Colorado Clinical and Translational Sciences Institute (CCTSI)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
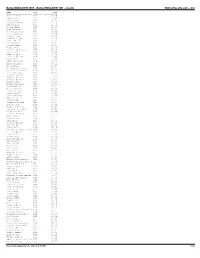
Bolderboulder 2005 - Bolderboulder 10K - Results Onlineraceresults.Com
BolderBOULDER 2005 - BolderBOULDER 10K - results OnlineRaceResults.com NAME DIV TIME ---------------------- ------- ----------- Michael Aish M28 30:29 Jesus Solis M21 30:45 Nelson Laux M26 30:58 Kristian Agnew M32 31:10 Art Seimers M32 31:51 Joshua Glaab M22 31:56 Paul DiGrappa M24 32:14 Aaron Carrizales M27 32:23 Greg Augspurger M27 32:26 Colby Wissel M20 32:36 Luke Garringer M22 32:39 John McGuire M18 32:42 Kris Gemmell M27 32:44 Jason Robbie M28 32:47 Jordan Jones M23 32:51 Carl David Kinney M23 32:51 Scott Goff M28 32:55 Adam Bergquist M26 32:59 trent r morrell M35 33:02 Peter Vail M30 33:06 JOHN HONERKAMP M29 33:10 Bucky Schafer M23 33:12 Jason Hill M26 33:15 Avi Bershof Kramer M23 33:17 Seth James DeMoor M19 33:20 Tate Behning M23 33:22 Brandon Jessop M26 33:23 Gregory Winter M26 33:25 Chester G Kurtz M30 33:27 Aaron Clark M18 33:28 Kevin Gallagher M25 33:30 Dan Ferguson M23 33:34 James Johnson M36 33:38 Drew Tonniges M21 33:41 Peter Remien M25 33:45 Lance Denning M43 33:48 Matt Hill M24 33:51 Jason Holt M18 33:54 David Liebowitz M28 33:57 John Peeters M26 34:01 Humberto Zelaya M30 34:05 Craig A. Greenslit M35 34:08 Galen Burrell M25 34:09 Darren De Reuck M40 34:11 Grant Scott M22 34:12 Mike Callor M26 34:14 Ryan Price M27 34:15 Cameron Widoff M35 34:16 John Tribbia M23 34:18 Rob Gilbert M39 34:19 Matthew Douglas Kascak M24 34:21 J.D. -

Jacob Markowitz Award Given to Past President
Biomaterials Forum, the official news magazine of the Society For Biomaterials, is published quarterly to serve the biomaterials community. Society members receive Biomaterials Forum as a benefit of membership. Non-members may subscribe to the magazine at the annual rate of $48. For subscription information, or membership inquiries, contact the Membership Department at the Society office (e-mail: [email protected]) or visit the Society’s Web site, www.biomaterials.org. The official news magazine of the SOCIETY FOR BIOMATERIALS • Volume 26, Issue 4 It is the policy of the Society For Biomaterials that all articles reflect only the views of the Executive Editor Martine LaBerge, Clemson University authors and that publication of articles or 501 Rhodes Research Center, Clemson, SC 29634-0905 Phone: (864) 656-5557 • Fax: (864) 656-4466 advertisements within Biomaterials Forum does E-mail: [email protected] not constitute endorsement by the Society or its agents of products, services, or views expressed Managing Editor Frank Scussa, Society For Biomaterials 17000 Commerce Parkway, Mt. Laurel, NJ 08054 herein. No representation is made as to the Phone: (856) 439-0500 • Fax: (856) 439-0525 accuracy hereof and the publication is printed E-mail: [email protected] subject to errors and omissions. Articles that do Government News John A. Tesk, National Institute of Standards and Technology not have an author byline may originate from Contributing Editor Industrial Liaison Office press releases. The Society For Biomaterials 100 Bureau Dr., Stop 1005, Gaithersburg, MD 20899-1005 Phone: (301) 975-6799 • Fax: (301) 963-9143 retains press releases on file for a period of one E-mail: [email protected] year from the date of publication. -

Girl Scout Scavenger Hunt Answer Sheet
Girl Scout Scavenger Hunt Answer Sheet (We have attempted to find all answers that are correct in this answer sheet. There is a possibility that we may have missed one or more. If you find an answer that is not included on this sheet, please take these steps: • Check your answer to make sure you have bio information to back it up • Send an email to [email protected] and share your information with Colorado Women’s Hall of Fame • You will receive a response about your answer • If appropriate, we will add your answer to the Answer Sheet and reissue it to the Girl Scout office so future troops doing the exercise will have your answer included. Thank you for delving into the remarkable achievements of our Inductees.) One of the options for earning a Colorado Women’s Hall (CWHF) of Fame fun patch is to complete the Scavenger Hunt below. There are clues at the end of the list that may help you find some answers. Please answer at least 15 of the 25 questions below using the following website as your source: www.cogreatwomen.org 1. How often does the Colorado Women’s Hall of Fame induct new women into the Hall? How many women are inducted at each Induction? ANSWER: • Every 2 years on an even year cycle, e.g.2020 • Ten women are inducted (4 historical and 6 contemporary). 2. What are the three criteria for a woman being selected as an Inductee into the Colorado Women’s Hall of Fame? Who can nominate? When? ANSWER: Criteria: • Made significant and enduring contributions to her fil(40%). -

Acknowledgment of Reviewers, 2009
Proceedings of the National Academy ofPNAS Sciences of the United States of America www.pnas.org Acknowledgment of Reviewers, 2009 The PNAS editors would like to thank all the individuals who dedicated their considerable time and expertise to the journal by serving as reviewers in 2009. Their generous contribution is deeply appreciated. A R. Alison Adcock Schahram Akbarian Paul Allen Lauren Ancel Meyers Duur Aanen Lia Addadi Brian Akerley Phillip Allen Robin Anders Lucien Aarden John Adelman Joshua Akey Fred Allendorf Jens Andersen Ruben Abagayan Zach Adelman Anna Akhmanova Robert Aller Olaf Andersen Alejandro Aballay Sarah Ades Eduard Akhunov Thorsten Allers Richard Andersen Cory Abate-Shen Stuart B. Adler Huda Akil Stefano Allesina Robert Andersen Abul Abbas Ralph Adolphs Shizuo Akira Richard Alley Adam Anderson Jonathan Abbatt Markus Aebi Gustav Akk Mark Alliegro Daniel Anderson Patrick Abbot Ueli Aebi Mikael Akke David Allison David Anderson Geoffrey Abbott Peter Aerts Armen Akopian Jeremy Allison Deborah Anderson L. Abbott Markus Affolter David Alais John Allman Gary Anderson Larry Abbott Pavel Afonine Eric Alani Laura Almasy James Anderson Akio Abe Jeffrey Agar Balbino Alarcon Osborne Almeida John Anderson Stephen Abedon Bharat Aggarwal McEwan Alastair Grac¸a Almeida-Porada Kathryn Anderson Steffen Abel John Aggleton Mikko Alava Genevieve Almouzni Mark Anderson Eugene Agichtein Christopher Albanese Emad Alnemri Richard Anderson Ted Abel Xabier Agirrezabala Birgit Alber Costica Aloman Robert P. Anderson Asa Abeliovich Ariel Agmon Tom Alber Jose´ Alonso Timothy Anderson Birgit Abler Noe¨l Agne`s Mark Albers Carlos Alonso-Alvarez Inger Andersson Robert Abraham Vladimir Agranovich Matthew Albert Suzanne Alonzo Tommy Andersson Wickliffe Abraham Anurag Agrawal Kurt Albertine Carlos Alos-Ferrer Masami Ando Charles Abrams Arun Agrawal Susan Alberts Seth Alper Tadashi Andoh Peter Abrams Rajendra Agrawal Adriana Albini Margaret Altemus Jose Andrade, Jr. -
Annual Meeting & Exposition
FINAL PROGRAM ANNUAL MEETING & EXPOSITION BIOMATERIALS RESEARCH: Hitting all the right notes, and avoiding the translational blues APRIL 20-23, 2021 www.biomaterials.org YOUR NAME,OUR REPUTATION DELIVERING CLINICAL UTILITY Our business model is designed to adapt to our client’s specific manufacturing and material development needs. We o er the resources, knowledge, and experience necessary to provide rapid research and development and a smooth transition into commercial production. To find out more about what we can do for you: www.tescoassociates.com QUALITY CLEAN ROOMS Our team puts the quality and • 12 ISO Class 7 Cleanroom Suites integrity of the device first in that are ISO Class 6 capable every stage of development. • Independent suite design to TESco has a stringent and robust facilitate proper line clearance quality management system, certified to ISO 13485:2016 and • The multiple phases of production, registered with FDA 1226183. prototyping and material preparation can be completed simultaneously EXPERIENCE MATERIAL INNOVATION • Stringent BioBurden control • Injection Molding & Extrusion We have a full portfolio of material • Controlled anteroom to allow • Material Selection and Compounding formulations with FDA master the transferring of product from files in place. Our knowledge of one process stage to another • FDA Submission Assistance bioabsorbable/biodurable polymers without leaving the cleanroom • Packaging and Sterilization Support and co-polymers covers a wide range environment • Assembly of molecular weights. APRIL 20-23, 2021 BIOMATERIALS RESEARCH: HITTING ALL THE RIGHT NOTES, AND AVOIDING THE TRANSLATIONAL BLUES YOUR NAME,OUR REPUTATION DELIVERING CLINICAL UTILITY Our business model is designed to adapt to our client’s specific manufacturing and material development needs. -

Kristi Anseth
Y Previous Tis Lahiri Tis Lahiri Speakers Memorial Seminar The Department of Chemical and 2014 James C. Liao Biomolecular Engineering 2013 Karen K. Gleason presents 2011 Ann L. Lee VANDERBILT UNIVERSIT 2009 Jeffrey Siirola Kristi Anseth 2008 Rakesh Agrawal Distinguished Professor, Tisone Professor, 2007 Douglas Lauffenberger Associate Professor of Surgery, and Howard Hughes Medical Institute Investigator 2006 Stanley I. Sandler University of Colorado, Boulder, CO 2005 Octave Levenspiel 2004 Mark E. Davis 2003 Timothy J. Anderson Cellular Control in a 2002 Arthur W. Westerburg Couple of Clicks 2001 Edward L. Cussler 2000 John M. Prausnitz 1999 Ronald W. Rousseau Monday, November 2, 2015 1998 Phillip C. Wankat 1997 Richard M. Felder 3:10 p.m.—4:00 p.m. 1996 H. Scott Fogler 134 Featheringill Hall Reception at 2:45pm Kristi Anseth Cellular Control in a Couple of Clicks Itinerary Sunday, November 1, 2015 - Flight arrives at 5:10pm. Kane Jennings or John Wilson Methods for culturing mammalian cells in a biologically relevant context are increasingly needed to study cell and tissue physiology, expand will pick up and take you to theVandy Marriott hotel, confirmation #91053507 and differentiate progenitor cells, and to grow replacement tissues for 6:30pm - Dinner at Husk with Kane Jennings, Ethan Lippmann and John Wilson regenerative medicine. Two-dimensional culture has been the paradigm for in Monday, November 2, 2015 vitro cell culture; however, evidence and intuition suggest that cells behave differently when they are isolated from the complex architecture of their 8:00am - 9:10am Breakfast with Paul Laibinis, Professor, ChBE will meet you native tissues and constrained to petri dishes or material surfaces with at the hotel. -

The Emergence of Tissue Engineering As a Research Field
5.0 Who Are the Tissue Engineers? This section examines the people and institutions that are active in tissue engineering or, in a few cases, played a key role in the past. We review some characteristics of the community of tissue engineers viewed in aggregate, introduce specific individuals and six major centers of activity that have played central roles in research or training since the earliest days of the emergence of tissue engineering, and conclude with a few observations on the corporate sector. Our focus here is on those who are actually doing tissue engineering; the role of funding agencies is addressed in a later section. Our analysis draws heavily on a roster of 231 tissue engineers compiled by the study team, and presented in Appendix 2. These include individuals who have published in the realm of tissue engineering, have trained with notable names in the field, or have otherwise self-proclaimed themselves as tissue engineers. The roster is not intended to be a definitive list of those who should be considered tissue engineers – rather, it should be viewed as a convenience sample intended to shed light in a qualitative sense on the nature of tissue engineering and its participants, and to provide an overall sense of trends affecting the character of the field. With that purpose in mind, however, we believe that the list does contain the great majority of academic, non-physician researchers with faculty appointments in the United States and Canada who have identified tissue engineering explicitly as an important component of their research interests. In addition, the list includes a selection of the most prominent physician-researchers in the field, along with a small sampling of individuals in the corporate sector. -

The TERMIS-Americas 2013 Annual Conference & Exposition PROGRAM
P ROGRAM The TERMIS-Americas 2013 Annual Conference & Exposition 3 CELEBRATING 25 YEARS g/am201 OF TRANSFORMATIVE r SCIENCE & ENGINEERING .termis.o w November 10-13, 2013 ww Hyatt Regency Atlanta Atlanta, Georgia Hosted by: TABLE of CONTENTS Welcome …. 4 General Information …. 5 Bench to Business Workshop …. 6 Women in TERM Luncheon …. 7 Opening Symposium …. 8 Opening Day Schedule Sunday, November 10 …. 9 Podium Presentations Monday, November 11 …. 10 - 14 Podium Presentations Tuesday, November 12 …. 15 - 18 Podium Presentations Wednesday, November 13 …. 19 - 24 Poster Session I Monday, November 11 …. 25 - 32 Poster Session II Tuesday, November 12 …. 33 - 41 Student & Young Investigator Section Welcome & Activities …. 43 - 44 Student Poster Competition …. 45 WFIRM YIA Award Winners …. 46 TERMIS-AM 2013 Award Winners …. 47 - 48 Exhibitor Floorplan and Listing …. 49 - 52 Sponsors …. 53 - 54 OPENING RECEPTION Hosted by the Exhibitors and Sponsors Sunday, November 10, 2013 7:00 - 9:00 PM Located in the Regency Ballroom 3 GENERAL INFORMATION November 10, 2013 SCIENTIFIC ADVISORY COMMITTEE Robert Guldberg, PhD, Georgia Institute of Technology, Dear Fellow TERMIS Attendees: Conference Chair and TERMIS-AM Chapter Chair On behalf of the scientific advisory committee, the international community of TERMIS members, and everyone involved in supporting the TERMIS-Americas (TERMIS-AM) 2013 Conference, we would like Todd McDevitt, PhD, Georgia Institute of Technology, to personally welcome you to Atlanta, Georgia. Scientific Program Chair The theme of this year’s meeting, “Celebrating 25 years of Transformative Science & Engineering,” Stephen Badylak, PhD, MD, University of Pittsburgh was inspired by the first federally funded tissue engineering workshop in 1998. -

2013 CU Answer Book
2013 CU Answer Book Institutional Research | Office of the Vice President for Budget and Finance June 2013 About CU CU History The University of Colorado dates back to the early days of Colorado. At its first session in 1861, the Colorado territorial legislature passed an act providing for the creation of a university in Boulder. To establish the university, the legislature appropriated $15,000, which was matched by Boulder residents. The Civil War delayed the formal founding of the university until 1876, the year Colorado became a state. The doors to Old Main opened on September 5, 1877. Old Main still stands and is used by many members of the university community. CU has grown dramatically since its early days. It is now a system with four campuses: Boulder, Colorado Springs, Denver and the Anschutz Medical Campus. In 1974 the Board of Regents officially established the CU System, led by a president, with each campus led by a chancellor. The Colorado Springs campus began in the 1920s as an extension center for the Boulder campus. By the 1960s the extension center had grown to more than 1,200 students. A gift of the land and buildings of the Cragmor Sanatorium provided a permanent site for the campus, and in 1965, the extension center became the University of Colorado Colorado Springs. The Denver Campus also began as an extension site, first offering courses from Boulder in 1912. It became an official extension center in 1957 with authority to grant degrees, and then became an autonomous CU campus in 1974. It shares the Auraria campus with the Community College of Denver and Metropolitan State College of Denver. -

MEET the FACULTY CANDIDATES Candidates Will Be Present to Meet with Faculty Recruiters on Wednesday, October 16, 2019 from 3:30P
MEET THE FACULTY CANDIDATES Candidates will be present to meet with faculty recruiters on Wednesday, October 16, 2019 from 3:30pm – 5:30pm in Exhibit Hall DE. Admission to the Poster Forum (other than candidates below) are by a business card showing that the individual is a faculty recruiter and a valid BMES Annual Meeting badge. AMR ASHRAF ABDEEN, PhD Wisconsin Institute for Discovery, University of Wisconsin, Madison, WI . [email protected] Research Overview: My interests lie at a unique intersection of biomaterials and mechanobiology, genomics and stem cell therapies. I aim to advance the analysis of biomaterial-cell interaction, fundamental mechanobiology and biomaterials-based therapeutics using novel genome engineering methods in the biomaterials field. My doctoral work focused on the use of biomaterials to probe cell-matrix interaction – how cell matrix affects their differentiation and secretory profile for therapeutic purposes. My postdoctoral work focuses on the more translational usage of biomaterials for therapies. Here, I’ve worked on protein delivery for genome editing, had exposure to state -of the-art regenerative stem cell therapies (for in vivo implantation) and immunotherapies (such as CAR-T therapies). In addition, I now have extensive experience in CRISPR-based genome manipulation for fundamental studies as well as therapeutic purposes. This work involved learning more sophisticated, high-throughput molecular biology assays. One focus of my lab will be studying the more fundamental biomaterials-cell interactions using unbiased biological methods such as high throughput sequencing or functional screens, coupled with a library of biomaterials that covers a wide range of materials properties. Another focus will be the m ore translational aspect of therapeutics, with a focus on delivery techniques for both gene and cell therapies. -

Kristi S. Anseth
KRISTI S. ANSETH Department of Chemical and Biological Engineering and the BioFrontiers Institute University of Colorado at Boulder 3415 Colorado Avenue, JSCBB UCB 596 Boulder, Colorado 80303-0596 phone: (303) 492-3147 fax: (303) 492-4341 e-mail: [email protected] Website: www.colorado.edu/ansethgroup/ EDUCATION Ph.D. in Chemical Engineering, University of Colorado, December 1994. B.S. in Chemical Engineering (with Highest Distinction), Purdue University, May 1992. PROFESSIONAL EXPERIENCE Distinguished Professor. Chemical and Biological Engineering, University of Colorado, Boulder, Jan. 2008 to present Howard Hughes Medical Institute Investigator. Sept. 2005 to August 2017 Tisone Professor. Chemical and Biological Engineering, University of Colorado, Boulder, Sept. 2003 to present Associate Faculty Director. BioFrontiers Institute, University of Colorado, Boulder, Nov. 2003 to present Professor (by courtesy). Craniofacial Biology, School of Dentistry, University of Colorado Health Sciences Center, Denver, Sept. 2005 to present Professor (by courtesy). Chemistry and Biochemistry, University of Colorado, Boulder, Mar. 2004 to present Professor (by courtesy). Molecular, Cellular and Developmental Biology, University of Colorado, Boulder, Mar. 2004 to present Professor. Chemical Engineering, University of Colorado, Boulder. Aug. 2002 to Aug. 2003 Patten Associate Professor. Chemical Engineering, University of Colorado, Boulder. Aug. 1999 to July 2002 Howard Hughes Medical Institute Assistant Investigator. Aug. 2000 to Aug. 2005 Associate Professor. Surgery, University of Colorado Health Sciences Center, Denver. Aug. 2000 to present Patten Assistant Professor. Chemical Engineering, University of Colorado, Boulder. Sept. 1998 to July 1999 Assistant Professor. Chemical Engineering, University of Colorado, Boulder. Aug. 1996 to Aug. 1998 Research Fellow. Dr. Robert Langer, mentor. MIT, Cambridge, MA. Sept. -

Adrianne M. Rosales Assistant Professor CPE 3.418 Email: [email protected]
Adrianne M. Rosales Assistant Professor CPE 3.418 email: [email protected] EDUCATION Ph.D. Chemical Engineering, May 2013 University of California, Berkeley – Berkeley, CA Advisor: Professor Rachel A. Segalman Dissertation: “Nanostructure Control of Biologically Inspired Polymers” B.S. Chemical Engineering, May 2007 The University of Texas at Austin – Austin, TX Graduated magna cum laude RESEARCH & WORK EXPERIENCE Postdoctoral Fellow 07/2013 - present Department of Chemical and Biological Engineering, University of Colorado, Boulder Lab of Professor Kristi Anseth Visiting Scholar in lab of Jason Burdick, University of Pennsylvania (09/2014 - present) Graduate Research Assistant 08/2007 – 05/2013 Department of Chemical & Biomolecular Engineering, University of California, Berkeley Labs of Professor Rachel A. Segalman & Dr. Ronald N. Zuckermann (LBNL) Undergraduate Research Assistant 01/2005 – 05/2007 Department of Chemical Engineering, University of Texas at Austin Lab of Professor Nicholas A. Peppas Polypropylene Licensing& Catalyst Intern 05/2006 – 08/2006 Dow Chemical Company – South Charleston, WV Beauty Care R&D Intern 06/2005 – 08/2005 Procter & Gamble – Cincinnati, OH FELLOWSHIPS AND AWARDS 2015 University of Washington Distinguished Young Scholars Seminar series – co-winner 2015 Best Paper, Biomaterials session, 2014 AIChE National Meeting 2014 NIH Ruth L. Kirschstein NRSA F32 Postdoctoral Fellowship 2014 American Heart Association Postdoctoral Fellowship (declined to accept NIH F32) 2014 Burroughs Wellcome Fund Postdoctoral Enrichment Program Award 2012 University of California Dissertation Year Fellowship 2012 Carl Storm Underrepresented Minority Fellowship (2012 Bioinspired Materials GRC) 2007 National Science Foundation Graduate Fellowship 2007 University of California, Berkeley, Chancellor’s Fellowship 2006 Dow Outstanding Junior Award (University of Texas at Austin) 2005 ConocoPhillips SPIRIT Scholars Program (University of Texas at Austin) 2003 National Hispanic Scholar Finalist Scholarship 2003 Robert C.