A Review of Its Use for Conscious Sedation of Children
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Statement on Safe Use of Propofol 2019
Statement on Safe Use of Propofol Committee of Origin: Ambulatory Surgical Care (Approved by the ASA House of Delegates on October 27, 2004, and amended on October 23, 2019) Because sedation is a continuum, it is not always possible to predict how an individual patient will respond. Due to the potential for rapid, profound changes in sedative/anesthetic depth and the lack of antagonist medications, agents such as propofol require special attention. Even if moderate sedation is intended, patients receiving propofol should receive care consistent with that required for deep sedation. The Society believes that the involvement of an anesthesiologist in the care of every patient undergoing anesthesia is optimal. However, when this is not possible, non-anesthesia personnel who administer propofol should be qualified to rescue* patients whose level of sedation becomes deeper than initially intended and who enter, if briefly, a state of general anesthesia.** • The physician responsible for the use of sedation/anesthesia should have the education and training to manage the potential medical complications of sedation/anesthesia. The physician should be proficient in airway management, have advanced life support skills appropriate for the patient population, and understand the pharmacology of the drugs used. The physician should be physically present throughout the sedation and remain immediately available until the patient is medically discharged from the post procedure recovery area. • The practitioner administering propofol for sedation/anesthesia should, at a minimum, have the education and training to identify and manage the airway and cardiovascular changes which occur in a patient who enters a state of general anesthesia, as well as the ability to assist in the management of complications. -

Midazolam Injection, USP
Midazolam Injection, USP 2 mg per 2 mL | NDC 70860-600-02 50 mg per 10 mL | NDC 70860-601-10 ATHENEX AccuraSEETM PACKAGING AND LABELING BIG, BOLD AND BRIGHT — TO HELP YOU SEE IT, SAY IT AND PICK IT RIGHT DIFFERENTIATION IN EVERY LABEL, DESIGNED TO HELP REDUCE MEDICATION ERRORS PLEASE SEE FULL PRESCRIBING INFORMATION, INCLUDING BOXED WARNING, FOR MIDAZOLAM INJECTION, USP, ENCLOSED. THE NEXT GENERATION OF PHARMACY INNOVATION To order, call 1-855-273-0154 or visit www.Athenexpharma.com Midazolam Injection, USP 2 5 mg NDC 70860-600-02 0 NDC 70860-601-10 2 mg per 2 mL mg 50 mg per 10 mL DESCRIPTION Glass Vial DESCRIPTION Glass Vial CONCENTRATION 1 mg per mL CONCENTRATION 5 mg per mL CLOSURE 13 mm CLOSURE 20 mm UNIT OF SALE 25 vials UNIT OF SALE 10 vials BAR CODED Yes BAR CODED Yes STORAGE Room Temp. STORAGE Room Temp. • AP RATED • PRESERVATIVE-FREE • AP RATED • NOT MADE WITH NATURAL RUBBER LATEX • NOT MADE WITH NATURAL RUBBER LATEX CHOOSE AccuraSEETM FOR YOUR PHARMACY Our proprietary, differentiated and highly-visible label designs can assist pharmacists in accurate medication selection. With a unique label design for every Athenex product, we’re offering your pharmacy added AccuraSEE. The idea is simple: “So what you see is exactly what you get.” Athenex, AccuraSEE and all label designs are copyright of Athenex. ©2020 Athenex. 000527 To order, call 1-855-273-0154 or visit www.Athenexpharma.com • Midazolam hydrochloride mufti-dose vial, is not intended for intrathecal or epidural • Anesthetic and sedation drugs are a necessary part of the care of children needing Midazolam Injection, USP administration, and is contraindicated for use in premature infants, because the formulation surgery, other procedures, or tests that cannot be delayed, and no specific medications INDICATIONS AND USAGE contains benzyl alcohol as a preservative. -
Intravenous Sedation and Preparing for Your Procedure
Oral and Maxillofacial Surgery Intravenous sedation and preparing for your procedure Information for patients Please ensure that you read this leaflet before you come to hospital for your operation What is sedation? Sedation is a way of using drugs (sedatives) to make you feel relaxed and sleepy during your procedure. We will give you your sedatives through an injection into a vein. Sedation is not a general anaesthetic and you will not be unconscious. You may not remember much of what happens during the procedure and directly afterwards. This is quite normal. Local anaesthetic will be given once you have been sedated. Do not drive, operate machinery or sign important documents for at least 24 hours after your procedure. You must make sure that you have a responsible adult with you who can stay in the department for a couple of hours and take you home by car or taxi. Someone must also stay with you for at least 24 hours after your procedure. Your procedure will be cancelled if you do not bring someone with you who can do this. Preparation for your procedure and what to bring with you • Patients having a procedure under sedation must follow the current fasting guidelines for general anaesthesia. You must not eat or drink for 6 hours before your procedure but you may have water up to 2 hours before. If you do eat or drink after these times your surgery will be cancelled. • Avoid alcohol for 24 hours before your procedure. • Bring with you a list of any medication or drugs you are taking. -

Moderate Sedation Study Guide 11-17-10
PROCEDURE RELATED SEDATION Outline I Introduction II Definitions: The 5 Levels of Sedation and Anesthesia III Emergency Procedures, Critical Care Areas and Policy Exclusions IV The Pre-Sedation Assessment V NPO: The Timing of Eating and Drinking before Sedation VI Review of Some Agents Used for Sedation VII Orders for Procedure Related Sedation VIII Environmental Requirements and Monitoring During Sedation IX Post-Procedure Monitoring and the PAR Score X Discharge Criteria and Concluding Post-Procedure Monitoring 1 PROCEDURE RELATED SEDATION Lance Brown, MD, MPH I. Introduction The purpose of this tutorial is to familiarize the reader with the Loma Linda University Medical Center Policy M-86 for Procedure Related Sedation. Procedure related sedation is used to make necessary medical procedures as comfortable as possible for patients and to facilitate the performance of necessary medical procedures by health care providers (typically physicians). It is important for health care providers performing procedure related sedation to be familiar with the pharmacologic characteristics of the agents being used, to understand the risk factors for complications related to procedure related sedation, and to individually plan the sedation for each patient. Each health care practitioner privileged to provide procedure related sedation takes responsibility for both the comfort and safety of the patients in their care. II. Definitions At Loma Linda University Medical Center, we have defined five distinct levels of sedation and anesthesia. Familiarity with the definitions of these levels of sedation is important for safely providing procedure related sedation and for complying with the policy of the Medical Center. It must be recognized, however, that sedation occurs along a continuum and that individual patients may have different degrees of sedation for a given dose and route of medication. -

Post-Intubation Analgesia and Sedation
POST-INTUBATION ANALGESIA AND SEDATION August 2012 J Pelletier Intubated patients experience pain and anxiety Mechanical ventilation, endotracheal tube Blood draws, positioning, suctioning Surgical procedures, dressing changes Awareness during neuromuscular blockade Invasive catheters Loss of control Unrelieved pain and anxiety cause adverse effects Self-injury and removal of life-sustaining devices Increased endogenous catecholamines Sleep deprivation, anxiety, and delirium Impaired post-ICU psychological recovery Emotional and posttraumatic effects Ventilator dysynchrony Immunosuppression Treating pain and anxiety improves outcomes Use of pain and sedation scales in critically ill patients allows: precise dosing reduced medication side effects reduced ICU and hospital length of stay shorter duration of mechanical ventilation Analgesics should be provided first, then anxiolysis If you were intubated, how much lorazepam or midazolam, and fentanyl would you want per hour? Intubated ED patients receive inadequate analgesia and sedation Retrospective study, tertiary ED 50% received no analgesia, 30% received no anxiolytic Of patients receiving postintubation vecuronium, 96% received either no or inadequate anxiolysis or analgesia Overall, 3 of 4 patients received no or inadequate analgesia and an equivalent number received no or inadequate anxiolysis Bonomo 2007 Analgesia: opioids Bind CNS and peripheral tissue receptors Mu-1 receptors: analgesia Mu-2 receptors: respiratory depression, vomiting, constipation, and -

The Emergence of New Psychoactive Substance (NPS) Benzodiazepines
Issue: Ir Med J; Vol 112; No. 7; P970 The Emergence of New Psychoactive Substance (NPS) Benzodiazepines. A Survey of their Prevalence in Opioid Substitution Patients using LC-MS S. Mc Namara, S. Stokes, J. Nolan HSE National Drug Treatment Centre Abstract Benzodiazepines have a wide range of clinical uses being among the most commonly prescribed medicines globally. The EU Early Warning System on new psychoactive substances (NPS) has over recent years detected new illicit benzodiazepines in Europe’s drug market1. Additional reference standards were obtained and a multi-residue LC- MS method was developed to test for 31 benzodiazepines or metabolites in urine including some new benzodiazepines which have been classified as New Psychoactive Substances (NPS) which comprise a range of substances, including synthetic cannabinoids, opioids, cathinones and benzodiazepines not covered by international drug controls. 200 urine samples from patients attending the HSE National Drug Treatment Centre (NDTC) who are monitored on a regular basis for drug and alcohol use and which tested positive for benzodiazepine class drugs by immunoassay screening were subjected to confirmatory analysis to determine what Benzodiazepine drugs were present and to see if etizolam or other new benzodiazepines are being used in the addiction population currently. Benzodiazepine prescription and use is common in the addiction population. Of significance we found evidence of consumption of an illicit new psychoactive benzodiazepine, Etizolam. Introduction Benzodiazepines are useful in the short-term treatment of anxiety and insomnia, and in managing alcohol withdrawal. 1 According to the EMCDDA report on the misuse of benzodiazepines among high-risk opioid users in Europe1, benzodiazepines, especially when injected, can prolong the intensity and duration of opioid effects. -

The Waterloo Wellington Palliative Sedation Protocol
The Waterloo Wellington Palliative Sedation Protocol Waterloo Wellington Interdisciplinary HPC Education Committee; PST Task Force Chair: Dr. Deborah Robinson MD CCFP(F), Focused practice in Oncology and Palliative Care Co-chairs: Cathy Joy, Palliative Care Consultant, Waterloo Region Chris Bigelow, Palliative Care Consultant, Wellington County Revision due: November 2016 Last revised and activated: November 13, 2013 Committee responsible for revisions: WW Interdisciplinary HPC Education Committee Table of Contents Purpose and Definitions .................................................................................................................... 2 Indications for the use of PST .............................................................................................................. 3 Criteria for Initiation of PST ............................................................................................................... 4 Process ............................................................................................................................................. 4 Documentation for Initiation of PST .................................................................................................. 5 Medications ......................................................................................................................................... 6 1st Line (Initiating PST) ...................................................................................................................... 6 2nd Line (When 1st -

Midazolam Injection, USP
Midazolam Injection, USP Rx only PHARMACY BULK PACKAGE – NOT FOR DIRECT INFUSION WARNING ADULTS AND PEDIATRICS: Intravenous midazolam has been associated with respiratory depression and respiratory arrest, especially when used for sedation in noncritical care settings. In some cases, where this was not recognized promptly and treated effectively, death or hypoxic encephalopathy has resulted. Intravenous midazolam should be used only in hospital or ambulatory care settings, including physicians’ and dental offices, that provide for continuous monitoring of respiratory and cardiac function, i.e., pulse oximetry. Immediate availability of resuscitative drugs and age- and size-appropriate equipment for bag/valve/mask ventilation and intubation, and personnel trained in their use and skilled in airway management should be assured (see WARNINGS). For deeply sedated pediatric patients, a dedicated individual, other than the practitioner performing the procedure, should monitor the patient throughout the procedures. The initial intravenous dose for sedation in adult patients may be as little as 1 mg, but should not exceed 2.5 mg in a normal healthy adult. Lower doses are necessary for older (over 60 years) or debilitated patients and in patients receiving concomitant narcotics or other central nervous system (CNS) depressants. The initial dose and all subsequent doses should always be titrated slowly; administer over at least 2 minutes and 1 allow an additional 2 or more minutes to fully evaluate the sedative effect. The dilution of the 5 mg/mL formulation is recommended to facilitate slower injection. Doses of sedative medications in pediatric patients must be calculated on a mg/kg basis, and initial doses and all subsequent doses should always be titrated slowly. -

Tracheal Intubation Intubação Traqueal
0021-7557/07/83-02-Suppl/S83 Jornal de Pediatria Copyright © 2007 by Sociedade Brasileira de Pediatria ARTIGO DE REVISÃO Tracheal intubation Intubação traqueal Toshio Matsumoto1, Werther Brunow de Carvalho2 Resumo Abstract Objetivo: Revisar os conceitos atuais relacionados ao procedimento Objective: To review current concepts related to the procedure of de intubação traqueal na criança. tracheal intubation in children. Fontes dos dados: Seleção dos principais artigos nas bases de Sources: Relevant articles published from 1968 to 2006 were dados MEDLINE, LILACS e SciELO, utilizando as palavras-chave selected from the MEDLINE, LILACS and SciELO databases, using the intubation, tracheal intubation, child, rapid sequence intubation, keywords intubation, tracheal intubation, child, rapid sequence pediatric airway, durante o período de 1968 a 2006. intubation and pediatric airway. Síntese dos dados: O manuseio da via aérea na criança está Summary of the findings: Airway management in children is relacionado à sua fisiologia e anatomia, além de fatores específicos related to their physiology and anatomy, in addition to specific factors (condições patológicas inerentes, como malformações e condições (inherent pathological conditions, such as malformations or acquired adquiridas) que influenciam decisivamente no seu sucesso. As principais conditions) which have a decisive influence on success. Principal indicações são manter permeável a aérea e controlar a ventilação. A indications are in order to maintain the airway patent and to control laringoscopia e intubação traqueal determinam alterações ventilation. Laryngoscopy and tracheal intubation cause cardiovascular cardiovasculares e reatividade de vias aéreas. O uso de tubos com alterations and affect airway reactivity. The use of tubes with cuffs is not balonete não é proibitivo, desde que respeitado o tamanho adequado prohibited, as long as the correct size for the child is chosen. -

Comparison of Propofol Alone and in Combination with Ketamine Or
Clinical Research Article pISSN 2005-6419 • eISSN 2005-7563 KJA Comparison of propofol alone and Korean Journal of Anesthesiology in combination with ketamine or fentanyl for sedation in endoscopic ultrasonography Shweta A Singh1, Kelika Prakash1, Sandeep Sharma1, Gaurav Dhakate1, and Vikram Bhatia2 Departments of 1Anaesthesiology and Critical Care and 2Hepatology, Institute of Liver & Biliary Sciences, New Delhi, India Background: We evaluated whether the addition of a small dose of ketamine or fentanyl would lead to a reduction in the total dose of propofol consumed without compromising the safety and recovery of patients having endoscopic ultraso- nography (EUS). Methods: A total of 210 adult patients undergoing elective EUS under sedation were included in the study. Patients were randomized into three groups. Patients were premedicated intravenously with normal saline in group 1, 50 µg fentanyl in group 2, and 0.5 mg/kg ketamine in group 3. All patients received intravenous propofol for sedation. Propofol consump- tion in mg/kg/h was noted. The incidence of hypotension, bradycardia, desaturation, and coughing was noted. The time to achieve a Post Anesthesia Discharge Score (PADS) of 10 was also noted. Results: There were 68 patients in group 1, 70 in group 2, and 72 in group 3. The amount of propofol consumed was significantly higher in group 1 (9.25 [7.3–13.2]) than in group 2 (8.8 [6.8–12.2]) and group 3 (7.6 [5.7–9.8]). Patient he- modynamics and oxygenation were well maintained and comparable in all groups. The time to achieve a PADS of 10 was significantly higher in group 3 compared to the other two groups. -

Inhaled Methoxyflurane (Penthrox) Sedation for Third Molar Extraction
Australian Dental Journal The official journal of the Australian Dental Association Australian Dental Journal 2011; 56: 296–301 SCIENTIFIC ARTICLE doi: 10.1111/j.1834-7819.2011.01350.x Inhaled methoxyflurane (Penthroxâ) sedation for third molar extraction: a comparison to nitrous oxide sedation WA Abdullah,* SA Sheta,* NS Nooh* *Department of Oral and Maxillofacial Surgery, College of Dentistry, King Saud University, Riyadh, Saudi Arabia. Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Mansoura University, Mansoura, Dakahlia, Egypt. ABSTRACT Background: The aim of this study was to evaluate the use of inhaled methoxyflurane (PenthroxÒ) in the reduction of dental anxiety in patients undergoing mandibular third molar removal in a specialist surgical suite and compare it to the conventional nitrous oxide sedation. Methods: A prospective randomized, non-blinded crossover design study of 20 patients receiving two types of sedation for their third molar extraction who participated in 40 treatment sessions. At first appointment, a patient was randomly assigned to receive either nitrous oxide sedation or intermittent PenthroxÒ inhaler sedation, with the alternate regimen administered during the second appointment. Peri-procedural vital signs (heart rate and blood pressure) were recorded and any deviations from 20% from the baseline values, as well as any drop in oxygen saturation below 92% were documented. The Ramsay Sedation Scale (RSS) score was recorded every five minutes. Patient cooperation during the procedure, patients’ general opinion about the sedation technique, surgeon satisfaction and the occurrence of side effects were all recorded. After the second procedure, the patient was also asked if he or she had any preference of one sedation technique over the other. -
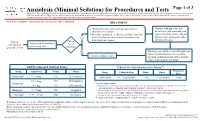
Anxiolysis (Minimal Sedation) for Procedures and Tests
Anxiolysis (Minimal Sedation) for Procedures and Tests Page 1 of 3 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. Note: Refer to UTMDACC Institutional Policy #CLN0502 for complete information. TREATMENT ● Document mental status and vital signs prior to Continue with procedure and administering sedation document mental status and vital ● Determine appropriate medication and dose based on signs after administering sedation onset of action (see chart below) of anxiolytic for and prior to beginning procedure Yes 1 desired patient response and post-procedure Patient Patient Assess need for anxiolysis scheduled for needs prior to procedure procedure or test anxiolysis? No Discharge patient when clinically stable and follow institutional processes regarding Continue with procedure discharge instructions and criteria for both inpatient and outpatient settings 2,3 Adult Recommended Anxiolysis Dosing Pediatric Recommended Anxiolysis Dosing3,5,6 Maximum Drug Adult Dose Route Onset Drug Pediatric Dose Route Onset Dose 4 Midazolam 5 – 10 mg PO 10-30 minutes Midazolam 0.5 – 1 mg/kg/dose PO 10-20 minutes 5 mg 0.5 – 2 mg PO 30-60 minutes Lorazepam 5 Pediatric considerations: 1 – 4 mg IM 20-30 minutes ● Consider lower dosing strategies for patients with cardiac or respiratory compromise, and those who received concomitant opiates, benzodiazepines or similar synergistic sedative medications.