An Overview of the New Classification of Periodontal and Peri-Implant Diseases and Conditions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters
microorganisms Article Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters Andrea Butera , Simone Gallo * , Carolina Maiorani, Domenico Molino, Alessandro Chiesa, Camilla Preda, Francesca Esposito and Andrea Scribante * Section of Dentistry–Department of Clinical, Surgical, Diagnostic and Paediatric Sciences, University of Pavia, 27100 Pavia, Italy; [email protected] (A.B.); [email protected] (C.M.); [email protected] (D.M.); [email protected] (A.C.); [email protected] (C.P.); [email protected] (F.E.) * Correspondence: [email protected] (S.G.); [email protected] (A.S.) Abstract: Periodontitis consists of a progressive destruction of tooth-supporting tissues. Considering that probiotics are being proposed as a support to the gold standard treatment Scaling-and-Root- Planing (SRP), this study aims to assess two new formulations (toothpaste and chewing-gum). 60 patients were randomly assigned to three domiciliary hygiene treatments: Group 1 (SRP + chlorhexidine-based toothpaste) (control), Group 2 (SRP + probiotics-based toothpaste) and Group 3 (SRP + probiotics-based toothpaste + probiotics-based chewing-gum). At baseline (T0) and after 3 and 6 months (T1–T2), periodontal clinical parameters were recorded, along with microbiological ones by means of a commercial kit. As to the former, no significant differences were shown at T1 or T2, neither in controls for any index, nor in the experimental -

Management of Acute Periodontal Abscess Mimicking Acute Apical Abscess in the Anterior Lingual Region: a Case Report
Open Access Case Report DOI: 10.7759/cureus.5592 Management of Acute Periodontal Abscess Mimicking Acute Apical Abscess in the Anterior Lingual Region: A Case Report Omar A. Alharbi 1 , Muhammad Zubair Ahmad 1 , Atif S. Agwan 1 , Durre Sadaf 1 1. Conservative Dentistry, Qassim University, College of Dentistry, Buraydha, SAU Corresponding author: Muhammad Zubair Ahmad, [email protected] Abstract Purulent infections of periodontal tissues are known as periodontal abscesses localized to the region of the involved tooth. Due to the high prevalence rate and aggressive symptoms, it is considered a dental emergency; urgent care is mandatory to maintain the overall health and well being of the patient. This case report describes the management of a patient who presented with an acute periodontal abscess secondary to poor oral hygiene. Clinically and radiographically, the lesion was mimicking an acute apical abscess secondary to pulpal necrosis. Periodontal treatment was started after completion of antibiotic therapy. The clinical presentation of the condition and results of the recovery, along with a brief review of relevant literature are discussed. Categories: Pain Management, Miscellaneous, Dentistry Keywords: periodontal abscess, antimicrobial agents, dental pulp test, dental pulp necrosis, apical suppurative periodontitis Introduction Periodontium, as a general term, describes the tissues surrounding and supporting the tooth structure. A localized purulent infection of the periodontal tissues adjacent to a periodontal pocket, also known as a periodontal abscess, is a frequently encountered periodontal condition that may be characterized by the rapid destruction of periodontal tissues [1-2]. The symptoms generally involve severe pain, swelling of the alveolar mucosa or gingiva, a reddish blue or red appearance of the affected tissues, and difficulty in chewing [1-3]. -

Cytokines and Their Genetic Polymorphisms Related to Periodontal Disease
Journal of Clinical Medicine Review Cytokines and Their Genetic Polymorphisms Related to Periodontal Disease Małgorzata Kozak 1, Ewa Dabrowska-Zamojcin 2, Małgorzata Mazurek-Mochol 3 and Andrzej Pawlik 4,* 1 Chair and Department of Dental Prosthetics, Pomeranian Medical University, Powsta´nców Wlkp 72, 70-111 Szczecin, Poland; [email protected] 2 Department of Pharmacology, Pomeranian Medical University, Powsta´nców Wlkp 72, 70-111 Szczecin, Poland; [email protected] 3 Department of Periodontology, Pomeranian Medical University, Powsta´nców Wlkp 72, 70-111 Szczecin, Poland; [email protected] 4 Department of Physiology, Pomeranian Medical University, Powsta´nców Wlkp 72, 70-111 Szczecin, Poland * Correspondence: [email protected] Received: 24 October 2020; Accepted: 10 December 2020; Published: 14 December 2020 Abstract: Periodontal disease (PD) is a chronic inflammatory disease caused by the accumulation of bacterial plaque biofilm on the teeth and the host immune responses. PD pathogenesis is complex and includes genetic, environmental, and autoimmune factors. Numerous studies have suggested that the connection of genetic and environmental factors induces the disease process leading to a response by both T cells and B cells and the increased synthesis of pro-inflammatory mediators such as cytokines. Many studies have shown that pro-inflammatory cytokines play a significant role in the pathogenesis of PD. The studies have also indicated that single nucleotide polymorphisms (SNPs) in cytokine genes may be associated with risk and severity of PD. In this narrative review, we discuss the role of selected cytokines and their gene polymorphisms in the pathogenesis of periodontal disease. Keywords: periodontal disease; cytokines; polymorphism 1. -

Prevention and Treatment of Periodontal Diseases in Primary Care Guidance in Brief
Scottish Dental SD Clinical Effectiveness Programme cep Prevention and Treatment of Periodontal Diseases in Primary Care Guidance in Brief June 2014 Scottish Dental SD Clinical Effectiveness Programme cep The Scottish Dental Clinical Effectiveness Programme (SDCEP) is an initiative of the National Dental Advisory Committee (NDAC) in partnership with NHS Education for Scotland. The Programme provides user-friendly, evidence-based guidance on topics identified as priorities for oral health care. SDCEP guidance aims to support improvements in patient care by bringing together, in a structured manner, the best available information that is relevant to the topic and presenting this information in a form that can be interpreted easily and implemented. Supporting the provision of safe, effective, person-centred care Scottish Dental SD Clinical Effectiveness Programme cep Prevention and Treatment of Periodontal Diseases in Primary Care Guidance in Brief June 2014 Prevention and Treatment of Periodontal Diseases in Primary Care Cover image: Colour-enhanced photomicrograph of oral bacterial colonies growing on an agar plate. Derren Ready, Wellcome Images. © Scottish Dental Clinical Effectiveness Programme SDCEP operates within NHS Education for Scotland. You may copy or reproduce the information in this document for use within NHS Scotland and for non-commercial educational purposes. Use of this document for commercial purposes is permitted only with written permission. ISBN 978 1 905829 18 7 Published June 2014 Scottish Dental Clinical Effectiveness Programme Dundee Dental Education Centre, Frankland Building, Small’s Wynd, Dundee DD1 4HN Email [email protected] Tel 01382 425751 / 425771 Website www.sdcep.org.uk Prevention and Treatment of Periodontal Diseases in Primary Care Introduction Prevention and Treatment of Periodontal Diseases in Primary Care is designed to assist and support primary care dental teams in providing appropriate care for patients both at risk of and with periodontal diseases. -

Periodontitis and Peri-Implantitis Biomarkers in Human Oral Fluids and the Null-Allele Mouse Model
Department of Cell Biology of Oral Diseases Institute of Dentistry, Biomedicum Helsinki, University of Helsinki, Helsinki, Finland Department of Oral and Maxillofacial Diseases Helsinki University Central Hospital (HUCH), University of Helsinki, Helsinki, Finland Department of Diagnostics and Oral Medicine Institute of Dentistry, University of Oulu, Oulu University Hospital, Oulu, Finland PERIODONTITIS AND PERI-IMPLANTITIS BIOMARKERS IN HUMAN ORAL FLUIDS AND THE NULL-ALLELE MOUSE MODEL Heidi Kuula Academic Dissertation To be presented with the permission of the Faculty of Medicine, University of Helsinki, for public discussion in the Lecture Hall 1 at Biomedicum Helsinki, Haartmaninkatu 8, Helsinki, on June 12th 2009, at 12 noon Helsinki 2009 Supervised by: Professor Timo Sorsa, DDS, PhD, Dipl Perio Department of Cell Biology of Oral Diseases, Institute of Dentistry, University of Helsinki, and Department of Oral and Maxillofacial Diseases, Helsinki University Central Hospital (HUCH) Helsinki, Finland Professor Tuula Salo, DDS, PhD Department of Diagnostics and Oral Medicine, Institute of Dentistry, University of Oulu, and Oulu University Hospital (OYS) Oulu, Finland Reviewed by: Assistant Professor Marja L. Laine, DDS, PhD Department of Oral Microbiology, Academic Centre for Dentistry Amsterdam Amsterdam, the Netherlands Professor Denis F. Kinane, BDS, PhD Associate Dean for Research and Enterprise Delta Endowed Professor Director, Oral Health and Systemic Disease Research Group University of Louisville Louisville, Kentucky, USA Opponent: Professor Anders Gustafsson, DDS, PhD Institute of Odontology Department of Periodontology Karolinska Institutet Huddinge, Sweden ISBN 978-952-92-5634-1 (paperback) ISBN 978-952-10-5603-1 (PDF) Helsinki 2009 Yliopistopaino 2 CONTENTS List of original publications Abbreviations Abstract 1. Introduction 2. -

Periodontal Practice Patterns
PERIODONTAL PRACTICE PATTERNS A Thesis Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of the Ohio State University By Janel Kimberlay Yu, D.D.S. Graduate Program in Dentistry The Ohio State University 2010 Dissertation Committee: Dr. Angelo Mariotti, Advisor Dr. Jed Jacobson Dr. Eric Seiber Copyright by Janel Kimberlay Yu 2010 Abstract Background: Differences in the rates of dental services between geographic regions are important since major discrepancies in practice patterns may suggest an absence of evidence-based clinical information leading to numerous treatment plans for similar dental problems and the misallocation of limited resources. Variations in dental care to patients may result from characteristics of the periodontist. Insurance claims data in this study were compared to the characteristics of periodontal providers to determine if variations in practice patterns exist. Methods: Claims data, between 2000-2009 from Delta Dental of Ohio, Michigan, Indiana, New Mexico, and Tennessee, were examined to analyze the practice patterns of 351 periodontists. For each provider, the average number of select CDT periodontal codes (4000-4999), implants (6010), and extractions (7140) were calculated over two time periods in relation to provider variable, including state, urban versus rural area, gender, experience, location of training, and membership in organized dentistry. Descriptive statistics were performed to depict the data using measures of central tendency and measures of dispersion. ii Results: Differences in periodontal procedures were present across states. Although the most common surgical procedure in the study period was osseous surgery, greater increases over time were observed in regenerative procedures (bone grafts, biologics, GTR) when compared to osseous surgery. -

Assessment of a Panel of Risk Indicators in Severe Periodontitis Patients
Assessment of a panel of risk indicators in severe periodontitis patients Ciobanu L.¹, Miricescu D. ², Didilescu A.³, Țărmure V.4 ¹PhD Student in Dental Medicine, Division of Microbiology, Faculty of Dental Medicine, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania ²Senior Lecturer, Division of Biochemistry, Faculty of Dental Medicine, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania ³Professor, Division of Embryology, Faculty of Dental Medicine, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania 4Associate Professor, Department of Orthodontics, Faculty of Dental Medicine, Iuliu Hațieganu University of Medicine and Pharmacy, Cluj-Napoca, Romania Correspondence to: Name: Ciobanu Lidia Address: Blvd. Camil Ressu 49, Bl. H26, Sc. D, Ap.61, Bucharest, Romania Phone: +40 724962500 E-mail address: [email protected] Abstract Aim and objectives The purpose of this study was to analyse a panel of risk indicators in a group of twenty-two patients with severe periodontitis. We also aimed to test possible associations between these indicators and the severity of periodontitis assessed by clinical attachment loss (CAL) mean values. Material and methods Periodontal status was assessed based on the CDC/AAP periodontitis case definition for population-based studies. Risk indicators, including age, gender, weight and height, level of education, and smoking habits, were recorded. Salivary cortisol level, as a marker of chronic stress, was also measured. Results The mean age of the patients was 44.86 (SD 12.81; range 24 to 72). Ten females (45.5%) were enrolled. Testing possible associations between risk indicators and CAL mean values showed no statistical significant correlations, although trends of positive correlations were found between males, BMI, and CAL, respectively Conclusions The present results suggest that a high BMI, as well as masculine gender, could have been important risk factors for severe periodontitis in this study group. -

Acute Periodontal Abscess in an Adolescent Patient: Case Report
ISSN: 2639-0434 Madridge Journal of Dentistry and Oral Surgery Case Report Open Access Acute Periodontal Abscess in an Adolescent Patient: Case Report Alparslan Dilsiz* Department of Periodontology, Faculty of Dentistry, Atatürk University, Erzurum, Turkey Article Info Abstract *Corresponding author: Periodontal abscess has been defined as a suppurative lesion that is associated with Alparslan Dilsiz periodontal breakdown and pus collection in the gingival wall of the periodontal pocket. Professor Department of Periodontology The prevalence of periodontal abscess is relatively high and it affects the prognosis of Faculty of Dentistry, Atatürk University the tooth. In this article, a patient with acute periodontal abscess due to poor oral Turkey hygiene was treated periodontically 10 days after the start of antibiotic therapy. The Fax: +90 442 2361375 clinical features and likely healing results of the lesion were discussed and related Tel: +90 442 2360940 E-mail: [email protected] literatures were reviewed. Keywords: Periodontal Abscess; Periodontal Pocket; Alveolar Bone Resorption; Received: August 16, 2017 Accepted: September 3, 2017 Suppuration; Anti-Bacterial Agents; Periodontal Atrophy and Periodontal Debridement. Published: September 8, 2017 Introduction Citation: Dilsiz A. Acute Periodontal Abscess in an Adolescent Patient: Case Periodontal abscess, which is a localized purulent infection of the periodontal Report. Madridge J Dent Oral Surg. 2017; tissues adjacent to a periodontal pocket, is a frequent periodontal condition in which 2(2): 77-79. periodontal tissues may be rapidly destroyed [1,2]. Major symptoms of a periodontal doi: 10.18689/mjdl-1000118 abscess are known as the spontaneous or evoked pain, gingival or mucosal swelling, Red or reddish blue discoloration of affected tissue [1-4]. -

Periodontal Health, Gingival Diseases and Conditions 99 Section 1 Periodontal Health
CHAPTER Periodontal Health, Gingival Diseases 6 and Conditions Section 1 Periodontal Health 99 Section 2 Dental Plaque-Induced Gingival Conditions 101 Classification of Plaque-Induced Gingivitis and Modifying Factors Plaque-Induced Gingivitis Modifying Factors of Plaque-Induced Gingivitis Drug-Influenced Gingival Enlargements Section 3 Non–Plaque-Induced Gingival Diseases 111 Description of Selected Disease Disorders Description of Selected Inflammatory and Immune Conditions and Lesions Section 4 Focus on Patients 117 Clinical Patient Care Ethical Dilemma Clinical Application. Examination of the gingiva is part of every patient visit. In this context, a thorough clinical and radiographic assessment of the patient’s gingival tissues provides the dental practitioner with invaluable diagnostic information that is critical to determining the health status of the gingiva. The dental hygienist is often the first member of the dental team to be able to detect the early signs of periodontal disease. In 2017, the American Academy of Periodontology (AAP) and the European Federation of Periodontology (EFP) developed a new worldwide classification scheme for periodontal and peri-implant diseases and conditions. Included in the new classification scheme is the category called “periodontal health, gingival diseases/conditions.” Therefore, this chapter will first review the parameters that define periodontal health. Appreciating what constitutes as periodontal health serves as the basis for the dental provider to have a stronger understanding of the different categories of gingival diseases and conditions that are commonly encountered in clinical practice. Learning Objectives • Define periodontal health and be able to describe the clinical features that are consistent with signs of periodontal health. • List the two major subdivisions of gingival disease as established by the American Academy of Periodontology and the European Federation of Periodontology. -

Application of Vibroacoustic Diagnosis in Assessing Bridges Connecting Teeth and Implants to Treat Tooth Absence in Sea Vessel Crews
POLISH MARITIME RESEARCH 1 (105) 2020 Vol. 27; pp. 188-194 10.2478/pomr-2020-0020 APPLICATION OF VIBROACOUSTIC DIAGNOSIS IN ASSESSING BRIDGES CONNECTING TEETH AND IMPLANTS TO TREAT TOOTH ABSENCE IN SEA VESSEL CREWS Artur Rasinski Military Institute of Medicine, Clinics of Otorhinolaryngology and Laryngological Oncology with the Clinical Ward of Oral and Maxillo-facial Surgery , Poland Grzegorz Klekot Warsaw University of Technology, Faculty of Automotive and Construction Machinery Engineering, Poland Piotr Skopiński Department of Histology and Embryology, Centre for Biostructure Research, Medical University of Warsaw, Poland ABSTRACT Implant treatment is a proven method in dentistry for partial and complete missing teeth reconstruction. In some clinical situations it is advisable to limit the number of implants, which can be obtained by making a bridge connecting the patient’s own tooth with the implant. So far, the possibility of using safe and permanent connections of natural teeth with implants has been examined to a small extent due to the dangers resulting from the different mobility of dental implants and teeth. An attempt was made to use vibro-acoustic techniques to evaluate various combinations of teeth and implants. Pilot studies were carried out on cadavers-pig mandibles with implants. There were recorded sounds in the immediate vicinity of the mandible formed in response to impulse excitations carried out with a point hit against a tooth or implant before and after their joining with a bridge. The comparison of spectra allows to see features indicating a high probability of being able to distinguish between the examined configurations. The results of the research should contribute to a better understanding of the mutual relations between the dental implant and the tooth, which are included in bridge. -
Staging and Grading Periodontitis
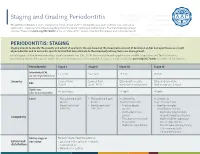
Staging and Grading Periodontitis The 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions resulted in a new classification of periodontitis characterized by a multidimensional staging and grading system. The charts below provide an overview. Please visit perio.org/2017wwdc for the complete suite of reviews, case definition papers, and consensus reports. PERIODONTITIS: STAGING Staging intends to classify the severity and extent of a patient’s disease based on the measurable amount of destroyed and/or damaged tissue as a result of periodontitis and to assess the specific factors that may attribute to the complexity of long-term case management. Initial stage should be determined using clinical attachment loss (CAL). If CAL is not available, radiographic bone loss (RBL) should be used. Tooth loss due to periodontitis may modify stage definition. One or more complexity factors may shift the stage to a higher level. Seeperio.org/2017wwdc for additional information. Periodontitis Stage I Stage II Stage III Stage IV Interdental CAL 1 – 2 mm 3 – 4 mm ≥5 mm ≥5 mm (at site of greatest loss) Severity Coronal third Coronal third Extending to middle Extending to middle RBL (<15%) (15% - 33%) third of root and beyond third of root and beyond Tooth loss No tooth loss ≤4 teeth ≥5 teeth (due to periodontitis) Local • Max. probing depth • Max. probing depth In addition to In addition to ≤4 mm ≤5 mm Stage II complexity: Stage III complexity: • Mostly horizontal • Mostly horizontal • Probing depths • Need for -

New Classification of Periodontal Diseases
BDJOpen www.nature.com/bdjopen ARTICLE OPEN New classification of periodontal diseases (NCPD): an application in a sub-Saharan country William Ndjidda Bakari 1, Diabel Thiam1, Ndeye Lira Mbow1, Anna Samb1, Mouhamadou Lamine Guirassy1, Ahmad Moustapha Diallo 1, Abdoulaye Diouf1, Adam Seck Diallo1 and Henri Michel Benoist1 PURPOSE: To determine the clinical and radiological profile of periodontitis according to the 2018 NCPD, in a Dakar (Senegal) based periodontal clinic. METHODS: This is a descriptive study based on patient’s records in the periodontology clinic. The study was conducted between November 2018 and February 2020 (15 months). All periodontitis cases were included in the study. Incomplete records (due to lack of radiographic workup or unusable periodontal charting) were excluded. Periodontitis diagnosis was established based on criteria used in the 2018 NCPD. Statistical analysis was carried out using SPSS version 20.0, with the significance threshold set at 0.05. RESULTS: A total number of 517 patient records were collected during the study period but only 127 periodontitis records were complete. The mean age of participants was 46.8 ± 13.8 years and 63.8% of participants were males. The mean plaque index and bleeding on probing (BOP) were 74% ± 21.3 and 58.1% ± 25.1, respectively. The mean maximum clinical attachment loss was 8.7 mm ±2.7, with a probing depth greater than 6 mm present in 50.4% of the sample. The median number of missing teeth was 3 (interquartile range 5–1). Pathological mobility was present in 60.6% of the patients and 78.0% had occlusion problems.