Restoration of Forearm Supination by Combining Pronator Teres with Allogeneic Tendon
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Median Nerve Compression at Pronator Teres
1 Median Nerve Compression at Pronator Teres Surgical Indications and Considerations Anatomical Considerations: The median nerve and brachial artery travel together down the arm. Therefore, one must be very careful not to interfere with either the median nerve or the brachial artery, especially when conducting surgical procedures. In the area of the pronator teres, there are many tendons as well. It is important to identify, as much as possible, the correct site of compression. Pathogenesis: The median nerve can get entrapped or compressed by several structures in the arm. The pronator teres muscle is the most common. Others entrapment sites include the flexor digitorum superficialis arch, the lacertus fibrosis (bicipital aponeurosis), and ligament of Struthers (frequency occurs in that order). For compression of the median nerve at the pronator teres and flexor digitorum superficialis, the cause is almost always due to hypertrophy of the respected muscle. This hypertrophy is from quick, forceful and repeated movements to the involved muscle. Examples include a carpenter or a baseball batter. As the muscle hypertrophies, the signal from the median nerve is diminished resulting in paresthesias in the median nerve distribution (lateral arm and hand) distal to the site of compression. Pain in the volar part of the forearm, often aggravated by repetitive supination and pronation, is a common symptom of pronator involvement. Another indicator is forearm pain with the compression of muscle such as pain in the volar part of the forearm implicating pronator teres. Onset is typically insidious and diagnosis is usually delayed 9 months to 2 years. Epidemiology: Pronator teres syndrome is the second most common cause of median nerve compression behind carpal tunnel syndrome. -

Early Passive Motion After Surgery
www.western -ortho.com www.denvershoulder.com Early Passive Motion after Shoulder Surgery Passive motion involves someone else moving the affected arm through the motion described. Or, in the case of elbow flexion/extension, you can use your opposite (non-affected arm) to move through the motion. Do 5 repetitions of each stretch 3 times per day. When you feel a slight ‘tightness’ with your arm in the position diagrammed, hold that position for 30 seconds. If lying down is difficult, the stretches can be done while seated. Shoulder Flexion Support arm at the wrist and elbow. With the thumb pointed forward, gently bring the arm up and forward then back to the side. Shoulder Abduction Support arm at wrist and elbow. With the thumb pointed away from the body and palm up, gently bring the arm out to the side. www.western -ortho.com www.denvershoulder.com Shoulder Internal/External Rotation Support arm at wrist and elbow. With the elbow at the side and bent to a 90 degree angle, gently rotate the hand away from the body down toward the table the individual is lying on. Elbow Flexion/Extension Forearm Pronation/Supination Grasp the wrist of your affected arm with your unaffected With your elbow and forearm supported on a table, hand. With your affected elbow against your side and your gently turn forearm so your palm is down, then turn palm up, gently bend and straighten your elbow. forearm so your palm is up. This can be done actively (without assistance from your other hand). . -

Pronator Syndrome: Clinical and Electrophysiological Features in Seven Cases
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.39.5.461 on 1 May 1976. Downloaded from Journal ofNeurology, Neurosurgery, and Psychiatry, 1976, 39, 461-464 Pronator syndrome: clinical and electrophysiological features in seven cases HAROLD H. MORRIS AND BRUCE H. PETERS From the Department ofNeurology, University of Texas Medical Branch, Galveston, Texas, USA SYNOPSIS The clinical and electrophysiological picture of seven patients with the pronator syndrome is contrasted with other causes ofmedian nerve neuropathy. In general, these patients have tenderness over the pronator teres and weakness of flexor pollicis longus as well as abductor pollicis brevis. Conduction velocity of the median nerve in the proximal forearm is usually slow but the distal latency and sensory nerve action potential at the wrist are normal. Injection of corticosteroids into the pronator teres has produced relief of symptoms in a majority of patients. Protected by copyright. In the majority of isolated median nerve dys- period 101 cases of the carpal tunnel syndrome functions the carpal tunnel syndrome is appropri- and the seven cases of the pronator syndrome ately first suspected. The median nerve can also reported here were identified. Median nerve be entrapped in the forearm giving rise to a conduction velocity determinations were made on similar picture and an erroneous diagnosis. all of these patients. The purpose of this report is to draw full attention to the pronator syndrome and to the REPORT OF CASES features which allow it to be distinguished from Table 1 provides clinical details of seven cases of the median nerve entrapment at other sites. -

Self Range of Motion Exercises for Arm and Hand
Self-Range of Motion Exercises for the Arm and Hand After a stroke, it is important to do the exercises in this handout for your affected arm and hand. You can do them on your own by using your unaffected arm and hand. These gentle movements are called “self-range of motion” exercises, and they help to maintain your movement, prevent stiffness, improve blood flow, and increase awareness of your affected arm and hand. Complete the exercises slowly and do not force movements. Stop if you feel pain. If you have any questions or concerns, please contact your Occupational Therapist: _______________________________ Do the exercises in this handout _____ times each day. Page - 1 Self-range of motion exercises for the arm and hand 1. Shoulder: Forward Arm Lift Interlock your fingers, or hold your wrist. With your elbows straight and thumbs facing the ceiling, lift your arms to shoulder height. Slowly lower your arms to starting position. Hold for ____ seconds. Repeat ____ times. Page - 2 Self-range of motion exercises for the arm and hand 2. Shoulder: “Rock the Baby” Stretch Hold your affected arm by supporting the elbow, forearm and wrist (as if cradling a baby). Slowly move your arms to the side, away from your body, lifting to shoulder height. Repeat this motion in the other direction. Slowly rock your arms side-to-side, and keep your body from turning. Repeat ____ times. Page - 3 Self-range of motion exercises for the arm and hand 3. Shoulder: Rotation Stretch Interlock your fingers, or hold your wrist. With your elbows bent at 90 degrees, keep your affected arm at your side. -

Morphological Study of Palmaris Longus Muscle
International INTERNATIONAL ARCHIVES OF MEDICINE 2017 Medical Society SECTION: HUMAN ANATOMY Vol. 10 No. 215 http://imedicalsociety.org ISSN: 1755-7682 doi: 10.3823/2485 Humberto Ferreira Morphological Study of Palmaris Arquez1 Longus Muscle ORIGINAL 1 University of Cartagena. University St. Thomas. Professor Human Morphology, Medicine Program, University of Pamplona. Morphology Laboratory Abstract Coordinator, University of Pamplona. Background: The palmaris longus is one of the most variable muscle Contact information: in the human body, this variations are important not only for the ana- tomist but also radiologist, orthopaedic, plastic surgeons, clinicians, Humberto Ferreira Arquez. therapists. In view of this significance is performed this study with Address: University Campus. Kilometer the purpose to determine the morphological variations of palmaris 1. Via Bucaramanga. Norte de Santander, longus muscle. Colombia. Suramérica. Tel: 75685667-3124379606. Methods and Findings: A total of 17 cadavers with different age groups were used for this study. The upper limbs region (34 [email protected] sides) were dissected carefully and photographed in the Morphology Laboratory at the University of Pamplona. Of the 34 limbs studied, 30 showed normal morphology of the palmaris longus muscle (PL) (88.2%); PL was absent in 3 subjects (8.85% of all examined fo- rearm). Unilateral absence was found in 1 male subject (2.95% of all examined forearm); bilateral agenesis was found in 2 female subjects (5.9% of all examined forearm). Duplicated palmaris longus muscle was found in 1 male subject (2.95 % of all examined forearm). The palmaris longus muscle was innervated by branches of the median nerve. The accessory palmaris longus muscle was supplied by the deep branch of the ulnar nerve. -

Muscles of the Upper Limb.Pdf
11/8/2012 Muscles Stabilizing Pectoral Girdle Muscles of the Upper Limb Pectoralis minor ORIGIN: INNERVATION: anterior surface of pectoral nerves ribs 3 – 5 ACTION: INSERTION: protracts / depresses scapula coracoid process (scapula) (Anterior view) Muscles Stabilizing Pectoral Girdle Muscles Stabilizing Pectoral Girdle Serratus anterior Subclavius ORIGIN: INNERVATION: ORIGIN: INNERVATION: ribs 1 - 8 long thoracic nerve rib 1 ---------------- INSERTION: ACTION: INSERTION: ACTION: medial border of scapula rotates scapula laterally inferior surface of scapula stabilizes / depresses pectoral girdle (Lateral view) (anterior view) Muscles Stabilizing Pectoral Girdle Muscles Stabilizing Pectoral Girdle Trapezius Levator scapulae ORIGIN: INNERVATION: ORIGIN: INNERVATION: occipital bone / spinous accessory nerve transverse processes of C1 – C4 dorsal scapular nerve processes of C7 – T12 ACTION: INSERTION: ACTION: INSERTION: stabilizes / elevates / retracts / upper medial border of scapula elevates / adducts scapula acromion / spine of scapula; rotates scapula lateral third of clavicle (Posterior view) (Posterior view) 1 11/8/2012 Muscles Stabilizing Pectoral Girdle Muscles Moving Arm Rhomboids Pectoralis major (major / minor) ORIGIN: INNERVATION: ORIGIN: INNERVATION: spinous processes of C7 – T5 dorsal scapular nerve sternum / clavicle / ribs 1 – 6 dorsal scapular nerve INSERTION: ACTION: INSERTION: ACTION: medial border of scapula adducts / rotates scapula intertubucular sulcus / greater tubercle flexes / medially rotates / (humerus) adducts -
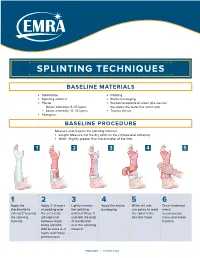
Splinting Techniques
SPLINTING TECHNIQUES BASELINE MATERIALS l Stockinette l Padding l Splinting material l Elastic bandaging l Plaster l Bucket/receptacle of water (the warmer — Upper extremity: 8–10 layers the water, the faster the splint sets) — Lower extremity: 10–12 layers l Trauma shears l Fiberglass BASELINE PROCEDURE Measure and prepare the splinting material. l Length: Measure out the dry splint on the contralateral extremity l Width: Slightly greater than the diameter of the limb 1 2 3 4 5 1 2 3 4 5 6 Apply the Apply 2–3 layers Lightly moisten Apply the elastic While still wet, Once hardened, stockinette to of padding over the splinting bandaging. use palms to mold check extend 2" beyond the area to be material. Place it the splint to the neruovascular the splinting splinted and and fold the ends desired shape. status and motor material. between digits of stockinette function. being splinted. over the splinting Add an extra 2–3 material. layers over bony prominences. EMRA.ORG | 972.550.0920 POSTERIOR LONG ARM VOLAR SPLINT SPLINT INDICATIONS INDICATIONS l Olecranon fractures l Soft tissue injuries of the hand and wrist l Humerus fractures l Carpal bone fractures l Radial head and neck fractures l 2nd–5th metacarpal head fractures CONSTRUCTION CONSTRUCTION l Start at posterior proximal arm l Start at palm at the metacarpal heads l Down the ulnar forearm l Down the volar forearm l End at the metacarpophalangeal joints l End at distal forearm APPLICATION APPLICATION l Cut hole in stockinette for thumb l Cut hole in stockinette for thumb l Elbow at 90º -

The Impact of Palmaris Longus Muscle on Function in Sports: an Explorative Study in Elite Tennis Players and Recreational Athletes
Journal of Functional Morphology and Kinesiology Article The Impact of Palmaris Longus Muscle on Function in Sports: An Explorative Study in Elite Tennis Players and Recreational Athletes Julie Vercruyssen 1,*, Aldo Scafoglieri 2 and Erik Cattrysse 2 1 Faculty of Physical Education and Physiotherapy, Master of Science in Manual therapy, Vrije Universiteit Brussel, Laarbeeklaan 103, 1090 Brussels, Belgium 2 Faculty of Physical Education and Physiotherapy, Department of Experimental Anatomy, Vrije Universiteit Brussel, Laarbeeklaan 103, 1090 Brussels, Belgium; [email protected] (A.S.); [email protected] (E.C.) * Correspondence: [email protected]; Tel.: +32-472-741-808 Academic Editor: Giuseppe Musumeci Received: 21 February 2016; Accepted: 24 March 2016; Published: 13 April 2016 Abstract: The Palmaris longus muscle can be absent unilateral or bilateral in about 22.4% of human beings. The aim of this study is to investigate whether the presence of the Palmaris longus muscle is associated with an advantage to handgrip in elite tennis players compared to recreational athletes. Sixty people participated in this study, thirty elite tennis players and thirty recreational athletes. The presence of the Palmaris longus muscle was first assessed using different tests. Grip strength and fatigue resistance were measured by an electronic hand dynamometer. Proprioception was registered by the Flock of Birds electromagnetic tracking system. Three tests were set up for measuring proprioception: joint position sense, kinesthesia, and joint motion sense. Several hand movements were conducted with the aim to correctly reposition the joint angle. Results demonstrate a higher presence of the Palmaris longus muscle in elite tennis players, but this was not significant. -

Common Elbow Injuries Symptoms
During the summer months, many people stay active by playing golf or tennis. These sports, however, carry a risk of injury to the tendons – bands of tissue that connect muscles to bones – in the elbow. This month’s AT Corner will explain how these injuries happen, how to treat them if they occur and, most importantly, how to prevent them. Common Elbow Injuries Tendonitis: Inflammation, pain and difficulty using the joint caused by repetitive activities and/or sudden trauma. Tendonosis: A degeneration (breakdown) or tear of tendons which occurs as a result of aging. Symptoms of tendonosis usually last more than a few weeks. Note: Your risk of tendonitis and tendonosis increases with age. They also occur more frequently in those who routinely perform activities that require repetitive movement, as this places greater amounts of stress on the tendons. Tennis elbow: Also referred to as lateral epicondylitis, this condition occurs when there is an injury to the outer elbow tendon. Golfers’ elbow: Also referred to as medial epicondylitis, this condition occurs when there is an injury to the inner elbow tendon. Note: Injuries to these tendons can occur in other sports and activities that use the wrist and forearm muscles. Most times, the dominant arm is the one affected. Symptoms • Pain that spreads from the elbow into the upper arm or down the forearm • Forearm weakness • Pain that can begin suddenly or gradually worsen over time • Difficulty with activities that require arm strength Treatment Over-the-counter medications: NSAIDs, such as ibuprofen (Advil®, Motrin®) and naproxen (Aleve®), or acetaminophen (Tylenol®) can provide pain relief. -
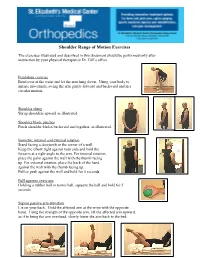
Shoulder Range of Motion Exercises
Shoulder Range of Motion Exercises The exercises illustrated and described in this document should be performed only after instruction by your physical therapist or Dr. Gill’s office. Pendulum exercise Bend over at the waist and let the arm hang down. Using your body to initiate movement, swing the arm gently forward and backward and in a circular motion. Shoulder shrug Shrug shoulders upward as illustrated. Shoulder blade pinches Pinch shoulder blades backward and together, as illustrated. Isometric internal and external rotation Stand facing a doorjamb or the corner of a wall. Keep the elbow tight against your side and hold the forearm at a right angle to the arm. For internal rotation, place the palm against the wall with the thumb facing up. For external rotation, place the back of the hand against the wall with the thumb facing up. Pull or push against the wall and hold for 5 seconds Ball squeeze exercises Holding a rubber ball or tennis ball, squeeze the ball and hold for 5 seconds Supine passive arm elevation Lie on your back. Hold the affected arm at the wrist with the opposite hand. Using the strength of the opposite arm, lift the affected arm upward, as if to bring the arm overhead, slowly lower the arm back to the bed. St. Elizabeth's Medical Center Orthopedics Department 736 Cambridge Street Brighton, MA 02135 www.semc.org/ortho Supine Passive Forward Flexion Lie on your back. Holding a stick in both hands about shoulder width apart, raise the involved arm with the help of the uninvolved arm up and then backward as if to reach overhead. -

Anatomical Study of Pronator Teres Muscle Innervation and Clinical Significance in Nerve Transfer
Int. J. Morphol., 36(4):1500-1508, 2018. Anatomical Study of Pronator Teres Muscle Innervation and Clinical Significance in Nerve Transfer Estudio Anatómico de la Inervación del Músculo Pronador Redondo y Significado Clínico en la Transferencia Nerviosa Edie Benedito Caetano1; Luiz Angelo Vieira1; José João Sabongi Neto2; Maurício Benedito Ferreira Caetano2; Rodrigo Guerra Sabongi3; Luca Martinez4; Kelson Koiti Ogata4 & Eduardo Baldy de Sousa Boni4 CAETANO, E. B.; VIEIRA, L A.; SABONGI NETO, J. J. ; CAETANO, M. B. F.; SABONGI, R. G.; MARTINEZ, L.; OGATA, K. K. & BONI, E. B. S. Anatomical study of pronator teres muscle innervation and clinical significance in nerve transfer. Int. J. Morphol., 36(4):1500-1508, 2018. SUMMARY: The anatomical relationship of the median nerve and its innervation pattern are variable and may have direct implications in surgical procedures such as distal nerve transfers. The objective of this study was to evaluate the anatomical variations of pronator teres muscle (PTM) innervation and its clinical significance in nerve transfers. Data were collected regarding the number of median nerve branches, site of their origin, contribution with branches of other muscles and the possibility of transferring expendable branches of PTM to the anterior interosseous nerve (AIN) and radial nerve. The most common origin of the branches was proximal to the humeral intercondylar line. The presence of only one PTM branch was identified in 9 limbs, in which 6 was exclusive for this muscle. The majority of specimens presented more than one branch to the PTM, with two branches in 19, although only 6 of these did not share branches with other muscles. -
Forearm Fractures Sean T
Forearm Fractures Sean T. Campbell, MD Assistant Attending Orthopedic Trauma Service Hospital for Special Surgery, New York, NY Core Curriculum V5 Objectives • Understand rationale for surgery for forearm fractures • Understand which segment is unstable based on injury pattern • Identify goals of surgery based on injury pattern • Review surgical techniques Core Curriculum V5 Introduction: Forearm Fractures • Young patients • Typically high energy injuries • Geriatric/osteopenic patients • May be low energy events • Mechanism • Fall on outstretched extremity • Direct blunt trauma Core Curriculum V5 Anatomy • Two bones that function as a forearm joint to allow rotation • Radius • Radial bow in coronal plane • Ulna • Proximal dorsal angulation in sagittal plane • Not a straight bone • Distinct bow in coronal plane (see next slides) • Proximal radioulnar joint (PRUJ) • Articulation of radial head with proximal ulna • Distal radioulnar joint • Articulation of ulnar head with distal radius • Interosseous membrane Hreha J+, Snow B+ Image from: Jarvie, Geoff C. MD, MHSc, FRCSC*; Kilb, Brett MD, MSc, BS*,†; Willing, Ryan PhD, BEng‡; King, Graham J. MD, MSc, FRCSC‡; Daneshvar, Parham MD, BS* Apparent Proximal Ulna Dorsal Angulation Variation Due to Ulnar Rotation, Journal of Orthopaedic Trauma: April 2019 - Volume 33 - Issue 4 - p e120-e123 doi: 10.1097/BOT.0000000000001408 Core Curriculum V5 Anatomy • Radial bow allows for pronosupination • Must be restored surgically when compromised • Multiple methods for assessment of radial bow • Comparison to contralateral images • Direct anatomic reduction of simple fractures • Biceps tuberosity 180 degrees of radial styloid • Note opposite apex medial bow of ulna • Not a straight bone Image from: Rockwood and Green, 9e, fig 41-9 Core Curriculum V5 Anatomy • Depiction of ulnar shape, noting proximal ulnar dorsal angulation (PUDA) in the top image, and varus angulation in the bottom image Image from: Jarvie, Geoff C.