Effects of Sustained Phencyclidine Exposure on Sensorimotor Gating of Startle in Rats Zoë A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
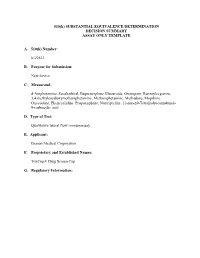
510(K) SUBSTANTIAL EQUIVALENCE DETERMINATION CHECKLIST
510(k) SUBSTANTIAL EQUIVALENCE DETERMINATION DECISION SUMMARY ASSAY ONLY TEMPLATE A. 510(k) Number: k122633 B. Purpose for Submission: New device C. Measurand: d-Amphetamine, Secobarbital, Buprenorphine Glucuroide, Oxazepam, Benzoylecgonine, 3,4-methylenedioxymethamphetamine, Methamphetamine, Methadone, Moprhine, Oxycodone, Phencyclidine, Propoxyphene, Nortriptyline, 11-nor-∆9-Tetrahydrocannabinol- 9-carboxylic acid D. Type of Test: Qualitative lateral flow immunoassay E. Applicant: Branan Medical Corporation F. Proprietary and Established Names: ToxCup® Drug Screen Cup G. Regulatory Information: Product Classification Regulation Section Panel Code LDJ II 862.3870 Cannabinoid test system Toxicology (91) DIO II 862.3250 Cocaine and cocaine metabolite Toxicology (91) test system DJG II 862.3650 Opiate test system Toxicology (91) DJC II 862.3610 Methamphetamine test system Toxicology (91) DKZ II 862.3100 Amphetamine test system Toxicology (91) LCM unclassifed Enzyme immunoassay Phencyclidine Toxicology (91) JXM II 862.3170 Benzodiazepine test system Toxicology (91) DIS II 862.3150 Barbiturate test system Toxicology (91) DJR II 862.3620 Methadone test system Toxicology (91) LFG II 862.3910 Tricyclic antidepressant drugs Toxicology (91) test system JXN II 862.3700 Propoxyphene test system Toxicology (91) H. Intended Use: 1. Intended use(s): See indications for use below. 2. Indications(s) for use: The ToxCup Drug Screen Cup is an in vitro screening test for the rapid detection of multiple drugs and drug metabolites in human urine at or above -

The Alkaloids: Chemistry and Biology
CONTRIBUTORS Numbers in parentheses indicate the pages on which the authors’ contributions begin. B. EMMANUEL AKINSHOLA (135), Department of Pharmacology, College of Medicine, Howard University, Washington, DC 20059, eakinshola@ howard.edu NORMA E. ALEXANDER (293), NDA International, 46 Oxford Place, Staten Island, NY 10301, [email protected] SYED F. ALI (79, 135), Division of Neurotoxicology, National Center for Toxicological Research, 3900 NCTR Road, Jefferson, AR 72079, [email protected] KENNETH R. ALPER (1, 249), Departments of Psychiatry and Neurology, New York University School of Medicine, 550 First Avenue, New York, NY 10016, [email protected] MICHAEL H. BAUMANN (79), Clinical Psychopharmacology Section, Intra- mural Research Program, NIDA, National Institutes of Health, Baltimore, MD 21224, [email protected] DANA BEAL (249), Cures-not-Wars, 9 Bleecker Street, New York, NY 10012, [email protected] ZBIGNIEW K. BINIENDA (193), Division of Neurotoxicology, National Cen- ter for Toxicological Research, 3900 NCTR Road, Jefferson, AR 72079, [email protected] WAYNE D. BOWEN (173), Laboratory of Medicinal Chemistry, NIDDK, NIH, Building 8 B1-23, 8 Center Drive, MSC 0820, Bethesda, MD 20892, [email protected] FRANK R. ERVIN (155), Department of Psychiatry and Human Genetics, McGill University, Montreal, Quebec H3A 2T5, Canada, md18@musica. mcgill.ca JAMES W. FERNANDEZ (235), Department of Anthropology, University of Chicago, 1126 E. 59th Street, Chicago, IL 60637, jwfi@midway. uchicago.edu xi xii CONTRIBUTORS RENATE L. FERNANDEZ (235), Department of Anthropology, University of Chicago, 1126 E. 59th Street, Chicago, IL 60637, rlf2@midway. uchicago.edu GEERTE FRENKEN (283), INTASH, P.O. -

Characterization of Multiple Sites of Action of Ibogaine
——Chapter 6—— CHARACTERIZATION OF MULTIPLE SITES OF ACTION OF IBOGAINE Henry Sershen, Audrey Hashim, And Abel Lajtha Nathan Kline Institute Orangeburg, New York 10962 I. Introduction.................................................................................................................. II. Issues Related to Ibogaine in the Treatment of Drug Dependence............................. A. Dopamine as a Primary Site of Drug-Mediated Responses .................................. B. Ibogaine or Its Metabolite and Acute versus Long-Term Effect........................... C. Single or Multiple Sites of Action of Ibogaine ..................................................... III. Effect of Ibogaine on Drug-Induced Behavior............................................................ IV. Binding Site Activity ................................................................................................... A. Relevant Site of Action.......................................................................................... V. Functional Activity ...................................................................................................... VI. Stimulant Drug Actions/Behaviors.............................................................................. VII. Current Non-Ibogaine Drug Treatment Protocols ....................................................... VIII. Conclusions.................................................................................................................. References................................................................................................................... -

Phencyclidine: an Update
Phencyclidine: An Update U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol, Drug Abuse and Mental Health Administration Phencyclidine: An Update Editor: Doris H. Clouet, Ph.D. Division of Preclinical Research National Institute on Drug Abuse and New York State Division of Substance Abuse Services NIDA Research Monograph 64 1986 DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administratlon National Institute on Drug Abuse 5600 Fishers Lane Rockville, Maryland 20657 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 NIDA Research Monographs are prepared by the research divisions of the National lnstitute on Drug Abuse and published by its Office of Science The primary objective of the series is to provide critical reviews of research problem areas and techniques, the content of state-of-the-art conferences, and integrative research reviews. its dual publication emphasis is rapid and targeted dissemination to the scientific and professional community. Editorial Advisors MARTIN W. ADLER, Ph.D. SIDNEY COHEN, M.D. Temple University School of Medicine Los Angeles, California Philadelphia, Pennsylvania SYDNEY ARCHER, Ph.D. MARY L. JACOBSON Rensselaer Polytechnic lnstitute National Federation of Parents for Troy, New York Drug Free Youth RICHARD E. BELLEVILLE, Ph.D. Omaha, Nebraska NB Associates, Health Sciences Rockville, Maryland REESE T. JONES, M.D. KARST J. BESTEMAN Langley Porter Neuropsychiatric lnstitute Alcohol and Drug Problems Association San Francisco, California of North America Washington, D.C. DENISE KANDEL, Ph.D GILBERT J. BOTV N, Ph.D. College of Physicians and Surgeons of Cornell University Medical College Columbia University New York, New York New York, New York JOSEPH V. -

01-Stanojlovic.Vp:Corelventura
Acta Veterinaria (Beograd), Vol. 58, No. 2-3, 111-120, 2008. DOI: 10.2298/AVB0803111S UDK 619:616.853 EFECTS OF ETHANOL ON ELECTROENCEPHALOGRAPHIC AND BEHAVIORAL SIGNS OF METAPHIT-INDUCED AUDIOGENIC SEIZURE STANOJLOVI] OLIVERA*, PETROVI] BOJANA*, HRN^I] D*, MLADENOVI] D**, RA[I] ALEKSANDRA* and [U[I] VESELINKA*** *Department of Physiology, School of Medicine, University of Belgrade, Serbia **Department of Pathophysiology, School of Medicine, University of Belgrade; *** Serbian Academy of Sciences and Arts, Serbia (Received 17. November 2007) The goal of the experiment was to give an answer to the question whether the simultaneous action of metaphit and audiogenic stimulation, which together lead to generalized reflex seizure in rodents, could be modified by ethanol. The rats divided in four groups received (i.p.): saline; metaphit (10 mg/kg); metaphit (10 mg/kg) + ethanol (2 g/kg); and ethanol (2 g/kg). Ethanol was administered to the metaphit-treated animals which had displayed seizures in the first eight tests. Audiogenic stimulation was applied at hourly intervals starting from the first hour after giving the metaphit injection throughout 16 hours of the experiment. For EEG recordings, three gold-plated electrodes were implanted into the rat skull. Metaphit led to hypersynchrounus epileptiform activity which forms polyspikes and spike-wave complexes. Behavior was represented by established grades of motor seizures. It was noticed that ethanol significantly decreased EEG signs of seizure, reduced the frequency as the amplitude of the waves increased (dominant ones were d and q). Ethanol completely blocked all the manifestations of the convulsive behavior of metaphit-treated animals. The results of this experiment suggest that ethanol inhibits behavioral and modifies EEG signs of the metaphit induced audiogenic generalized epilepsy. -
B 0621 DJS1700000009 03.Pdf
The following documentation is an electronically‐ submitted vendor response to an advertised solicitation from the West Virginia Purchasing Bulletin within the Vendor Self‐Service portal at wvOASIS.gov. As part of the State of West Virginia’s procurement process, and to maintain the transparency of the bid‐opening process, this documentation submitted online is publicly posted by the West Virginia Purchasing Division at WVPurchasing.gov with any other vendor responses to this solicitation submitted to the Purchasing Division in hard copy format. Purchasing Division State of West Virginia 2019 Washington Street East Solicitation Response Post Office Box 50130 Charleston, WV 25305-0130 Proc Folder : 311309 Solicitation Description : ADDENDUM 3 DRUG TESTING KITS AND SUPPLIES Proc Type : Central Master Agreement Date issued Solicitation Closes Solicitation Response Version 2017-04-11 SR 0621 ESR04101700000004880 1 13:30:00 VENDOR 000000221536 REDWOOD TOXICOLOGY LABORATORY INC Solicitation Number: CRFQ 0621 DJS1700000009 Total Bid : $117,980.00 Response Date: 2017-04-11 Response Time: 00:31:03 Comments: FOR INFORMATION CONTACT THE BUYER Crystal Rink (304) 558-2402 [email protected] Signature on File FEIN # DATE All offers subject to all terms and conditions contained in this solicitation Page : 1 FORM ID : WV-PRC-SR-001 Line Comm Ln Desc Qty Unit Issue Unit Price Ln Total Or Contract Amount 1 13 Panel Urine Test Kit 8000.00000 EA $5.050000 $40,400.00 Comm Code Manufacturer Specification Model # 46151606 Extended Description : 13 Panel Urine Test Kit Comments: See Pricing Page Exhibit A for more details, including optional cup item. Five business days for RTL inventory product (i.e. -

Pharmacology and Therapeutic Potential of Sigma1 Receptor Ligands E.J
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central 344 Current Neuropharmacology, 2008, 6, 344-366 Pharmacology and Therapeutic Potential of Sigma1 Receptor Ligands E.J. Cobos1,2, J.M. Entrena1, F.R. Nieto1, C.M. Cendán1 and E. Del Pozo1,* 1Department of Pharmacology and Institute of Neuroscience, Faculty of Medicine, and 2Biomedical Research Center, University of Granada, Granada, Spain Abstract: Sigma () receptors, initially described as a subtype of opioid receptors, are now considered unique receptors. Pharmacological studies have distinguished two types of receptors, termed 1 and 2. Of these two subtypes, the 1 re- ceptor has been cloned in humans and rodents, and its amino acid sequence shows no homology with other mammalian proteins. Several psychoactive drugs show high to moderate affinity for 1 receptors, including the antipsychotic haloperi- dol, the antidepressant drugs fluvoxamine and sertraline, and the psychostimulants cocaine and methamphetamine; in ad- dition, the anticonvulsant drug phenytoin allosterically modulates 1 receptors. Certain neurosteroids are known to interact with 1 receptors, and have been proposed to be their endogenous ligands. These receptors are located in the plasma membrane and in subcellular membranes, particularly in the endoplasmic reticulum, where they play a modulatory role in 2+ intracellular Ca signaling. Sigma1 receptors also play a modulatory role in the activity of some ion channels and in sev- eral neurotransmitter systems, mainly in glutamatergic neurotransmission. In accordance with their widespread modula- tory role, 1 receptor ligands have been proposed to be useful in several therapeutic fields such as amnesic and cognitive deficits, depression and anxiety, schizophrenia, analgesia, and against some effects of drugs of abuse (such as cocaine and methamphetamine). -

PCP Oral Fluid
Neogen Corporation 944 Nandino Blvd., Lexington KY 40511 USA 800/477-8201 USA/Canada | 859/254-1221 Fax: 859/255-5532 | E-mail: [email protected] | Web: www.neogen.com/Toxicology PHENCYCLIDINE (PCP) ORAL FLUID KIT ELISA KIT INSTRUCTIONS PRODUCT # 120419 & 120415 (RTU) FORENSIC USE ONLY INTENDED USE: For the determination of trace quantities of Phenylcyclidine (PCP) in human oral fluid. This assay was designed to be compatible with the Neogen NeoSal™ Oral Fluid Collection Device. DESCRIPTION Neogen Corporation’s Phenylcyclidine (PCP) ELISA (Enzyme-Linked ImmunoSorbent Assay) test kit is a qualitative one-step kit designed for use as a screening device for the detection of drugs and/or their metabolites. The kit was designed for screening purposes and is intended for forensic use only. It is recommended that all suspect samples be confirmed by a quantitative method such as gas chromatography/mass spectrometry (GC/MS). ASSAY PRINCIPLES Neogen Corporation’s test kit operates on the basis of competition between the drug or its metabolite in the sample and the drug-enzyme conjugate for a limited number of antibody binding sites. First, the sample or control is added to the microplate. Next, the drug-enzyme conjugate is added and the mixture is incubated for 45 minutes at room temperature. During this incubation, the drug in the sample or the drug-enzyme conjugate binds to antibody immobilized in the microplate wells. After incubation, the plate is washed to remove any unbound sample or drug-enzyme conjugate. The presence of bound drug-enzyme conjugate is recognized by the addition of K-Blue® Substrate (TMB). -

Modulation of Asic1a Function by Sigma-1 Receptors: Physiological and Pathophysiological Implications
University of South Florida Scholar Commons Graduate Theses and Dissertations Graduate School 2-27-2009 Modulation of ASIC1a Function by Sigma-1 Receptors: Physiological and Pathophysiological Implications Yelenis Herrera University of South Florida Follow this and additional works at: https://scholarcommons.usf.edu/etd Part of the American Studies Commons Scholar Commons Citation Herrera, Yelenis, "Modulation of ASIC1a Function by Sigma-1 Receptors: Physiological and Pathophysiological Implications" (2009). Graduate Theses and Dissertations. https://scholarcommons.usf.edu/etd/2011 This Dissertation is brought to you for free and open access by the Graduate School at Scholar Commons. It has been accepted for inclusion in Graduate Theses and Dissertations by an authorized administrator of Scholar Commons. For more information, please contact [email protected]. Modulation of ASIC1a Function by Sigma-1 Receptors: Physiological and Pathophysiological Implications by Yelenis Herrera A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Medical Sciences Department of Molecular Pharmacology and Physiology College of Medicine University of South Florida Major Professor: Javier Cuevas, Ph.D. Keith R. Pennypacker, Ph.D. Eric S. Bennett, Ph.D. Jay B. Dean, Ph.D. Alison Willing, Ph.D. ZhiGang Xiong, Ph.D. Date of Approval: February 27, 2009 Keywords: intracellular calcium, whole-cell currents, AKAP150, calcineurin, G protein, neurotransmission, glutamate, VGCC, NMDA receptor © Copyright 2009, Yelenis Herrera DEDICATION Those who have inspired me throughout my life and scientific career are those that I love the most. This dissertation is dedicated to them - my husband and family. I would like to thank my Mom and Dad for giving me the opportunity to be free, succeed and pursue my education. -

Mechanisms of Cocaine Abuse and Toxicity
Mechanisms of Cocaine Abuse and Toxicity U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol, Drug Abuse, and Mental Health Administration I Mechanisms of Cocaine Abuse and Toxicity Editors: Doris Clouet, Ph.D. Khursheed Asghar, Ph.D. Roger Brown, Ph.D. Division of Preclinical Research National Institute on Drug Abuse NIDA Research Monograph 88 1988 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse 5600 Fishers Lane Rockville, MD 20857 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 NIDA Research Monographs are prepared by the research divisions of the National Institute on Drug Abuse and published by its Office of Science. The primary objective of the series is to provide critical reviews of research problem areas and techniques, the content of state-of-the-art conferences, and integrative research reviews. Its dual publication emphasis is rapid and targeted dissemination to the scientific and professional community. Editorial Advisors MARTIN W. ADLER, Ph.D. MARY L. JACOBSON Temple University School of Medicine National Federation of Parents for Philadelphia,Pennsylvania Drug-Free Youth Omaha, Nebraska SYDNEY ARCHER, Ph.D. Rensselaer Polytechnic lnstitute Troy, New York REESE T. JONES, M.D. Langley Porter Neuropsychiatric lnstitute RICHARD E. BELLEVILLE, Ph.D. San Francisco, California NB Associates, Health Sciences RockviIle, Maryland DENISE KANDEL, Ph.D. KARST J. BESTEMAN College of Physicians and Surgeons of Alcohol and Drug Problems Association Columbia University of North America New York, New York Washington, D.C. GILBERT J. -

Curriculum Vitae
Professor Dragan M. Djuric, MD, PhD Department: Institute of Medical Physiology “Richard Burian”, School of Medicine, University of Belgrade Address: Višegradska 26/II, 11000 Belgrade, Serbia Phone: +381 11 36 07 074 Fax: +381 11 36 11 261 E-mail: [email protected] CURRICULUM VITAE DRAGAN M. DJURIC, MD, PhD Professor and Chair, Institute of Medical Physiology “Richard Burian”, School of Medicine, University of Belgrade, President, Serbian Physiological Society Assembly, President, Serbian Association for Arteriosclerosis, Thrombosis and Vascular Biology Research Office: Institute of Medical Physiology “Richard Burian” School of Medicine, University of Belgrade Visegradska 26/II, 11000 Belgrade Republic of Serbia Phone: +381 11 36 07 074 Fax: +381 11 36 11 261 E-mail: [email protected] Personal Data Birth date: September 13, 1961 Place of birth: Krusevac, Serbia Language: English Academic Degrees MD Title: School of Medicine, University of Belgrade Graduated: 1987 Internship: School of Medicine, University of Belgrade Residency: Training in Internal Medicine, Clinical Centre of Serbia, Belgrade Certification: Board Eligible in Internal Medicine (1996); Board Certified in Clinical Physiology (2007) PhD Title: 1993, School of Medicine, University of Belgrade Undergraduate Training 1986 Department of Surgery, Ulleval Hospital, Oslo, Norway Postgraduate Study and Education 1989-1991 Endocrinology, School of Medicine, University of Belgrade 1991-1993 Experimental Physiology, School of Medicine, University of Belgrade Postdoctoral Training 1998 -

Sigma, PCP, and NMDA Receptors
National Institute on Drug Abuse RESEARCH MONOGRAPH SERIES Sigma, PCP, and NMDA Receptors 133 U.S. Department of Health and Human Services • Public Health Service • National Institutes of Health Sigma, PCP, and NMDA Receptors Editors: Errol B. De Souza, Ph.D. Addiction Research Center National Institute on Drug Abuse Doris Clouet, Ph.D. Division of Basic Research National Institute on Drug Abuse Edythe D. London, Ph.D. Addiction Research Center National Institute on Drug Abuse Research Monograph 133 1993 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Substance Abuse and Mental Health Services Administration National Institute on Drug Abuse 5600 Fishers Lane Rockville, MD 20857 ACKNOWLEDGMENT This monograph is based on the papers and discussions from a technical review on “Sigma, PCP, and NMDA Receptors Systems” held on September 27-28, 1989, in Baltimore, MD. The review meeting was sponsored by the National Institute on Drug Abuse. COPYRIGHT STATUS The National Institute on Drug Abuse has obtained permission from the copyright holders to reproduce certain previously published material as noted in the text. Further reproduction of this copyrighted material is permitted only as part of a reprinting of the entire publication or chapter. For any other use, the copyright holder’s permission is required. All other material in this volume except quoted passages from copyrighted sources is in the public domain and may be used or reproduced without permission from the Institute or the authors. Citation of the source is appreciated. Opinions expressed in this volume are those of the authors and do not necessarily reflect the opinions or official policy of the National Institute on Drug Abuse or any other part of the Department of Health and Human Services.