Quality and Health Outcomes Committee AGENDA
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Victor Black Label Discography
The Victor Black Label Discography Victor 25000, 26000, 27000 Series John R. Bolig ISBN 978-1-7351787-3-8 ii The Victor Black Label Discography Victor 25000, 26000, 27000 Series John R. Bolig American Discography Project UC Santa Barbara Library © 2017 John R. Bolig. All rights reserved. ii The Victor Discography Series By John R. Bolig The advent of this online discography is a continuation of record descriptions that were compiled by me and published in book form by Allan Sutton, the publisher and owner of Mainspring Press. When undertaking our work, Allan and I were aware of the work started by Ted Fa- gan and Bill Moran, in which they intended to account for every recording made by the Victor Talking Machine Company. We decided to take on what we believed was a more practical approach, one that best met the needs of record collectors. Simply stat- ed, Fagan and Moran were describing recordings that were not necessarily published; I believed record collectors were interested in records that were actually available. We decided to account for records found in Victor catalogs, ones that were purchased and found in homes after 1901 as 78rpm discs, many of which have become highly sought- after collector’s items. The following Victor discographies by John R. Bolig have been published by Main- spring Press: Caruso Records ‐ A History and Discography GEMS – The Victor Light Opera Company Discography The Victor Black Label Discography – 16000 and 17000 Series The Victor Black Label Discography – 18000 and 19000 Series The Victor Black -

The Greening of Shoreland Hills by Barbara Stodola
THE TM 911 Franklin Street Weekly Newspaper Michigan City, IN 46360 Volume 25, Number 35 Thursday, September 10, 2009 The Greening of Shoreland Hills by Barbara Stodola Blending with the tall trees of Shoreland Hills, the house built by Larry Wood chips blanket the steep dune; the stairway consists of chunks of Zimmer and Ted Perzanowski was designed to harmonize with nature. street pavement salvaged from a vacant lot in Michigan City. On a tree-shaded dune in Shoreland Hills, Larry “It’s been a passion of mine during my thirty-year Zimmer and Ted Perzanowski have built an eco- career, to make a home as environmentally friendly friendly house that defers to the natural beauty of as possible,” says Zimmer. “We used local products, its site. local craftsmen, and recycled materials whenever About forty oaks remain on the property, and a possible. We sent the trees to a sawyer from Har- fi ve-inch mulch of wood chips blankets the ground bert, and a company from Stevensville (Lakeshore – mulch created from the fi fteen trees removed to Stair) did the interior stair treads and fl oor boards.” make way for the house. Chunks of asphalt street On the fi rst fl oor are offi ces for Zimmer, an inte- pavement, hauled away from a vacant lot in Michi- rior designer, and Perzanowski, whose counseling gan City, now form a rustic stairway, climbing up practice is subtitled “Talk To Ted.” the dune – just one of the clever recycling tech- niques used in construction of the house. Greening Continued on Page 2 THE Page 2 September 10, 2009 THE 911 Franklin Street • Michigan City, IN 46360 219/879-0088 • FAX 219/879-8070 In Case Of Emergency, Dial e-mail: News/Articles - [email protected] email: Classifieds - [email protected] http://www.thebeacher.com/ PRINTED WITH Published and Printed by TM Trademark of American Soybean Association THE BEACHER BUSINESS PRINTERS Delivered weekly, free of charge to Birch Tree Farms, Duneland Beach, Grand Beach, Hidden 911 Shores, Long Beach, Michiana Shores, Michiana MI and Shoreland Hills. -

Crowning the Queen of the Sonoran Desert: Tucson and Saguaro National Park
Crowning the Queen of the Sonoran Desert: Tucson and Saguaro National Park An Administrative History Marcus Burtner University of Arizona 2011 Figure 1. Copper Pamphlet produced by Tucson Chamber of Commerce, SAGU257, Box 1, Folder 11, WACC. “In a canon near the deserted mission of Cocospera, Cereus giganteus was first met with. The first specimen brought the whole party to a halt. Standing alone upon a rocky projection, it rose in a single unbranched column to the height of some thirty feet, and formed a sight which seemed almost worth the journey to behold. Advancing into the canon, specimens became more numerous, until at length the whole vegetation was, in places, made up of this and other Cacaceae. Description can convey no adequate idea of this singular vegetation, at once so grand and dreary. The Opuntia arborescens and Cereus Thurberi, which had before been regarded with wonder, now seemed insignificant in comparison with the giant Cactus which towered far above.” George Thurber, 1855, Boundary Commission Report.1 Table of Contents 1 Asa Gray, ―Plantae Novae Thurberianae: The Characters of Some New Genera and Species of Plants in a Collection Made by George Thurber, Esq., of the Late Mexican Boundary ii List of Illustrations v List of Maps ix Introduction Crowning the Queen of the Desert 1 The Question of Social Value and Intrinsically Valuable Landscapes Two Districts with a Shared History Chapter 1 Uncertain Pathways to a Saguaro National Monument, 1912-1933 9 Saguaros and the Sonoran Desert A Forest of Saguaros Discovering -

Super ACRONYM - Round 3
Super ACRONYM - Round 3 1. A joke centered around this name is the punchline to a brief scene that begins with a "mop and bucket man" being called to "The Nauseator." A man in a fishing hat with this name asks "are you talking to me?," and another character with this name is told to "come along" in a scene that also introduces the retired characters Disgruntled (*) Goat and Ku Klux Klam. That confusion surrounding two people with this four-letter name follows a child's pleas to buy a souvenir license plate from the gift shop at Itchy & Scratchy Land. For 10 points, give this name that is comically distinct from the name of Marge and Homer Simpson's son. ANSWER: Bort (do not accept or prompt on "Bart") <Nelson> 2. The Chicago American Gears are likely best known for being the first pro basketball team of this man. This man's five NBA championships all occurred alongside coach John Kundla. An iconic multi-colored basketball was the idea of this co-founder of the (*) ABA. A practice drill involving making layups on alternating sides of the basket is named for this player. The width of the free throw lane and rules regarding goaltending were both changed because of this player's dominance at both DePaul and an NBA team that later moved to the west coast. A number 99 jersey was worn by, for 10 points, what bespectacled center for the Minneapolis Lakers? ANSWER: George (Lawrence) Mikan [MIKE-in] <Nelson> 3. Frank Skinner currently hosts a BBC interview show named for a location in this book. -

Boston Symphony Orchestra Concert Programs, Season 124, 2004-2005
m 2004-2005 SEASON afPF* BOSTON \\ SYM PHONY ORCHESTRA LEVI E JAMES N sin • * * \H iV 4" JAMES LEVINE MUSIC DIRECTOR BERNARD HAITINK CONDUCTOR EMERITUS SEIJI OZAWA MUSIC DIRECTOR LAUREATE Invite the entire string section for cocktails. With floor plans from 2,300 to over Phase One of this 5,000 square feet, you can entertain magnificent property is in grand style at Longyear. 100% sold and occupied. Enjoy 24-hour concierge service, Phase Two is now under con- single-floor condominium living struction and being offered by at its absolute finest, all Sotheby's International Realty & harmoniously located on Hammond Residential Real Estate an extraordinary eight- GMAC. Priced from $1,725,000. acre gated community atop prestigious Call Hammond at (617) 731-4644, Fisher Hill ext. 410. LONGYEAR. fin< ! REASON #11 open heart surgery that's a lot less open There are lots of reasons to consider Beth Israel Deaconess Medical Center for your major medical care. Like minimally invasive heart surgery that minimizes pain, reduces cosmetic trauma and speeds recovery time. From cardiac services and gastroenterology to organ transplantation and cancer care, you'll find some of the most cutting-edge medical advances available anywhere. To find out more, visit www.bidmc.harvard.edu or call 800-667-5356. Beth Israel Deaconess A teaching hospital of Harvard Medical School Medical Center Affiliated with Joslin Clinic | A Research Partner of the Dana-Farber/Harvard Cancer Center | Official Hospital of the Boston Red Sox James Levine, Music Director Bernard Haitink, Conductor Emeritus Seiji Ozawa, Music Director Laureate 124th Season, 2004-2005 Trustees of the Boston Symphony Orchestra, Inc. -

Marisa Mccarthy [email protected] (626) 793-7172 Ext
FOR IMMEDIATE RELEASE Pasadena Symphony Association Pasadena Symphony & POPS Contact: Marisa McCarthy [email protected] (626) 793-7172 ext. 13 For artist bios and images visit: http://pasadenasymphony-pops.org/2018-19-classics- announcement/ February 20, 2018 PASADENA SYMPHONY ANNOUNCES 2018-19 CLASSICS SEASON Guest artists include celebrated violinist Anne Akiko Meyers, Van Cliburn winner Olga Kern, Sphinx Competition winner Melissa White and Baroque concertos featuring the orchestra’s principal musicians. Pasadena, CA – The Pasadena Symphony announces its 91st season with a larger than life schedule of seven concerts, commencing on October 20th with Mozart’s Requiem through to a May 4th finale with the four most famous notes in Classical music – Beethoven’s Fifth Symphony. Other highlights include Mahler’s Symphony No. 1 “Titan,” a tribute to the great Leonard Bernstein and a Tchaikovsky Spectacular for the ages. All concerts take place at Pasadena’s historic Ambassador Auditorium with performances at both 2pm and 8pm. The season also includes the annually sold out Holiday Candlelight Concert, newly lead by Music Director David Lockington, on Saturday, December 15, 2018 with both 4pm and 7pm performances at All Saints Church. The Pasadena Symphony Association is pleased to announce this upcoming season after recently signing a new five-year musician’s contract, reinforcing its position as the area’s premiere destination for live symphonic music with an eye for long-term stability and artistic growth. Music Director David Lockington kicks off the 2018-19 season on October 20, 2018 with Mozart’s hauntingly beautiful Requiem. On November 17th he celebrates three of America’s greatest composers with masterpieces from On the Town to West Side Story from Leonard Bernstein, Aaron Copland and Samuel Barber with Sphinx Competition Laureate -violinist Melissa White. -

18.9 Scores, Books, Catalogues, Pp 207-216
OPERA SCORES 4022. BLUEBEARD’S CASTLE (Béla Bártok). HC. Full score. 1952 Boosey & Hawkes edition. German/English. 174 pp. Very slight spine wear. Just about 1-2. $12.00. 4015. [IL ] CAMPANELLO (Gaetano Donizetti). Maroon Ricordi. 1975 printing. Italian. 149 pp. Just about 1-2. $8.00. 4016. CENDRILLON (Jules Massenet). HC. Au Ménestrel. 1899. 361 pp. Slightest cover wear, otherwise just about 1-2. $15.00. 4004. [THE ] CONSUL (Gian-Carlo Menotti). PC. G. Schirmer. 1950. English. 291 pp. Slightest cover wear. Just about 1-2. $10.00. 4028. [ LA ] DANSEUSE DE TANAGRA (Henri Hirchmann). HC. Choudens, France. 1911. French. 293 pp. A few underlined lines. Some spine wear. Just about 1-2. $15.00. 4018. DEJANICE (Alfredo Catalani). HC. Pub. 1892. 281 pp. This is a 1920 reprint . Loose first page. Slightest cover wear. Otherwise just about 1-2. $12.00. 4030. DINORAH (Giacomo Meyerbeer). HC. Ricordi. No dates, but probably around 1900 printing. Italian. 349 pp. Spine has gold stamping “Lily Pons”. Obviously from her library but in clean, unmarked condition. Just about 1-2. $15.00. 4002. [ THE ] EMPEROR JONES (Louis Gruenberg). PC. Cos Cob Press, NY, 1933. English/German. 174 pp. Pencil writing in inside blank cover pages. Lightest cover mks. Excellent copy. Just about 1-2. $15.00. 4023. [ LA ] FORÊT BLEUE (Louis Aubert). HC. Durand et Cie, France. 1911. French/ English. 236 pp. Lightest spine wear. Just about 1-2. $15.00. 4014. FRANCESCA DA RIMINI (Riccardo Zandonai). HC. Maroon Ricordi. 1945 printing. Italian. 335 pp. Covers loose. Content as new. Just about 1-2. -
THE RECORD COLLECTOR MAGAZINE Given Below Is the Featured Artist(S) of Each Issue (D=Discography, B=Biographical Information)
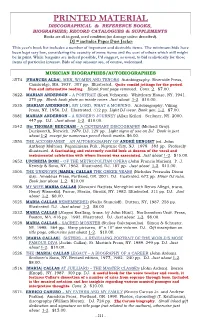
PRINTED MATERIAL DISCOGRAPHICAL & REFERENCE BOOKS, BIOGRAPHIES; RECORD CATALOGUES & SUPPLEMENTS Books are all in good, used condition (no damage unless described). DJ = includes Paper Dust Jacket This year’s book list includes a number of important and desirable items. The minimum bids have been kept very low, considering the scarcity of some items and the cost of others which still might be in print. While bargains are indeed possible, I’d suggest, as usual, to bid realistically for those items of particular interest. Bids of any amount are, of course, welcomed. MUSICIAN BIOGRAPHIES/AUTOBIOGRAPHIES 3574. [FRANCES ALDA]. MEN, WOMEN AND TENORS. Autobiography. Riverside Press, Cambridge, MA. 1937. 307 pp. Illustrated. Quite candid jottings for the period. Fun and informative reading. Blank front page removed. Cons. 2. $7.00. 3622. MARIAN ANDERSON – A PORTRAIT (Kosti Vehanen). Whittlesey House, NY. 1941. 270 pp. Blank book plate on inside cover. Just about 1-2. $10.00. 3535. [MARIAN ANDERSON]. MY LORD, WHAT A MORNING. Autobiography. Viking Press, NY. 1956. DJ. Illustrated. 312 pp. Light DJ wear. Book gen. 1-2. $7.00. 3581. MARIAN ANDERSON – A SINGER’S JOURNEY (Allan Keiler). Scribner, NY. 2000. 447 pp. DJ. Just about 1-2. $10.00. 3542. [Sir THOMAS] BEECHAM – A CENTENARY DISCOGRAPHY (Michael Gray). Duckworth, Norwich. 1979. DJ. 129 pp. Light signs of use on DJ. Book is just about 1-2 except for numerous pencil check marks. $6.00. 3550. THE ACCOMPANIST – AN AUTOBIOGRAPHY OF ANDRÉ BENOIST (ed. John Anthony Maltese). Paganiniana Pub., Neptune City, NJ. 1978. 383 pp. Profusely illustrated. A fascinating and extremely candid look at dozens of the vocal and instrumental celebrities with whom Benoist was associated. -
This Property Is Listed in the National Register of Historic Places In
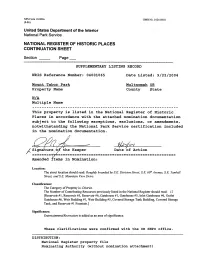
NFS Form 10-900a OMB No. 1024-0018 (8-86) United States Department of the Interior National Park Service NATIONAL REGISTER OF HISTORIC PLACES CONTINUATION SHEET Section ___ Page __ SUPPLEMENTARY LISTING RECORD NRIS Reference Number: 04001065 Date Listed: 9/22/2004 Mount Tabor Park Multnomah OR Property Name County State N/A Multiple Name This property is listed in the National Register of Historic Places in accordance with the attached nomination documentation subject to the following exceptions, exclusions, or amendments, notwithstanding the National Park Service certification included in the nomination documentation. '——' f / / r I 7 / Signature /or the Keeper Date of Action — — — — = = — — _/L^_ _____ ______ = = _______ = ____ = ___ = _____.__ = = _______ = ___: _ Amended Items in Nomination: Location: The street location should read: Roughly bounded by S.E. Division Street, S.E. 60th Avenue, S.E. Yamhill Street, and S.E. Mountain View Drive. Classification: The Category of Property is: District. The Number of Contributing Resources previously listed in the National Register should read: 12 [Reservoir #1, Reservoir #5, Reservoir #6, Gatehouse #1, Gatehouse #5, Inlet Gatehouse #6, Outlet Gatehouse #6, Weir Building #1, Weir Building #5, Covered Storage Tank Building, Covered Storage Tank, and Reservoir #1 Fountain.] Significance: Entertainment/Recreation is added as an area of significance. These clarifications were confirmed with the OR SHPO office DISTRIBUTION: National Register property file Nominating Authority (without nomination attachment) NFS Form 10-900 ,r- OMB No. 10024-0018 (Oct.1990) United States Department of the Interior National Park Service National Register of Historic Places Registration Form This form is for use in nominating or requesting determinations for individual properties and districts. -

Boston Symphony Orchestra Concert Programs, Summer, 2002
BOSTON SYMPHONY ORCHESTRA 2002 season " ''**/ v % f-iw ''*":'*' ..V „*''.< .. 4& ^ - V » •' '>' ' irf , J ^ v:>? . 5 •^t - I ORIGINS GflUCRV formerly TRIBAL ARTS GALLERY, NYC Ceremonial and modern sculpture for new and advanced collectors Open 7 Days 36 Main St. POB 905 413-298-0002 Stockbridge, MA 01 262 . Every car has its moment. This one has thousands per second. iiflH Sillfll! The new 3 Series. Pure drive, The New ^KS*. BMW 3 Series /gPr^E^ From $27,745* \jf Test drive The Ultimate Driving Machine^ bmwusa.com The Ultimate at your authorized BMW center 1-800-334-4BMW Driving Machine* . For all there is to see and do in city after city, after city, after city. Britain is brimming with the finest theatre, art, music, entertainment, dining, shopping and more, in city after city. So is our UK City Experience Guide. It's rich with information about the incredible range of all there is to see and do in the cities of Britain. From living it up in Liverpool, to immersing yourself in drama in Bath. For your free copy of the UK City Experience Guide call 1-800-205-9846, visit us on the web at www. travelbritain.org/cityculture. BRITISH TOURIST AUTHORITY BOSTON SYMPHONY ORCHESTRA One Hundred and Twenty-First Season, 2001-02 TANGLEWOOD 2002 Trustees of the Boston Symphony Orchestra, Inc. Peter A. Brooke, Chairman Dr. Nicholas T. Zervas, President Deborah Davis Berman, Vice-Chairman Vincent M. O'Reilly, Treasurer Julian Cohen, Vice-Chairman Ray Stata, Vice-Chairman Nina L. Doggett, Vice-Chairman Harlan E. Anderson Charles K. -
|||GET||| What Love Has Done 1St Edition
WHAT LOVE HAS DONE 1ST EDITION DOWNLOAD FREE Elizabeth Cain | 9781532014321 | | | | | Leaves Of Love: Stories for Ageing & Dying Well Belgium Ultratop 50 Flanders [14]. That is until returning home after a short absence south of the border, the East Lothian writing beastie caught her by the tail and sat her down to gather her sheaf of stories into Leaves of Love. This is the most terrifying and exciting process imaginable! Retrieved February 11, Apologies for the silence. The song hit number one in both the United Kingdom and the United States and is the group's biggest hit to date. Singer Jessie Ware released a cover version in April[4] and singer Delta Goodrem released a cover version in September It also suggests some ideas for laying out a body, possible rituals and the importance of grieving. What treasures you are! Mick Jones [4]. June 10, Lot Les Mots An error has occurred while processing this page. The Scotsman. This version of the song was included in a popular Brazilian soap opera, Senhora do Destino. I am quite overwhelmed by your generosity and support for this project. US Billboard Hot []. US Adult Contemporary Billboard []. I have been sitting on the proverbial river bank, head under my wing, feeling very despondant. Phone: Email: yourshipment westsidemailcenter. Westside Mail What Love Has Done 1st edition will proactively reach out to you to arrange packing, shipping and insurance. Knowing so many people also believe in Leaves of Love has also made a big difference. Plus everything from 10x Paperback Bundle. Visit our Help Centre to find out more. -

The Victor Red Seal Discography, Volume II: Double-Sided Series To
The Victor Red Seal Discography, Volume II: Double-Sided Series to 1930 , and: The Victor Black Label Discography: 16000–17000 Series , and: The Victor Black Label Discography: 18000–19000 Series , and: The Victor Discography: Green, Blue and Purple Labels , and: The Edison Discography (1926–1929) (review) Gary A. Galo Notes, Volume 66, Number 3, March 2010, pp. 575-579 (Review) Published by Music Library Association DOI: https://doi.org/10.1353/not.0.0312 [ This contentFor additional has been information declared free about to read this byarticle the pubisher during the COVID-19 pandemic. ] https://muse.jhu.edu/article/376356 Book Reviews 575 posed right at the outset in the Tokita- tions; but with the considerable lean to- Hughes introductory chapter. wards the survey in many of its essays, it This is a research companion that works would be well placed too in undergraduate very well indeed, if one works hard with it; collections supporting performing-arts- it is a book for poring over, both with re- orientated Asian Studies programs, and in gard to its texts and its music examples; collections supporting (ethno)musicology and it rewards reading across its various programs with a focus on East Asia. A most chapters. It is an articulate, forward-looking welcome new friend! companion demanding interaction, but as- suming a certain amount of self-reliance in its partner. It goes without saying that it is Elizabeth Markham clearly essential for graduates in the field, University of Arkansas and accordingly for graduate library collec- BIBLIOGRAPHY The Victor Red Seal Discography, Volume II: Double-Sided Series to 1930.