pasteur, 67404 Illkirch cedex, CU de Strasbourg, France, and 2Unite´ de Recherches sur les Handicaps Ge´ne´tiques de l’Enfant, INSERM U393, Hoˆpital Necker-Enfants Malades, 75015 Paris, France Friedreich ataxia (FRDA), the most common recessive ataxia, is characterized by degeneration of the large sensory neurons of the spinal cord and cardiomyopathy. It is caused by severely reduced levels of frataxin, a mitochondrial protein involved in iron–sulfur cluster (ISC) biosynthesis. Through a spatiotemporally controlled conditional gene-targeting approach, we have generated two mouse models for FRDA that specifically develop progressive mixed cerebellar and sensory ataxia, the most prominent neurological features of FRDA. Histological studies showed both spinal cord and dorsal root ganglia (DRG) anomalies with absence of motor neuropathy, a hallmark of the human disease. In addition, one line revealed a cerebellar granule cell loss, whereas both lines had Purkinje cell arborization defects. These lines represent the first FRDA models with a slowly progressive neurological degeneration. We identified an autophagic process as the causative pathological mechanism in the DRG, leading to removal of mitochondrial debris and apparition of lipofuscin deposits. -

Treatment of Autonomic Dysreflexia for Adults & Adolescents with Spinal
Treatment of Autonomic Dysreflexia for Adults & Adolescents with Spinal Cord Injuries Authors: Dr James Middleton, Director, State Spinal Cord Injury Service, NSW Agency for Clinical Innovation. Dr Kumaran Ramakrishnan, Honorary Fellow, Rehabilitation Studies Unit, Sydney Medical School Northern, The University of Sydney, and Consultant Rehabilitation Physician & Senior Lecturer, Department of Rehabilitation Medicine, University Malaya. Dr Ian Cameron, Head of the Rehabilitation Studies Unit, Sydney Medical School Northern, The University of Sydney. Reviewed and updated in 2013 by the authors. AGENCY FOR CLINICAL INNOVATION Level 4, Sage Building 67 Albert Avenue Chatswood NSW 2067 PO Box 699 Chatswood NSW 2057 T +61 2 9464 4666 | F +61 2 9464 4728 E [email protected] | www.aci.health.nsw.gov.au Produced by the NSW State Spinal Cord Injury Service. SHPN: (ACI) 140038 ISBN: 978-1-74187-972-8 Further copies of this publication can be obtained from the Agency for Clinical Innovation website at: www.aci.health.nsw.gov.au Disclaimer: Content within this publication was accurate at the time of publication. This work is copyright. It may be reproduced in whole or part for study or training purposes subject to the inclusion of an acknowledgment of the source. It may not be reproduced for commercial usage or sale. Reproduction for purposes other than those indicated above, requires written permission from the Agency for Clinical Innovation. © Agency for Clinical Innovation 2014 Published: February 2014 HS13-136 ACKNOWLEDGEMENTS This document was originally published as a fact sheet for the Rural Spinal Cord Injury Project (RSCIP), a pilot healthcare program for people with a spinal cord injury (SCI) conducted within New South Wales involving the collaboration of Prince Henry & Prince of Wales Hospitals, Royal North Shore Hospital, Royal Rehabilitation Centre Sydney, Spinal Cord Injuries Australia and the Paraplegic & Quadriplegic Association of NSW. -

Scienti®C Review Spastic Movement Disorder
Spinal Cord (2000) 38, 389 ± 393 ã 2000 International Medical Society of Paraplegia All rights reserved 1362 ± 4393/00 $15.00 www.nature.com/sc Scienti®c Review Spastic movement disorder V Dietz*,1 1Paracare, Paraplegic Centre of the University Hospital Balgrist, ZuÈrich, Switzerland This review deals with the neuronal mechanisms underlying spastic movement disorder, assessed by electrophysiological means with the aim of ®rst, a better understanding of the underlying pathophysiology and second, the selection of an adequate treatment. For the patient usually one of the ®rst symptoms of a lesion within the central motor system represents the movement disorder, which is most characteristic during locomotion in patients with spasticity. The clinical examination reveals exaggerated tendon tap re¯exes and increased muscle tone typical of the spastic movement disorder. However, today we know that there exists only a weak relationship between the physical signs obtained during the clinical examination in a passive motor condition and the impaired neuronal mechanisms being in operation during an active movement. By the recording and analysis of electrophysiological and biomechanical parameters during a functional movement such as locomotion, the signi®cance of, for example, impaired re¯ex behaviour or pathophysiology of muscle tone and its contribution to the movement disorder can reliably be assessed. Consequently, an adequate treatment should not be restricted to the cosmetic therapy and correction of an isolated clinical parameter but should be based on the pathophysiology and signi®cance of the mechanisms underlying the disorder of functional movement which impairs the patient. Spinal Cord (2000) 38, 389 ± 393 Keywords: spinal cord injury; spasticity; electrophysiological recordings; treatment Introduction Movement disorders are prominent features of impaired strength of electromyographic (EMG) activation of function of the motor systems and are frequently best antagonistic leg muscles as well as intrinsic and passive re¯ected during gait. -

Amino Acid Disorders 105
AMINO ACID DISORDERS 105 Massaro, A. S. (1995). Trypanosomiasis. In Guide to Clinical tions in biological fluids relatively easy. These Neurology (J. P. Mohrand and J. C. Gautier, Eds.), pp. 663– analyzers separate amino acids either by ion-ex- 667. Churchill Livingstone, New York. Nussenzweig, V., Sonntag, R., Biancalana, A., et al. (1953). Ac¸a˜o change chromatography or by high-pressure liquid de corantes tri-fenil-metaˆnicos sobre o Trypanosoma cruzi in chromatography. The results are plotted as a graph vitro: Emprego da violeta de genciana na profilaxia da (Fig. 1). The concentration of each amino acid can transmissa˜o da mole´stia de chagas por transfusa˜o de sangue. then be calculated from the size of the corresponding O Hospital (Rio de Janeiro) 44, 731–744. peak on the graph. Pagano, M. A., Segura, M. J., DiLorenzo, G. A., et al. (1999). Cerebral tumor-like American trypanosomiasis in Most amino acid disorders can be diagnosed by acquired immunodeficiency syndrome. Ann. Neurol. 45, measuring the concentrations of amino acids in 403–406. blood plasma; however, some disorders of amino Rassi, A., Trancesi, J., and Tranchesi, B. (1982). Doenc¸ade acid transport are more easily recognized through the Chagas. In Doenc¸as Infecciosas e Parasita´rias (R. Veroesi, Ed.), analysis of urine amino acids. Therefore, screening 7th ed., pp. 674–712. Guanabara Koogan, Sa˜o Paulo, Brazil. Spina-Franc¸a, A., and Mattosinho-Franc¸a, L. C. (1988). for amino acid disorders is best done using both South American trypanosomiasis (Chagas’ disease). In blood and urine specimens. Occasionally, analysis of Handbook of Clinical Neurology (P. -

Spinocerebellar Ataxia 17 (SCA17) and Huntington’S Disease-Like 4 (HDL4)
Spinocerebellar ataxia 17 (SCA17) and Huntington’s disease-like 4 (HDL4). Giovanni Stevanin, Alexis Brice To cite this version: Giovanni Stevanin, Alexis Brice. Spinocerebellar ataxia 17 (SCA17) and Huntington’s disease-like 4 (HDL4).. The Cerebellum, Springer, 2008, 7 (2), pp.170-8. 10.1007/s12311-008-0016-1. inserm- 00293796 HAL Id: inserm-00293796 https://www.hal.inserm.fr/inserm-00293796 Submitted on 26 Mar 2009 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Stevanin & Brice, SCA7 and HDL4 1 SPINOCEREBELLAR ATAXIA 17 (SCA17) AND HUNTINGTON’S DISEASE-LIKE 4 (HDL4) GIOVANNI STEVANIN1,2,3 & ALEXIS BRICE1,2,3 1INSERM, U679, 75013 Paris, France; 2Université Pierre et Marie Curie – Paris 6, UMR S679, Institut Fédératif de Recherche en Neurosciences, Groupe Hospitalier Pitié-Salpêtrière, 75013 Paris, France; 3APHP, Groupe Hospitalier Pitié-Salpêtrière, Département de Génétique et Cytogénétique, 75013 Paris, France Correspondence: Giovanni Stevanin, PhD, INSERM U679, Groupe Pitié-Salpêtrière, 47 Boulevard de l’Hôpital, 75651 Paris Cedex 13, France. E-mail: [email protected] Running title: SCA7 and HDL4 Stevanin & Brice, SCA7 and HDL4 2 Abstract Spinocerebellar ataxia 17 (SCA17) or Huntington's disease-like-4 is a neurodegenerative disease caused by the expansion above 44 units of a CAG/CAA repeat in the coding region of the TATA box binding protein (TBP) gene leading to an abnormal expansion of a polyglutamine stretch in the corresponding protein. -

Cerebellar Ataxia
CEREBELLAR ATAXIA Dr. Waqar Saeed Ziauddin Medical University, Karachi, Pakistan What is Ataxia? ■ Derived from a Greek word, ‘A’ : not, ‘Taxis’ : orderly Ataxia is defined as an inability to maintain normal posture and smoothness of movement. Types of Ataxia ■ Cerebellar Ataxia ■ Sensory Ataxia ■ Vestibular Ataxia Cerebellar Ataxia Cerebrocerebellum Spinocerebellum Vestibulocerebellum Vermis Planning and Equilibrium balance Posture, limb and initiating and posture eye movements movements Limb position, touch and pressure sensation Limb ataxia, Eye movement dysdiadochokinesia, disorders, Truncal and gait Dysmetria dysarthria nystagmus, VOR, ataxia hypotonia postural and gait. Gait ataxia Types of Cerebellar Ataxia • Vascular Acute Ataxia • Medications and toxins • Infectious etiologies • Atypical Infectious agents • Autoimmune disorders • Primary or metastatic tumors Subacute Ataxia • Paraneoplastic cerebellar degeneration • Alcohol abuse and Vitamin deficiencies • Systemic disorders • Autosomal Dominant Chronic • Autosomal recessive Progressive • X linked ataxias • Mitochondrial • Sporadic neurodegenerative diseases Vascular Ataxia ▪ Benedikt Syndrome It is a rare form of posterior circulation stroke of the brain. A lesion within the tegmentum of the midbrain can produce Benedikt Syndrome. Disease is characterized by ipsilateral third nerve palsy with contralateral hemitremor. Superior cerebellar peduncle and/or red nucleus damage in Benedikt Syndrome can further lead in to contralateral cerebellar hemiataxia. ▪ Wallenberg Syndrome In -

Spinocerebellar Ataxia Type 29 Due to Mutations in ITPR1: a Case Series and Review of This Emerging Congenital Ataxia Jessica L
Zambonin et al. Orphanet Journal of Rare Diseases (2017) 12:121 DOI 10.1186/s13023-017-0672-7 RESEARCH Open Access Spinocerebellar ataxia type 29 due to mutations in ITPR1: a case series and review of this emerging congenital ataxia Jessica L. Zambonin1*, Allison Bellomo2, Hilla Ben-Pazi3, David B. Everman2, Lee M. Frazer2, Michael T. Geraghty4, Amy D. Harper5, Julie R. Jones2, Benjamin Kamien6, Kristin Kernohan1,4, Mary Kay Koenig7, Matthew Lines4, Elizabeth Emma Palmer8,9, Randal Richardson10, Reeval Segel11, Mark Tarnopolsky12, Jason R. Vanstone4, Melissa Gibbons13, Abigail Collins14, Brent L. Fogel15, Care4Rare Canada Consortium, Tracy Dudding-Byth16 and Kym M. Boycott1,4 Abstract Background: Spinocerebellar ataxia type 29 (SCA29) is an autosomal dominant, non-progressive cerebellar ataxia characterized by infantile-onset hypotonia, gross motor delay and cognitive impairment. Affected individuals exhibit cerebellar dysfunction and often have cerebellar atrophy on neuroimaging. Recently, missense mutations in ITPR1 were determined to be responsible. Results: Clinical information on 21 individuals from 15 unrelated families with ITPR1 mutations was retrospectively collected using standardized questionnaires, including 11 previously unreported singletons and 2 new patients from a previously reported family. We describe the genetic, clinical and neuroimaging features of these patients to further characterize the clinical features of this rare condition and assess for any genotype-phenotype correlation for this disorder. Our cohort consisted of 9 males and 12 females, with ages ranging from 28 months to 49 years. Disease course was non-progressive with infantile-onset hypotonia and delays in motor and speech development. Gait ataxia was present in all individuals and 10 (48%) were not ambulating independently between the ages of 3–12 years of age. -

Diagnostic Clues in Multiple System Atrophy
DO I:10.4274/Tnd.82905 Case Report / Olgu Sunumu Diagnostic Clues in Multiple System Atrophy: A Case Report and Literature Review Multisistem Atrofi Tanısında İpuçları: Bir Olgu Sunumu ve Literatürün Gözden Geçirilmesi Mehmet Yücel, Oğuzhan Öz, Hakan Akgün, Semai Bek, Tayfun Kaşıkçı, İlter Uysal, Yaşar Kütükçü, Zeki Odabaşı Gülhane Military Medical Academy, Ankara, Turkey Sum mary Multiple system atrophy (MSA) is an adult-onset, sporadic, progressive neurodegenerative disease. Based on the consensus criteria, patients with MSA are clinically classified into cerebellar (MSA-C) and parkinsonian (MSA-P) subtypes. In addition to major diagnostic criteria including poor response to levodopa, and presence of pyramidal or cerebellar signs (ataxia) or autonomic failure, certain clinical features or ‘‘red flags’’ may raise the clinical suspicion for MSA. In our case report we present a 67-year-old female patient admitted to our hospital due to inability to walk, with poor response to levodopa therapy, whose neurological examination revealed severe Parkinsonism, ataxia and who fulfilled all criteria for MSA, as rarely seen in clinical practice.(Turkish Journal of Neurology 2013; 19:28-30) Key Words: Multiple system atrophy, autonomic failure, diagnostic criteria Özet Multisistem atrofi (MSA) erişkin dönemde başlayan, ilerleyici, nedeni bilinmeyen sporadik nörodejeneratif bir hastalıktır. MSA kabul görmüş tanı kriterlerine göre klinik olarak serebellar (MSA-C) ve parkinsoniyen (MSA-P) alt tiplerine ayrılmaktadır. Düşük levadopa yanıtı, piramidal, serebellar bulguların (ataksi) ya da otonomik bozukluk olması gibi majör tanı kriterlerininin yanında “red flags” olarak isimlendirilen belirgin klinik bulgular ya da uyarı işaretlerinin olması MSA tanısı için klinik şüpheyi oluşturmalıdır. Olgu sunumunda 67 yaşında yürüyememe şikayeti ile polikliniğimize müracaat eden ve levadopa tedavisine düşük yanıt gösteren ciddi parkinsonizm bulguları ile ataksi bulunan kadın hasta MSA tanı kriterlerini tam olarak karşıladığı ve klinik pratikte nadir görüldüğü için sunduk. -
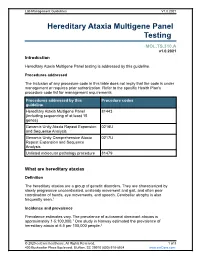
Hereditary Ataxia Multigene Panel Testing
Lab Management Guidelines V1.0.2021 Hereditary Ataxia Multigene Panel Testing MOL.TS.310.A v1.0.2021 Introduction Hereditary Ataxia Multigene Panel testing is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline Hereditary Ataxia Multigene Panel 81443 (including sequencing of at least 15 genes) Genomic Unity Ataxia Repeat Expansion 0216U and Sequence Analysis Genomic Unity Comprehensive Ataxia 0217U Repeat Expansion and Sequence Analysis Unlisted molecular pathology procedure 81479 What are hereditary ataxias Definition The hereditary ataxias are a group of genetic disorders. They are characterized by slowly progressive uncoordinated, unsteady movement and gait, and often poor coordination of hands, eye movements, and speech. Cerebellar atrophy is also frequently seen.1 Incidence and prevalence Prevalence estimates vary. The prevalence of autosomal dominant ataxias is approximately 1-5:100,000.1 One study in Norway estimated the prevalence of hereditary ataxia at 6.5 per 100,000 people.2 © 2020 eviCore healthcare. All Rights Reserved. 1 of 8 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2021 Symptoms Although hereditary ataxias are made up of multiple different conditions, they are characterized by slowly progressive uncoordinated, unsteady movement and gait, and often poor coordination of hands, eye movements, and speech. Cerebellar atrophy is also frequently seen.1 Cause Hereditary ataxias are caused by mutations in one of numerous genes. -
Molecular Diagnostics of Charcot-Marie-Tooth Disease and Related Peripheral Neuropathies
17_Lupski 3/30/06 1:47 PM Page 243 NeuroMolecular Medicine Copyright © 2006 Humana Press Inc. All rights of any nature whatsoever reserved. ISSN0895-8696/06/08:243–254/$30.00 doi: 10.1385/NMM:8:1:243 REVIEW ARTICLE Molecular Diagnostics of Charcot-Marie-Tooth Disease and Related Peripheral Neuropathies Kinga Szigeti,1 Eva Nelis,2,3 and James R. Lupski*,1,4 1Departments of Molecular and Human Genetics, Baylor College of Medicine, Houston, TX; 2Molecular Genetics, Flanders Interuniversity Institute for Biotechnology, Institute Born-Bunge, University of Antwerp, Antwerpen, Belgium; 3Laboratory of Neurogenetics, Institute Born-Borge, University of Antwerp, Antwerpen, Belgium; and 4Pediatrics, Baylor College of Medicine, and Texas Children Hospital, Houston, TX 77030 Received January 10, 2006; Revised January 13, 2006; Accepted January 13, 2006 Abstract DNAdiagnostics plays an important role in the characterization and management of patients manifesting inherited peripheral neuropathies. We describe the clinical integration of molecular diagnostics with medical history, physical examination, and electrophysiological studies. Mole- cular testing can help establish a secure diagnosis, enable genetic counseling regarding recurrence risk, potentially provide prognostic information, and in the near future may be important for the choice of therapies. doi: 10.1385/NMM:8:1:243 Index Entries:Molecular diagnostics; Charcot-Marie-Tooth disease; CMT; hereditary neuropathy with liability to pressure palsies; HNPP; Dejerine-Sottas neuropathy; DSN; congenital hypomyelinating neuropathy; CHN; CMT1A duplication; HNPP deletion. Introduction genetic testing, one needs to be familiar with the diagnostic tests available, choose the appropriate Molecular genetic diagnosis has become an inte- patients for testing, and utilize the diagnostic tools gral part of the evaluation of patients with hered- in a logical fashion to optimize the use of resources.