Simeprevir, Faldaprevir and Sofosbuvir
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Faldaprevir, Pegylated Interferon, and Ribavirin for Treatment-Naïve HCV Genotype-1: Pooled Analysis of Two Phase 3 Trials
Faldaprevir, pegylated interferon and ribavirin. , 2016; 15 (3): 333-349 333 ORIGINAL ARTICLE May-June, Vol. 15 No. 3, 2016: 333-349 The Official Journal of the Mexican Association of Hepatology, the Latin-American Association for Study of the Liver and the Canadian Association for the Study of the Liver Faldaprevir, pegylated interferon, and ribavirin for treatment-naïve HCV genotype-1: pooled analysis of two phase 3 trials Donald M. Jensen,1 Tarik Asselah,2 Douglas Dieterich,3 Graham R. Foster,4 Mark S. Sulkowski,5 Stefan Zeuzem,6 Parvez Mantry,7 Eric M. Yoshida,8 Christophe Moreno,9 Denis Ouzan,10 Mark Wright,11 Luis E. Morano,12 Robert Buynak,13 Marc Bourlière,14 Tarek Hassanein,15 Shuhei Nishiguchi,16 Jia-Horng Kao,17 Masao Omata,18 Seung W. Paik,19 David K. Wong,20 Edward Tam,21 Kelly Kaita,22 S. Victor Feinman,23 Jerry O. Stern,24 Joseph Scherer,24 Anne-Marie Quinson,24 Florian Voss,25 John-Paul Gallivan,25 Wulf O. Böcher,25 Peter Ferenci26 1 University of Chicago Medicine, Chicago, IL, USA. 2 Hôpital Beaujon, APHP, University Paris-Diderot and INSERM CRB3, Clichy, France. 3 Icahn School of Medicine at Mount Sinai, New York, NY, USA. 4 Queen Mary University of London, London, UK. 5 Johns Hopkins University School of Medicine, Baltimore, MD, USA. 6 J.W.Goethe University Hospital, Frankfurt, Germany. 7 The Liver Institute at Methodist Dallas Medical Center, Dallas, TX, USA. 8 University of British Columbia, Vancouver, BC, Canada. 9 CUB Hôpital Erasme, Université Libre de Bruxelles, Brussels, Belgium. 10 Institut Arnault Tzanck, St. -

Faldaprevir Combined with Peginterferon Alfa2a and Ribavirin In
Faldaprevir Combined With Peginterferon Alfa-2a and Ribavirin in Chronic Hepatitis C Virus Genotype-1 Patients With Prior Nonresponse: SILEN-C2 Trial Mark S. Sulkowski,1 Marc Bourlie`re,2 Jean-Pierre Bronowicki,3 Tarik Asselah,4 Jean-Michel Pawlotsky,5 Stephen D. Shafran,6 Stanislas Pol,7 Stefan Mauss,8 Dominique Larrey,9 Yakov Datsenko,10 Jerry O. Stern,11 George Kukolj,12 Joseph Scherer,11 Gerhard Nehmiz,10 Gerhard G. Steinmann,10 and Wulf O. B€ocher13 Faldaprevir (BI 201335) is a potent, hepatitis C virus (HCV) NS3/4A protease inhibitor. In all, 290 noncirrhotic HCV genotype (GT)-1 patients with prior null (<1log10 viral load [VL] drop at any time on treatment) or partial response (1log10 VL drop but never undetectable on treatment) were randomized 2:1:1 to receive 48 weeks of peginterferon alfa-2a and ribavirin (PegIFN/RBV) in combination with faldaprevir 240 mg once daily (QD) with 3 days PegIFN/RBV lead-in (LI), 240 mg QD without LI, or 240 mg twice daily (BID) with LI. Patients in the 240 mg QD/LI group achieving maintained rapid virologic response (mRVR; VL <25 IU/mL [Roche TaqMan] at week 4 and undetectable at weeks 8 to 20) were rerandomized to cease all treatment at week 24 or continue PegIFN/RBV up to week 48. Sustained virologic response (SVR) rates were 32%, 50%, and 42% in prior partial responders, and 21%, 35%, and 29% in prior null responders in the faldaprevir 240 mg QD/LI, 240 mg QD, and 240 mg BID/LI groups, respectively. -
UNO Template
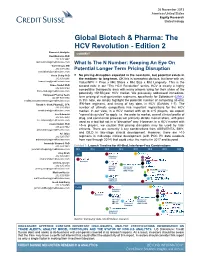
26 November 2013 Americas/United States Equity Research Biotechnology Global Biotech & Pharma: The HCV Revolution - Edition 2 Research Analysts COMMENT Ravi Mehrotra PhD 212 325 3487 [email protected] What Is The N Number: Keeping An Eye On Vamil Divan, MD 212 538 5394 Potential Longer Term Pricing Disruption [email protected] Koon Ching PhD ■ No pricing disruption expected in the near-term, but potential exists in 212 325 6286 the medium- to long-term. OK this is somewhat obvious, but bear with us: [email protected] Value/NPV = Price x Mkt Share x Mkt Size x Mkt Longevity. This is the Bruce Nudell PhD second note in our "The HCV Revolution" series. HCV is clearly a highly 212 325 9122 competitive therapeutic area with many players vying for their share of the [email protected] potentially >$15B/year HCV market. We previously addressed immediate- European Pharma Team 44 207 888 0304 term pricing of next-generation regimens, specifically for Sofosbuvir (LINK). [email protected] In this note, we simply highlight the potential number of competing all-oral, Ronak H. Shah, Pharm.D., CFA IFN-free regimens, and timing of key data, in HCV (Exhibits 1-7). The 212 325 9799 number of ultimate competitors has important implications for the HCV [email protected] market. In our view, in a HCV market with up to 4−5 players, we expect Lee Kalowski "normal drug rules" to apply: i.e. the order to market, overall clinical profile of 212 325 9683 drug, and commercial prowess will primarily dictate market share, with price [email protected] used as a tool but not in a "disruptive" way. -

Startverso4 PHASE III TRIAL of FALDAPREVIR PLUS PEGYLATED INTERFERON Α-2A and RIBAVIRIN in PATIENTS with HIV and HCV GENOTYPE-1 CO-INFECTION
STARTVerso4 PHASE III TRIAL OF FALDAPREVIR PLUS PEGYLATED INTERFERON α-2a AND RIBAVIRIN IN PATIENTS WITH HIV AND HCV GENOTYPE-1 CO-INFECTION JK Rockstroh1, M Nelson2, V Soriano3, K Arastéh4, J Guardiola5, S Bhagani6, J Mallolas7, C Tural8, M Puoti9, P Ingiliz10, M Battegay11, MK Jain12, M Núñez13, K Marks14, J Kort15, JO Stern15, R Vinisko15, M Manero16, D Dieterich17, on behalf of the STARTVerso4 Study Group 1University of Bonn, Bonn, Germany; 2Chelsea and Westminster Hospital, London, UK; 3Hospital Carlos III, Madrid, Spain; 4EPIMED, Vivantes Auguste-Viktoria Hospital, Berlin, Germany; 5Hospital de la Santa Creu i Sant Pau, Barcelona, Spain; 6Royal Free Hospital, London, UK; 7Hospital Clínic, Barcelona, Spain; Jürgen K. Rockstroh 1099 8Hospital Universitari Germans Trias i Pujol, Barcelona, Spain; 9AO Ospedale Niguarda Cà Granda, Milan, Italy; 10Medizinisches Infektiologiezentrum Berlin (MIB), Berlin, Germany; 11Division of Infectious Diseases and Hospital Epidemiology, Basel, Switzerland; 12UT Southwestern Medical Center, Dallas, TX, USA; 13Wake Forest University, Winston-Salem, NC, USA; 14Weill Cornell Medical College, New York, NY, USA; 15Boehringer Ingelheim Pharmaceuticals, Inc., Ridgefield, CT, USA; 16Boehringer Ingelheim España S.A., Barcelona, Spain; 17Mount Sinai School of Medicine, New York, NY, USA [email protected] BACKGROUND RESULTS EFFICACY FIGURE 4e. SVR4 by ART (total population) TABLE 5. AE summary ●● SVR4 was achieved by 74% of patients overall (Figure 3). FDV 120 mg FDV 240 mg + PR + PR Total ●● Faldaprevir (FDV) is a potent inhibitor of HCV NS3/4A.1 PATIENTS - SVR4 rates were comparable across FDV doses and durations of treatment. 24 weeks Total FDV + PR a ●● 1 n (%) (N=123) (N=185) (N=308) FDV has antiviral activity against HCV genotypes (GT) 1, 4, 5, and 6 in vitro. -
Design and Synthesis of Hepatitis C Virus NS3 Protease Inhibitors
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Pharmacy 197 Design and Synthesis of Hepatitis C Virus NS3 Protease Inhibitors Targeting Different Genotypes and Drug-Resistant Variants ANNA KARIN BELFRAGE ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6192 ISBN 978-91-554-9166-6 UPPSALA urn:nbn:se:uu:diva-243317 2015 Dissertation presented at Uppsala University to be publicly examined in B41 BMC, Husargatan 3, Uppsala, Friday, 27 March 2015 at 09:15 for the degree of Doctor of Philosophy (Faculty of Pharmacy). The examination will be conducted in Swedish. Faculty examiner: Ulf Ellervik (Lunds tekniska högskola). Abstract Belfrage, A. K. 2015. Design and Synthesis of Hepatitis C Virus NS3 Protease Inhibitors. Targeting Different Genotypes and Drug-Resistant Variants. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Pharmacy 197. 108 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-554-9166-6. Since the first approved hepatitis C virus (HCV) NS3 protease inhibitors in 2011, numerous direct acting antivirals (DAAs) have reached late stages of clinical trials. Today, several combination therapies, based on different DAAs, with or without the need of pegylated interferon-α injection, are available for chronic HCV infections. The chemical foundation of the approved and late-stage HCV NS3 protease inhibitors is markedly similar. This could partly explain the cross-resistance that have emerged under the pressure of NS3 protease inhibitors. The first-generation NS3 protease inhibitors were developed to efficiently inhibit genotype 1 of the virus and were less potent against other genotypes. The main focus in this thesis was to design and synthesize a new class of 2(1H)-pyrazinone based HCV NS3 protease inhibitors, structurally dissimilar to the inhibitors evaluated in clinical trials or approved, potentially with a unique resistance profile and with a broad genotypic coverage. -

Incidence and Predictors of Hepatocellular Carcinoma In
Massimo Puoti Dept. of Infectious Diseases AO Ospedale Niguarda Cà Granda Milan, Italy The revolving alphabet soup of hepatitis viral infections Hepatitis C drug therapy – present© by and author future ESCMID Online Lecture Library Hepatitis C drug therapy • The present • The future © by author ESCMID Online Lecture Library Anti HCV agents Interferon and Ribavirin © by author ESCMID Online Lecture Library Viral Load vs. Time 1.E+08 • Lack of sensitivity to IFN 1.E+07 • Insufficient antiviral activity 1st phase 1.E+06 2nd phase • Defective clearance of DNA (cp/ml) DNA - 1.E+05 3rd phase infected cells HBV 1.E+04 4th phase 1.E+03 -7 7 21 35 ©49 by63 author77 91 105 119 133 147 161 175 Time (days) • In theESCMID first 2-3 weeks of therapy, Online the viral load Lecturedecline derives mainly Library from the reduction of viral production direct antiviral effect of the drug • Thereafter the viremia decline derives mainly from the clearance of infected cell Colombatto P et al.. Antiv Ther, 2003 Patterns of Virologic Response 7 Null response [1] 6 5 IU/mL) 10 4 Partial response 3 Relapse 40% chance 2 of SVR with © by author pegIFN/RBV[2] HCV RNA (log HCV RNA 1 Undetectable RVR EVR EOT SVR 0 ESCMID-8 -4 -2 0 4Online 8 12 16 Lecture20 24 32 40 48Library 52 60 72 Wks After Start of Therapy 1. Ghany MG, et al. Hepatology. 2009;49:1335-1374. 2. McHutchison JG, et al. N Engl J Med. 2009;361:580-593. WHAT WE HAVE LEARNED ABOUT TREATMENT (IFN) FAILURE Response to IFN alfa depends on : . -

HCV Eradication with Direct Acting Antivirals (Daas)?
HCV eradication with direct acting antivirals (DAAs)? Emilie Estrabaud Service d’Hépatologie et INSERM UMR1149, AP-HP Hôpital Beaujon, Paris, France. [email protected] HCV eradication with direct acting antivirals (DAAs)? HCV replication HCV genome and DAAs targets NS3 inhibitors NS5A inhibitors NS5B inhibitors Take home messages HCV viral cycle Asselah et al. Liver Int. 2015;35 S1:56-64. Direct acting antivirals 5’NTR Structural proteins Nonstructural proteins 3’NTR Metalloprotease Envelope Serine protease Glycoproteins RNA Capsid RNA helicase Cofactors Polymerase C E1 E2 NS1 NS2 NS3 NS4A NS4B NS5A NS5B Protease Inhibitors NS5A Inhibitors Polymerase Inhibitors Telaprevir Daclatasvir Nucs Non-Nucs Boceprevir Ledipasvir Simeprevir ABT-267 Sofosbuvir ABT-333 Faldaprevir GS-5816 VX-135 Deleobuvir Asunaprevir Direct Acting Antivirals: 2015 Asselah et al. Liver Int. 2015;35 S1:56-64. Genetic barrier for HCV direct acting antivirals High Nucleos(t)ide 1 mutation= high cost to Analog Inhibitors fitness, 2-3 additional mutations to increase fitness 2 st generation Protease Inhibitors n Non Nucleos(t)ide Analog Inhibitors : NS5 A Inhibitors 1 st generation Protease Inhibitors 1 mutation= low cost to fitness Low Halfon et al. J Hepatol 2011. Vol 55(1):192-206. HCV protease inhibitors (PI) Inhibit NS3/NS4A serine protease responsible for the processing of the polyprotein 1st generation 1st generation, 2nd wave 2nd generation Resistance low low high barrier Genotype activity 1: 1 a< 1b All except 3 all Drug drug Important Less Less interaction Drugs Boceprevir Simeprevir (Janssen) MK-5172 Telaprevir Faldaprevir (BI) ACH-2684 Paritaprevir (ABT-450)/r (AbbVie) Vedroprevir (Gilead) Vaniprevir (Merck) Sovaprevir (Achillion) Asunaprevir (BMS) NS3/NS4A structure Repositioning of helicase domain Self cleavage Lipid Bilayer Inactive Insertion of the Active carboxy-terminal tail Bartenschlager et al. -

Diapositiva 1
Resistencias & Epidemiología Eva Poveda Division of Clinical Virology INIBIC-Complexo Hospitalario Universitario de A Coruña Rapid Evolution of HCV Regimens: Easier to take/tolerate, Short Duration, Pangenotypic, Higher SVR, Eventually Oral for all patients SVR: 70-80% ≥ 90% ≥ 90% 2013 2014 2015 Genotype 2&3 Genotype 2 Genotypes 1-6 P/R SOF+RBV 12 weeks SOF+LPV ± RBV Genotypes 1 Genotype 3 ABT-450+ABT-267+ Telaprevir + P/R SOF+RBV 24 weeks ABT- 333 +RBV Boceprevir + P/R Genotypes 1-4 DCV+ASU SOF+ P/R SOF+DCV Genotypes 1&4 SMV+ P/R HCV Resistance to DAA During DAA-based treatment: ■ Rapid selection of resistance mutation may occur, eventually leading to viral break-through. Kieffer et al. Hepatology 2007; 46:631-9 Pilot-Matias et al. 46th EASL 2011, Abs1107 ■ Several changes at different positions at the NS3 protease, NS5B polymerase, and NS5A protein have been associated with loss of susceptibility to DAAs. Sarrazin et al. Gastroenterology 2010;138:447-62 MainTable 2. Main characteristics characteristics of the genotype of theactivity genotypeand resistance of DAA activity classes. and resistance of DAA classes. Genotype activity Resistance Key resistance mutations NS3 ■ First PI generation: genotypes 1 (1b >1a) Low genetic barrier First PI generation: protease (Telaprevir & Boceprevir) High cross-resistance G1a: R155K, V36M inhibitors G1b: V36M, T54A/S, A156T ■ Second wave and second PI generation: across all but genotype 3 (D168Q) Second wave and second PI generation: (Simeprevir, faldaprevir, vaniprevir, F43S, Q80K, R155K, D168A/E/H/T/V asunaprevir, sovaprevir, MK-5172, ACH-2684) NS5 Across all genotypes High genetic barrier Sofosbuvir*: nucleos(ti)de High cross-resistance G1a: S282T+(I434M) Sofosbuvir displays less antiviral activity G1b: S282T analogues againts genotypes 3 (treatment duration 24 G2a: S282T+(T179A, M289L, I293L, inhibitors weeks of sofosbuvir+RBV). -

Twelve-Week Ravidasvir Plus Ritonavir-Boosted Danoprevir And
bs_bs_banner doi:10.1111/jgh.14096 HEPATOLOGY Twelve-week ravidasvir plus ritonavir-boosted danoprevir and ribavirin for non-cirrhotic HCV genotype 1 patients: A phase 2 study Jia-Horng Kao,* Min-Lung Yu,† Chi-Yi Chen,‡ Cheng-Yuan Peng,§ Ming-Yao Chen,¶ Huoling Tang,** Qiaoqiao Chen** and Jinzi J Wu** *Graduate Institute of Clinical Medicine and Hepatitis Research Center, National Taiwan University College of Medicine and Hospital, ¶Division of Gastroenterology, Department of Internal Medicine, Taipei Medical University Shuang Ho Hospital, Taipei, †Division of Hepatobiliary, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung, ‡Division of Gastroenterology, Department of Internal Medicine, Chia-Yi Christian Hospital, Chiayi, and §Division of Hepatogastroenterology, Department of Internal Medicine, China Medical University Hospital, Taichung, Taiwan; and **Ascletis BioScience Co., Ltd., Hangzhou, China Key words Abstract danoprevir, efficacy, hepatitis C, interferon free, ravidasvir. Background and Aim: The need for all-oral hepatitis C virus (HCV) treatments with higher response rates, improved tolerability, and lower pill burden compared with Accepted for publication 9 January 2018. interferon-inclusive regimen has led to the development of new direct-acting antiviral agents. Ravidasvir (RDV) is a second-generation, pan-genotypic NS5A inhibitor with high Correspondence barrier to resistance. The aim of this phase 2 study (EVEREST study) was to assess the ef- Jia-Horng Kao, Graduate Institute of Clinical ficacy and safety of interferon-free, 12-week RDV plus ritonavir-boosted danoprevir Medicine and Hepatitis Research Center, (DNVr) and ribavirin (RBV) regimen for treatment-naïve Asian HCV genotype 1 (GT1) National Taiwan University College of Medicine patients without cirrhosis. and Hospital, 7 Chung-Shan South Road, Taipei Methods: A total of 38 treatment-naïve, non-cirrhotic adult HCV GT1 patients were en- 10002, Taiwan. -

Caracterización Molecular Del Perfil De Resistencias Del Virus De La
ADVERTIMENT. Lʼaccés als continguts dʼaquesta tesi queda condicionat a lʼacceptació de les condicions dʼús establertes per la següent llicència Creative Commons: http://cat.creativecommons.org/?page_id=184 ADVERTENCIA. El acceso a los contenidos de esta tesis queda condicionado a la aceptación de las condiciones de uso establecidas por la siguiente licencia Creative Commons: http://es.creativecommons.org/blog/licencias/ WARNING. The access to the contents of this doctoral thesis it is limited to the acceptance of the use conditions set by the following Creative Commons license: https://creativecommons.org/licenses/?lang=en Programa de doctorado en Medicina Departamento de Medicina Facultad de Medicina Universidad Autónoma de Barcelona TESIS DOCTORAL Caracterización molecular del perfil de resistencias del virus de la hepatitis C después del fallo terapéutico a antivirales de acción directa mediante secuenciación masiva Tesis para optar al grado de doctor de Qian Chen Directores de la Tesis Dr. Josep Quer Sivila Dra. Celia Perales Viejo Dr. Josep Gregori i Font Laboratorio de Enfermedades Hepáticas - Hepatitis Víricas Vall d’Hebron Institut de Recerca (VHIR) Barcelona, 2018 ABREVIACIONES Abreviaciones ADN: Ácido desoxirribonucleico AK: Adenosina quinasa ALT: Alanina aminotransferasa ARN: Ácido ribonucleico ASV: Asunaprevir BOC: Boceprevir CCD: Charge Coupled Device CLDN1: Claudina-1 CHC: Carcinoma hepatocelular DAA: Antiviral de acción directa DC-SIGN: Dendritic cell-specific ICAM-3 grabbing non-integrin DCV: Daclatasvir DSV: Dasabuvir -

Stamp-V3 1..249
23 March 2016 Volume 23 Supplement 1 S1 Volume 23 Volume Supplement 1 P ages A1–A262 ages EUROPEAN JOURNAL OF HOSPITAL PHARMACY OF HOSPITAL JOURNAL EUROPEAN ABSTRACT BOOK 21st Congress of the EAHP 16-18 March 2016 Vienna, Austria March 2016 March Contents Volume 23 Supplement 1 | EJHP March 2016 Abstracts from the EAHP 2016 Congress A1 Clinical pharmacy A172 Other hospital pharmacy topics A104 Drug distribution A178 Pharmacokinetics and pharmacodynamics A118 Drug information and pharmacotherapy A195 Production and preparation A158 General management A214 Patient safety and risk management A167 International posters A250 Author index POSTER AWARD NOMINEES Presentations on Wednesday, 16 March, 14:00–15:30, Room 93 Time Poster number Poster nominee oral presentations Author 14:00 DD-021 Medicine supply chain of a central pharmacy: risk mapping F Charra shortage 14:10 PP-001 Contamination with cytotoxic drugs in the workplace – E Korczowska ESOP pilot study 14:20 PP-039 Double checking manipulations for complex and/or high A Alcobia Martins risk preparations 14:30 CP-055 The clinical pharmacist resolves medication related E Tudela-Lopez problems in cranio, maxillofacial and oral surgery patients 14:40 CP-085 The impact of pharmacist interventions on safety M Tovar Pozo and cost savings 14:50 CP-219 Effectiveness and safety of switching to dual antiretroviral J Luis Revuelta therapy in a treatment experienced HIV cohort 15:00 DD-027 Implementation and evaluation of an appointment based F J Alvarez Manceñido model for outpatients attended in -

Response-Guided Therapy in Patients with Genotype 1 Hepatitis C Virus: Current Status and Future Prospects Eric J Lawitz and Fernando E Membreno
bs_bs_banner doi:10.1111/jgh.12632 REVIEW Response-guided therapy in patients with genotype 1 hepatitis C virus: Current status and future prospects Eric J Lawitz and Fernando E Membreno The Texas Liver Institute, University of Texas Health Science Center at San Antonio, San Antonio, Texas, USA Key words Abstract direct-acting antiviral, HCV RNA, protease inhibitors, response-guided therapy. On-treatment responses to antiviral therapy are used to determine duration of therapy in patients being treated for genotype 1 hepatitis C virus infection. Such use of response- Accepted for publication 9 March 2014. guided therapy has successfully reduced exposure of patients to the side-effects of pegylated interferon and ribavirin without jeopardizing overall treatment success. Correspondence Response-guided therapy is an integral part of treatment using the current standard treat- Dr Eric J Lawitz, 607 Camden Street, ments involving the direct-acting antiviral (DAA) agents—boceprevir or telaprevir— University of Texas Health Science Center, combined with pegylated interferon/ribavirin. Improvements in our understanding of the San Antonio, TX 78215, USA. kinetics of viral load during antiviral therapy have shown us that more potent suppression Email: [email protected] of viral replication increases the rate of viral eradication, providing impetus for the development of more potent DAAs. Emerging results from clinical trials of these agents— including trials of interferon-free DAA combinations—suggest that very high rates of viral eradication are achievable, even in patients who failed to respond to previous courses of interferon-based therapy. Furthermore, because of these high rates of treatment success, on-treatment assessment of viral response may become unnecessary.