Exposure Assessment and Medical Surveillance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Model for Mandatory Job Safety Analysis Embedded in the Premit-To-Work System >
International Gas Union Research Conference 2011 <A MODEL FOR MANDATORY JOB SAFETY ANALYSIS EMBEDDED IN THE PREMIT-TO-WORK SYSTEM > Main author I. K. Yoon KOREA ABSTRACT Permit to Work (PTW) systems is defined as "a formal documented system used to control the certain types of work that are potentially hazardous". Generally, PTW system should be designed to specify the work to be done safely and the precaution to be taken as well as approval, responsibility, permissions of work. For this reason, PTW is regarded as one of the most important safety management system to control the risk of maintenance that causes 30% of the accident in chemical industries. In the early days, PTW was based on paper based system. But recently has continued to evolve into a computer based system. And these advanced systems has been applied to 80% of oil industry in North Sea and upgraded with providing the hazard information as well as supporting documentation. Usually, the hazard information is provided in the form of hazard checklist or attached risk assessment report such as JSA sheet. But when we consider the various types of work, place and environment, all the potential work related hazard cannot be reviewed in the form of prescribed checklist or certain attachment. To review the potential hazard perfectly, the work permit should be supported by Job Safety Analysis (JSA). But it has rarely been seen that company have a rule to require the mandatory JSA whenever permit to work is accomplished. Despite a relatively simple analysis structure, it is time-consuming and person-consuming methodology to complete all the procedure. -

Personal Protective Equipment Hazard Assessment
WORKER HEALTH AND SAFETY Personal Protective Equipment Hazard Assessment Oregon OSHA Personal Protective Equipment Hazard Assessment About this guide “Personal Protective Equipment Hazard Assessment” is an Oregon OSHA Standards and Technical Resources Section publication. Piracy notice Reprinting, excerpting, or plagiarizing this publication is fine with us as long as it’s not for profit! Please inform Oregon OSHA of your intention as a courtesy. Table of contents What is a PPE hazard assessment ............................................... 2 Why should you do a PPE hazard assessment? .................................. 2 What are Oregon OSHA’s requirements for PPE hazard assessments? ........... 3 Oregon OSHA’s hazard assessment rules ....................................... 3 When is PPE necessary? ........................................................ 4 What types of PPE may be necessary? .......................................... 5 Table 1: Types of PPE ........................................................... 5 How to do a PPE hazard assessment ............................................ 8 Do a baseline survey to identify workplace hazards. 8 Evaluate your employees’ exposures to each hazard identified in the baseline survey ...............................................9 Document your hazard assessment ...................................................10 Do regular workplace inspections ....................................................11 What is a PPE hazard assessment A personal protective equipment (PPE) hazard assessment -

Guidelines for Human Exposure Assessment Risk Assessment Forum
EPA/100/B-19/001 October 2019 www.epa.gov/risk Guidelines for Human Exposure Assessment Risk Assessment Forum EPA/100/B-19/001 October 2019 Guidelines for Human Exposure Assessment Risk Assessment Forum U.S. Environmental Protection Agency DISCLAIMER This document has been reviewed in accordance with U.S. Environmental Protection Agency (EPA) policy. Mention of trade names or commercial products does not constitute endorsement or recommendation for use. Preferred citation: U.S. EPA (U.S. Environmental Protection Agency). (2019). Guidelines for Human Exposure Assessment. (EPA/100/B-19/001). Washington, D.C.: Risk Assessment Forum, U.S. EPA. Page | ii TABLE OF CONTENTS DISCLAIMER ..................................................................................................................................... ii LIST OF TABLES.............................................................................................................................. vii LIST OF FIGURES ........................................................................................................................... viii LIST OF BOXES ................................................................................................................................ ix ABBREVIATIONS AND ACRONYMS .............................................................................................. x PREFACE ........................................................................................................................................... xi AUTHORS, CONTRIBUTORS AND -

Hazards Analysis Report
PROJECT MANAGEMENT Doc. No. LUSI SUB-SYSTEM DOCUMENT PM-391-001-34 R0 1.1 Management Hazards Analysis Report Technical Contact: Nadine Kurita LUSI Chief Engineer Signature Date Approved by: Tom Fornek LUSI Project Manager Signature Date Approved by: John Galayda LCLS Project Director Signature Date Rev Description Date 0 Initial Release July 8, 2008 PM-391-001-34 R0 Verify that this is the latest revision. 1 of 34 Check for change orders or requests TABLE OF CONTENTS 1. Introduction............................................................................................................. 3 1.1 Purpose and Scope .............................................................................................. 3 1.2 Environment, Worker and Public Safety ............................................................ 3 2. Summary................................................................................................................. 4 2.1 Overview of Hazards .......................................................................................... 4 2.2 Comprehensiveness of the Safety Analysis ........................................................ 5 2.3 Appropriateness of the Accelerator Safety Envelope ......................................... 5 3. Project Description..................................................................................................5 3.1 X-Ray Pump/Probe Diffraction Instrument........................................................ 6 3.2 Coherent X-ray Imaging Instrument.................................................................. -
Personal Protective Equipment/Job Hazard Analysis Program
SALISBURY UNIVERSITY PPE/JOB HAZARD ANALYSIS STANDARD PRACTICE INSTRUCTION DATE: January 15, 2019 SUBJECT: Personal Protective Equipment/Job Hazard Analysis Program REGULATORY STANDARD: 29 CFR §1910.132-138. I. PURPOSE: The purpose of this program is to establish procedures for wearing Personal Protective Equipment (PPE) by all Salisbury University employees, contractors and visitors on campus. This program supports compliance with the Occupational Safety and Health Administration (OSHA) standards that cover PPE, specifically, 29 CFR 1910.132, .133, .135, .136 and .138. This program applies to all University employees, contractors and visitors who work in areas that contain hazards to the eyes, face, head, hands and feet. Respiratory and noise hazards are covered in the S0U Respiratory Protection Program and the SU Hearing Conservation Program. II. DEFINITIONS: ANSI (American National Standards Institute): A nonprofit organization that approves national safety standards. Ophthalmologist: A physician/surgeon who specializes in diagnosing and treating eye diseases and disorders. Optician: A skilled technician who, when given a medical prescription, is qualified to make, fit and dispense eyeglasses and contact lenses, either in an optical laboratory or for retail sale to the public; opticians do not examine patients or write prescriptions. Optometrist: A licensed primary eye-care provider who performs eye examinations, prescribes and dispenses eyeglasses and contact lenses and performs some diagnostic work, such as screening for glaucoma or cataracts. Plano: A common term for nonprescription safety glasses. PPE: Personal Protective Equipment III. RESPONSIBILITIES: A. The Program Administrator The SU PPE Program Administrator is the Director of Sustainability & Environmental Safety. Responsibilities include: Modify only under the supervision of the Safety Manager. -
Personal Protective Equipment (PPE) Guide
Personal Protective Equipment (PPE) Guide Volume 1: General PPE February 2003 F417-207-000 This guide is designed to be used by supervisors, lead workers, managers, employers, and anyone responsible for the safety and health of employees. Employees are also encouraged to use information in this guide to analyze their own jobs, be aware of work place hazards, and take active responsibility for their own safety. Photos and graphic illustrations contained within this document were provided courtesy of the Occupational Safety and Health Administration (OSHA), Oregon OSHA, United States Coast Guard, EnviroWin Safety, Microsoft Clip Gallery (Online), and the Washington State Department of Labor and Industries. TABLE OF CONTENTS (If viewing this pdf document on the computer, you can place the cursor over the section headings below until a hand appears and then click. You can also use the Adobe Acrobat Navigation Pane to jump directly to the sections.) How To Use This Guide.......................................................................................... 4 A. Introduction.........................................................................................6 B. What you are required to do ..............................................................8 1. Do a Hazard Assessment for PPE and document it ........................................... 8 2. Select and provide appropriate PPE to your employees................................... 10 3. Provide training to your employees and document it ........................................ 11 -
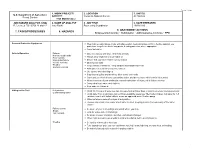
7. Tasks/Procedures 8. Hazards 9. Abatement
FS-6700-7 (11/99) 1. WORK PROJECT/ 2. LOCATION 3. UNIT(S) U.S. Department of Agriculture ACTIVITY Coconino National Forest All Districts Forest Service Trail Maintenance JOB HAZARD ANALYSIS (JHA) 4. NAME OF ANALYST 5. JOB TITLE 6. DATE PREPARED References-FSH 6709.11 and 12 Amy Racki Partnership Coordinator 10/28/2013 9. ABATEMENT ACTIONS 7. TASKS/PROCEDURES 8. HAZARDS Engineering Controls * Substitution * Administrative Controls * PPE Personal Protective Equipment Wear helmet, work gloves, boots with slip-resistant heels and soles with firm, flexible support, eye protection, long sleeve shirts, long pants, hearing protection where appropriate Carry first aid kit Vehicle Operation Fatigue Drive defensively and slow. Watch for animals Narrow, rough roads Always wear seatbelts and turn lights on Poor visibility Mechanical failure Ensure that you have reliable communication Vehicle Accients Obey speed limits Weather Keep vehicles maintained. Keep windows and windshield clean Animals on Road Anticipate careless actions by other drivers Use spotter when backing up Stay clear of gullies and trenches, drive slowly over rocks. Carry and use chock blocks, use parking brake, and do not leave vehicle while it is running Inform someone of your destination and estimated time of return, call in if plans change Carry extra food, water, and clothing Stop and rest if fatigued Hiking on the Trail Dehydration Drink 12-15 quarts of water per day, increase fluid on hotter days or during extremely strenuous activity Contaminated water Drink -

Safety Manual
Eastern Elevator Safety and Health Manual January 2017 Page 1 of 125 SAFETY AND HEALTH MANUAL Index by Section Number Safety Policy ................................................................................................................. …4 Section 1: General Health and Safety Policies ............................................................. …5 Section 2: Hazard Communication ................................................................................ ..13 Section 3: Personal Protective Equipment (PPE) ......................................................... ..18 Section 4: Emergency Action Plan ................................................................................ ..31 Section 5: Fall Protection .............................................................................................. ..34 Section 6: Ladder Safety ............................................................................................... ..38 Section 7: Bloodborne Pathogens ................................................................................ ..42 Section 8: Motor Vehicle / Fleet Safety ......................................................................... ..47 Section 9: Hearing Conservation .................................................................................. ..50 Section 10: Lockout / Tagout ........................................................................................ ..53 Section 11: Fire Prevention .......................................................................................... -

EPA COVID-19 Job Hazard Analysis (JHA) Supplement, July 6, 2020, Final
EPA COVID-19 Job Hazard Analysis (JHA) Supplement, July 6, 2020, Final Table of Contents 1. Introduction 2. OSHA Worker Exposure Risk to COVID-19, Summary 3. Pre-Travel Considerations 4. EPA COVID-19 Job Hazard Analysis (JHA) Supplement Instructions 5. EPA COVID-19 Job Hazard Analysis (JHA) Supplement Template 6. EPA COVID-19 OLEM Job Hazard Analysis Supplement Example 1. Introduction • The COVID-19 Public Health Emergency is very dynamic. Federal, state and local government guidance is updated frequently. There may be new CDC, OSHA or EPA guidance that will impact the current content of this JHA prior to the next update. As a result, it is important to review the government links in this JHA for new information. Additionally, due to possible differences in state or local health department requirements on COVID-19, the employee, supervisor and the SHEMP manager should review applicable state/local requirements before traveling and deployment to a site. These state/local requirements may be more flexible for essential workers that are traveling into the area, and EPA travel for field work may qualify as such essential travel. • Prior to travel, assess the prevalence for COVID-19 cases in the area(s) you are traveling to (and through) in addition to where you will be performing site work. This assessment should include evaluation of whether the area has demonstrated a downward trajectory of positive tests and documented cases within a 14-day period. Including this will help staff determine how to “assess the prevalence.”. • Specific COVID-19 information can be found on state/territorial/local government and health department websites. -

A PRACTICAL GUIDE for USE of REAL TIME DETECTION SYSTEMS for WORKER PROTECTION and COMPLIANCE with OCCUPATIONAL EXPOSURE LIMITS May 2019
A PRACTICAL GUIDE FOR USE OF REAL TIME DETECTION SYSTEMS FOR WORKER PROTECTION AND COMPLIANCE WITH OCCUPATIONAL EXPOSURE LIMITS May 2019 WHITE PAPER May 2019 A PRACTICAL GUIDE FOR USE OF REAL TIME DETECTION SYSTEMS FOR WORKER PROTECTION AND COMPLIANCE WITH OCCUPATIONAL EXPOSURE LIMITS Prepared by: Energy Facility Contractor’s Group (EFCOG) Industrial Hygiene and Safety Task Group and Members of the American Industrial Hygiene Association (AIHA) Exposure Assessment Strategies Group Dina Siegel1, David Abrams 2, John Hill3, Steven Jahn2, Phil Smith2, Kayla Thomas4 1 Los Alamos National Laboratory 2 AIHA Exposure Assessment Strategies Committee 3 Savannah River Site 4 Kansas City National Security Campus A PRACTICAL GUIDE FOR USE OF REAL TIME DETECTION SYSTEMS FOR WORKER PROTECTION AND COMPLIANCE WITH OCCUPATIONAL EXPOSURE LIMITS May 2019 Table of Contents 1.0 Executive Summary 2.0 Introduction 3.0 Discussion 3.1 Occupational Exposure Assessment 3.2 Regulatory Compliance 3.3 Occupational Exposure Limits 3.4 Traditional Use of Real Time Detection Systems 3.5 Use and Limitations of Real Time Detection Systems 3.6 Use of Real Time Detection Systems for Compliance 3.7 Documentation/Reporting of Real Time Detection Systems Results 3.8 Peak Exposures Data Interpretations 3.9 Conclusions 4.0 Matrices 5.0 References 6.0 Attachments Page | 2 A PRACTICAL GUIDE FOR USE OF REAL TIME DETECTION SYSTEMS FOR WORKER PROTECTION AND COMPLIANCE WITH OCCUPATIONAL EXPOSURE LIMITS May 2019 1.0 Executive Summary This white paper presents practical guidance for field industrial hygiene personnel in the use and application of real time detection systems (RTDS) for exposure monitoring. -

Supplementary File 2: Assessment of Quality and Bias
Supplementary File 2: Assessment of quality and bias In preparing the tool, it was not possible to identify a dominant factor for which studies should be controlled for, instead recognising several key variables. Comparability was therefore scored against a single criterion of ‘effectively controlling for relevant factors’, meaning a maximum of eight points, rather than nine, were available. Where a nested cohort or matched case group was identified within an interventional study, it was agreed that the quality of the study as applied to impact of ETS would be appraised, and not the main interventional study outcomes. This acknowledged that high quality trials not relevant to the impact of ETS exposure could contain poor quality cohorts that were appropriate for inclusion, or vice versa. A point was awarded for satisfactory response on each question, indicated by a tick in the relevant table. Cohort Outcome Measures Domain and outcomes Point Representativeness of the exposed cohort A Truly representative of the paediatric population undergoing surgery B Somewhat representative of the paediatric population undergoing surgery C Selected subgroup of the population undergoing surgery D No description of the cohort selection process Selection of the non-exposed cohort A Drawn from the same community as the exposed cohort B Drawn from a different source C No description of the derivation of the non-exposed cohort Ascertainment of exposure A Secure record (e.g. surgical record, biological test) B Structured interview C Written self-report of self-completed questionnaire D No description Demonstration that outcome of interest was not present at start of the study A Yes B No Comparability of cohorts on the basis of the design or analysis A Study controls for reasonable factors (e.g. -
Exposure Assessment Concepts
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike License. Your use of this material constitutes acceptance of that license and the conditions of use of materials on this site. Copyright 2006, The Johns Hopkins University, Patrick Breysse, and Peter S. J. Lees. All rights reserved. Use of these materials permitted only in accordance with license rights granted. Materials provided “AS IS”; no representations or warranties provided. User assumes all responsibility for use, and all liability related thereto, and must independently review all materials for accuracy and efficacy. May contain materials owned by others. User is responsible for obtaining permissions for use from third parties as needed. Exposure Assessment Concepts Patrick N. Breysse, PhD, CIH Peter S.J. Lees, PhD, CIH Johns Hopkins University Section A Introduction Origin of Hygiene Hygeia was the Greek goddess of health Rene Dubos wrote: “For the worshippers of Hygeia, health is … a positive attribute to which men are entitled if they govern their lives wisely” Prevention is key 4 Exposure—Definition Contact between the outer boundary of the human body (skin, nose, lungs, GI tract) and a contaminant Requires the simultaneous presence of a contaminant and the contact between the person and that medium Quantified by concentration of contaminant and time and frequency of contact 5 Route of Exposure Inhalation Ingestion Dermal Direct injection Inhalation is most common in workplace—but not in general environment Moving towards concept of total exposure 6 Exposure Assessment Magnitude – Concentration in media (ppm, f/cc) Duration – Minutes, hours, days, working life, lifetime Frequency – Daily, weekly, seasonally 7 Types of Air Sampling: Time Source: U.S.