The Pharmacology of Midazolam and Thiopental with Regard to the Lethal Injection Protocol in the State of Mississippi
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diazepam - Alcohol Withdrawal
Diazepam - alcohol withdrawal Why have I been prescribed diazepam? If a person stops drinking alcohol after a time of drinking too much they can experience withdrawal effects. These include “the shakes”, sweating, having fits, seeing things which are not there (hallucinations) and feeling anxious and low in mood. They can feel wound up and find it difficult to sleep. These withdrawal effects can be very uncomfortable and in extreme cases can be dangerous if they persist into “DTs” (delirium tremens). Diazepam is used to help reduce these withdrawal symptoms. It relieves anxiety and tension and aids sleep. Diazepam can also prevent fits. It controls the withdrawal symptoms until the body is free of alcohol and has settled down. This usually takes three to seven days from the time you stop drinking. What exactly is diazepam? Diazepam is a benzodiazepine. This group of medicines is also called anxiolytics or minor tranquillisers. Diazepam has many uses. It can be used to reduce symptoms of anxiety and insomnia, as well as to help people come off alcohol. Diazepam should only be prescribed and taken as a short course. Is diazepam safe to take? Diazepam is safe to take for a short period of time, but it doesn’t suit everyone. Below are a few conditions where diazepam may be less suitable. If any of these apply to you please tell your doctor or key-worker. If you have depression or a mental illness If you have lung disease or breathing problems, or suffer from liver or kidney trouble If you take any other medicines or drugs, including those on prescription and bought from a chemist If you take illicit drugs bought “on the street” If you are pregnant or breast-feeding What is the usual dose of diazepam? The dose of diazepam will usually be started at 10-20mg four times a day. -

Insomnia and Anxiety in Older People Sleeping Pills Are Usually Not the Best Solution
® Insomnia and anxiety in older people Sleeping pills are usually not the best solution lmost one-third of older people in the people who take one of United States take sleeping pills. These these medicines sleep medicines are also sometimes called only a little longer and A“sedative-hypnotics” or “tranquilizers.” They better than those who affect the brain and spinal cord. don’t take a medicine. Doctors prescribe some of these medicines Sleeping pills can for sleep problems. Some of these medicines have serious side effects. also can be used to treat other conditions, such All sedative-hypnotic medicines have special as anxiety or alcohol withdrawal. Sometimes, risks for older adults. Seniors are likely to be doctors also prescribe certain anti-depressants more sensitive to the medicines’ effects than for sleep, even though that’s not what they’re younger adults. And these medicines may designed to treat. stay in older people’s bodies longer. These Most older adults should first try to treat their medicines can cause confusion and memory insomnia without medicines. According to the problems that: American Geriatrics Society, there are safer and • Increase the risk of falls and hip fractures. better ways to improve sleep or reduce anxiety. These are common causes of hospital stays Here’s why: and death in older people. Sleeping pills may not help much. • Increase the risk of car accidents. Many ads say that sleeping pills help people get a full, restful night’s sleep. But studies show that this is not exactly true in real life. On average, The new “Z” medicines also have risks. -
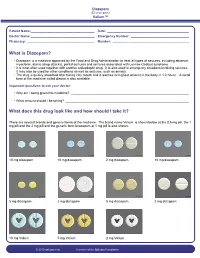
What Is Diazepam?
Diazepam (Di-a-ze-pam) Valium™ Patient Name: ___________________________________ Date: _____________________________________________ Doctor Name: ___________________________________ Emergency Number: ________________________________ Pharmacy: _____________________________________ Number: __________________________________________ What is Diazepam? • Diazepam is a medicine approved by the Food and Drug Administration to treat all types of seizures, including absence, myoclonic, atonic (drop attacks), partial seizures and seizures associated with Lennox-Gastaut syndrome. • It is most often used together with another antiepileptic drug. It is also used in emergency situations involving seizures. It may also be used for other conditions as well as seizures, such as anxiety. • The drug is quickly absorbed after taking it by mouth and it reaches its highest amount in the body in 1-2 hours. A rectal form of the medicine called diastat is also available. Important questions to ask your doctor: • Why am I being given this medicine? _________________________________________________________________ • What amount should I be taking? ____________________________________________________________________ What does this drug look like and how should I take it? There are several brands and generic forms of the medicine. The brand name Valium is shown below at the 0.5 mg pill, the 1 mg pill and the 2 mg pill and the generic form lorazepam at 1 mg pill is also shown. 10 mg diazepam 10 mg diazepam 2 mg diazepam 10 mg diazepam 5 mg diazepam 2 mg diazepam 5 mg diazepam 2 mg diazepam 10 mg Valium 5 mg Valium 2 mg Valium © 2010 epilepsy.com A service of the Epilepsy Foundation Diazepam (Di-a-ze-pam) Valium™ Frequently Asked Questions: How do I take Diazepam? To use the tablet form: chew tablets and swallow or swallow the tablet whole. -

Management of Status Epilepticus
Published online: 2019-11-21 THIEME Review Article 267 Management of Status Epilepticus Ritesh Lamsal1 Navindra R. Bista1 1Department of Anaesthesiology, Tribhuvan University Teaching Address for correspondence Ritesh Lamsal, MD, DM, Department Hospital, Institute of Medicine, Tribhuvan University, Nepal of Anaesthesiology, Tribhuvan University Teaching Hospital, Institute of Medicine, Tribhuvan University,Kathmandu, Nepal (e-mail: [email protected]). J Neuroanaesthesiol Crit Care 2019;6:267–274 Abstract Status epilepticus (SE) is a life-threatening neurologic condition that requires imme- diate assessment and intervention. Over the past few decades, the duration of seizure Keywords required to define status epilepticus has shortened, reflecting the need to start thera- ► convulsive status py without the slightest delay. The focus of this review is on the management of con- epilepticus vulsive and nonconvulsive status epilepticus in critically ill patients. Initial treatment ► neurocritical care of both forms of status epilepticus includes immediate assessment and stabilization, ► nonconvulsive status and administration of rapidly acting benzodiazepine therapy followed by nonbenzodi- epilepticus azepine antiepileptic drug. Refractory and super-refractory status epilepticus (RSE and ► refractory status SRSE) pose a lot of therapeutic problems, necessitating the administration of contin- epilepticus uous infusion of high doses of anesthetic agents, and carry a high risk of debilitating ► status epilepticus morbidity as well as mortality. ► super-refractory sta- tus epilepticus Introduction occur after 30 minutes of seizure activity. However, this working definition did not indicate the need to immediately Status epilepticus (SE) is a medical and neurologic emergency commence treatment and that permanent neuronal injury that requires immediate evaluation and treatment. It is associat- could occur by the time a clinical diagnosis of SE was made. -

Risk Based Requirements for Medicines Handling
Risk based requirements for medicines handling Including requirements for Schedule 4 Restricted medicines Contents 1. Introduction 2 2. Summary of roles and responsibilities 3 3. Schedule 4 Restricted medicines 4 4. Medicines acquisition 4 5. Storage of medicines, including control of access to storage 4 5.1. Staff access to medicines storage areas 5 5.2. Storage of S4R medicines 5 5.3. Storage of S4R medicines for medical emergencies 6 5.4. Access to storage for S4R and S8 medicines 6 5.5. Pharmacy Department access, including after hours 7 5.6. After-hours access to S8 medicines in the Pharmacy Department 7 5.7. Storage of nitrous oxide 8 5.8. Management of patients’ own medicines 8 6. Distribution of medicines 9 6.1. Distribution outside Pharmacy Department operating hours 10 6.2. Distribution of S4R and S8 medicines 10 7. Administration of medicines to patients 11 7.1. Self-administration of scheduled medicines by patients 11 7.2. Administration of S8 medicines 11 8. Supply of medicines to patients 12 8.1. Supply of scheduled medicines to patients by health professionals other than pharmacists 12 9. Record keeping 13 9.1. General record keeping requirements for S4R medicines 13 9.2. Management of the distribution and archiving of S8 registers 14 9.3. Inventories of S4R medicines 14 9.4. Inventories of S8 medicines 15 10. Destruction and discards of S4R and S8 medicines 15 11. Management of oral liquid S4R and S8 medicines 16 12. Cannabis based products 17 13. Management of opioid pharmacotherapy 18 14. -

GABA Receptors
D Reviews • BIOTREND Reviews • BIOTREND Reviews • BIOTREND Reviews • BIOTREND Reviews Review No.7 / 1-2011 GABA receptors Wolfgang Froestl , CNS & Chemistry Expert, AC Immune SA, PSE Building B - EPFL, CH-1015 Lausanne, Phone: +41 21 693 91 43, FAX: +41 21 693 91 20, E-mail: [email protected] GABA Activation of the GABA A receptor leads to an influx of chloride GABA ( -aminobutyric acid; Figure 1) is the most important and ions and to a hyperpolarization of the membrane. 16 subunits with γ most abundant inhibitory neurotransmitter in the mammalian molecular weights between 50 and 65 kD have been identified brain 1,2 , where it was first discovered in 1950 3-5 . It is a small achiral so far, 6 subunits, 3 subunits, 3 subunits, and the , , α β γ δ ε θ molecule with molecular weight of 103 g/mol and high water solu - and subunits 8,9 . π bility. At 25°C one gram of water can dissolve 1.3 grams of GABA. 2 Such a hydrophilic molecule (log P = -2.13, PSA = 63.3 Å ) cannot In the meantime all GABA A receptor binding sites have been eluci - cross the blood brain barrier. It is produced in the brain by decarb- dated in great detail. The GABA site is located at the interface oxylation of L-glutamic acid by the enzyme glutamic acid decarb- between and subunits. Benzodiazepines interact with subunit α β oxylase (GAD, EC 4.1.1.15). It is a neutral amino acid with pK = combinations ( ) ( ) , which is the most abundant combi - 1 α1 2 β2 2 γ2 4.23 and pK = 10.43. -

Dynamic Regulation of the GABAA Receptor Function by Redox Mechanisms S
Supplemental material to this article can be found at: http://molpharm.aspetjournals.org/content/suppl/2016/07/20/mol.116.105205.DC1 1521-0111/90/3/326–333$25.00 http://dx.doi.org/10.1124/mol.116.105205 MOLECULAR PHARMACOLOGY Mol Pharmacol 90:326–333, September 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics MINIREVIEW—A LATIN AMERICAN PERSPECTIVE ON ION CHANNELS Dynamic Regulation of the GABAA Receptor Function by Redox Mechanisms s Daniel J. Calvo and Andrea N. Beltrán González Laboratorio de Neurobiología Celular y Molecular, Instituto de Investigaciones en Ingeniería Genética y Biología Molecular Downloaded from ¨Dr. Héctor N. Torres¨ (INGEBI), Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET), Ciudad Autónoma de Buenos Aires, Argentina (D.J.C., A.N.B.G.) Received May 15, 2016; accepted July 14, 2016 ABSTRACT molpharm.aspetjournals.org Oxidizing and reducing agents, which are currently involved normally present in neurons and glia or are endogenously in cell metabolism and signaling pathways, can regulate fast generated in these cells under physiologic states or during inhibitory neurotransmission mediated by GABA receptors in the oxidative stress (e.g., hydrogen peroxide, superoxide and hy- nervous system. A number of in vitro studies have shown that droxyl radicals, nitric oxide, ascorbic acid, and glutathione), diverse redox compounds, including redox metabolites and induce potentiating or inhibiting actions on different native and reactive oxygen and nitrogen species, modulate phasic and recombinant GABAA receptor subtypes. Based on these results, it tonic responses mediated by neuronal GABAA receptors through is thought that redox signaling might represent a homeostatic both presynaptic and postsynaptic mechanisms. -

Benzodiazepines
Benzodiazepines Using benzodiazepines in Children and Adolescents Overview Benzodiazepines are group of medications used to treat several different conditions. Some examples of these medications include: lorazepam (Ativan®); clonazepam (Rivotril®); alprazolam (Xanax®) and oxazepam (Serax®). Other benzodiazepine medications are available, but are less commonly used in children and adolescents. What are benzodiazepines used for? Benzodiazepines may be used for the following conditions: • anxiety disorders: generalized anxiety disorder; social anxiety disorder; post-traumatic stress disorder (PTSD); panic attacks/disorder; excessive anxiety prior to surgery • sleep disorders: trouble sleeping (insomnia); waking up suddenly with great fear (night terrors); sleepwalking • seizure disorders (epilepsy) • alcohol withdrawal • treatment of periods of extreme slowing or excessive purposeless motor activity (catatonia) Your doctor may be using this medication for another reason. If you are unclear why this medication is being prescribed, please ask your doctor. How do benzodiazepines work? Benzodiazepines works by affecting the activity of the brain chemical (neurotransmitter) called GABA. By enhancing the action of GABA, benzodiazepines have a calming effect on parts of the brain that are too excitable. This in turn helps to manage anxiety, insomnia, and seizure disorders. How well do benzodiazepines work in children and adolescents? When used to treat anxiety disorders, benzodiazepines decrease symptoms such as nervousness, fear, and excessive worrying. Benzodiazepines may also help with the physical symptoms of anxiety, including fast or strong heart beat, trouble breathing, dizziness, shakiness, sweating, and restlessness. Typically, benzodiazepines are prescribed to manage anxiety symptoms that are uncomfortable, frightening or interfere with daily activities for a short period of time before conventional anti-anxiety treatments like cognitive-behavioural therapy or anti-anxiety takes effect. -

Midazolam Injection, USP
Midazolam Injection, USP 2 mg per 2 mL | NDC 70860-600-02 50 mg per 10 mL | NDC 70860-601-10 ATHENEX AccuraSEETM PACKAGING AND LABELING BIG, BOLD AND BRIGHT — TO HELP YOU SEE IT, SAY IT AND PICK IT RIGHT DIFFERENTIATION IN EVERY LABEL, DESIGNED TO HELP REDUCE MEDICATION ERRORS PLEASE SEE FULL PRESCRIBING INFORMATION, INCLUDING BOXED WARNING, FOR MIDAZOLAM INJECTION, USP, ENCLOSED. THE NEXT GENERATION OF PHARMACY INNOVATION To order, call 1-855-273-0154 or visit www.Athenexpharma.com Midazolam Injection, USP 2 5 mg NDC 70860-600-02 0 NDC 70860-601-10 2 mg per 2 mL mg 50 mg per 10 mL DESCRIPTION Glass Vial DESCRIPTION Glass Vial CONCENTRATION 1 mg per mL CONCENTRATION 5 mg per mL CLOSURE 13 mm CLOSURE 20 mm UNIT OF SALE 25 vials UNIT OF SALE 10 vials BAR CODED Yes BAR CODED Yes STORAGE Room Temp. STORAGE Room Temp. • AP RATED • PRESERVATIVE-FREE • AP RATED • NOT MADE WITH NATURAL RUBBER LATEX • NOT MADE WITH NATURAL RUBBER LATEX CHOOSE AccuraSEETM FOR YOUR PHARMACY Our proprietary, differentiated and highly-visible label designs can assist pharmacists in accurate medication selection. With a unique label design for every Athenex product, we’re offering your pharmacy added AccuraSEE. The idea is simple: “So what you see is exactly what you get.” Athenex, AccuraSEE and all label designs are copyright of Athenex. ©2020 Athenex. 000527 To order, call 1-855-273-0154 or visit www.Athenexpharma.com • Midazolam hydrochloride mufti-dose vial, is not intended for intrathecal or epidural • Anesthetic and sedation drugs are a necessary part of the care of children needing Midazolam Injection, USP administration, and is contraindicated for use in premature infants, because the formulation surgery, other procedures, or tests that cannot be delayed, and no specific medications INDICATIONS AND USAGE contains benzyl alcohol as a preservative. -

Determination of Barbiturates and 11-Nor-9-Carboxy-Δ9-THC in Urine
Determination of Barbiturates and 11-Nor-9-carboxy- 9-THC in Urine using Automated Disposable Pipette Extraction (DPX) and LC/MS/MS Fred D. Foster, Oscar G. Cabrices, John R. Stuff, Edward A. Pfannkoch GERSTEL, Inc., 701 Digital Dr. Suite J, Linthicum, MD 21090, USA William E. Brewer Department of Chemistry and Biochemistry, University of South Carolina, 631 Sumter St. Columbia, SC 29208, USA KEYWORDS DPX, LC/MS/MS, Sample Preparation, High Throughput Lab Automation ABSTRACT This work demonstrates the use of disposable pipette extraction (DPX) as a fast and automated sample preparation technique for the determination of barbiturates and 11-nor-9- carboxy- 9-THC (COOH-THC) in urine. Using a GERSTEL MultiPurpose Sampler (MPS) with DPX option coupled to an Agilent 6460 LC-MS/MS instrument, 8 barbiturates and COOH-THC were extracted and their concentrations determined. The resulting average cycle time of 7 min/ sample, including just-in-time sample preparation, enabled high throughput screening. Validation results show that the automated DPX-LC/ AppNote 1/2013 MS/MS screening method provides adequate sensitivity for all analytes and corresponding internal standards that were monitored. Lower limits of quantitation (LLOQ) were found to be 100 ng/mL for the barbiturates and 10 ng/mL for COOH-THC and % CVs were below 10 % in most cases. INTRODUCTION The continuously growing quantity of pain management sample extract for injection [1-2]. The extraction of the drugs used has increased the demand from toxicology Barbiturates and COOH-THC is based on the DPX-RP- laboratories for more reliable solutions to monitor S extraction method described in an earlier Application compliance in connection with substance abuse and/or Note detailing monitoring of 49 Pain Management diversion. -

Central Intelligence Agency (CIA) Freedom of Information Act (FOIA) Case Log October 2000 - April 2002
Description of document: Central Intelligence Agency (CIA) Freedom of Information Act (FOIA) Case Log October 2000 - April 2002 Requested date: 2002 Release date: 2003 Posted date: 08-February-2021 Source of document: Information and Privacy Coordinator Central Intelligence Agency Washington, DC 20505 Fax: 703-613-3007 Filing a FOIA Records Request Online The governmentattic.org web site (“the site”) is a First Amendment free speech web site and is noncommercial and free to the public. The site and materials made available on the site, such as this file, are for reference only. The governmentattic.org web site and its principals have made every effort to make this information as complete and as accurate as possible, however, there may be mistakes and omissions, both typographical and in content. The governmentattic.org web site and its principals shall have neither liability nor responsibility to any person or entity with respect to any loss or damage caused, or alleged to have been caused, directly or indirectly, by the information provided on the governmentattic.org web site or in this file. The public records published on the site were obtained from government agencies using proper legal channels. Each document is identified as to the source. Any concerns about the contents of the site should be directed to the agency originating the document in question. GovernmentAttic.org is not responsible for the contents of documents published on the website. 1 O ct 2000_30 April 2002 Creation Date Requester Last Name Case Subject 36802.28679 STRANEY TECHNOLOGICAL GROWTH OF INDIA; HONG KONG; CHINA AND WTO 36802.2992 CRAWFORD EIGHT DIFFERENT REQUESTS FOR REPORTS REGARDING CIA EMPLOYEES OR AGENTS 36802.43927 MONTAN EDWARD GRADY PARTIN 36802.44378 TAVAKOLI-NOURI STEPHEN FLACK GUNTHER 36810.54721 BISHOP SCIENCE OF IDENTITY FOUNDATION 36810.55028 KHEMANEY TI LEAF PRODUCTIONS, LTD. -

And Calcium, Magnesium, Potassium and Sodium Oxybates (Xywav™)
Louisiana Medicaid Sodium Oxybate (Xyrem®) and Calcium, Magnesium, Potassium and Sodium Oxybates (Xywav™) The Louisiana Uniform Prescription Drug Prior Authorization Form should be utilized to request clinical authorization for sodium oxybate (Xyrem®) and calcium, magnesium, potassium and sodium oxybates (Xywav™). These agents have Black Box Warnings and are subject to Risk Evaluation and Mitigation Strategy (REMS) under FDA safety regulations. Please refer to individual prescribing information for details. Approval Criteria • The recipient is 7 years of age or older on date of request; AND • The recipient has a documented diagnosis of narcolepsy or cataplexy; AND • The prescribing provider is a Board-Certified Neurologist or a Board-Certified Sleep Medicine Physician; AND • By submitting the authorization request, the prescriber attests to the following: o The prescribing information for the requested medication has been thoroughly reviewed, including any Black Box Warning, Risk Evaluation and Mitigation Strategy (REMS), contraindications, minimum age requirements, recommended dosing, and prior treatment requirements; AND o All laboratory testing and clinical monitoring recommended in the product prescribing information have been completed as of the date of the request and will be repeated as recommended; AND o The recipient has no inappropriate concomitant drug therapies or disease states. Duration of initial authorization approval: 3 months Reauthorization Criteria • The recipient continues to meet all initial approval criteria; AND