Solomon Islands Health System Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gender and Investment Climate Reform Assessment in Partnership with Ausaid
IFC Advisory Services in East Asia and the Pacific Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Solomon Islands Gender and Investment Climate Reform Assessment In Partnership with AusAID Public Disclosure Authorized January 2010 Sonali Hedditch & Clare Manuel © 2010 International Finance Corporation 2121 Pennsylvania Avenue, NW Washington DC 20433USA Telephone: 202-473-1000 Internet: www.ifc.org The findings, interpretations, and conclusions expressed herein are those of the author(s) and do not necessarily reflect the views of the Executive Directors of IFC or the governments they represent. IFC does not guarantee the accuracy of the data included in this work. The boundaries, colors, denominations, and other information shown on any map in this work do not imply any judgment on the part of IFC concerning the legal status of any territory or the endorsement or acceptance of such boundaries. Gender and Investment Climate Reform Assessment Solomon Islands Preface and Acknowledgements This Report is the result of collaboration between the Australian Agency for International Development (AusAID) and the International Finance Corporation (IFC), a member of the World Bank Group. The Report has been produced for: • The Solomon Islands Government, primarily the Ministries of Commerce and Finance: to make recommendations for reform actions for Government to further enable women in Solomon Islands to participate effectively in the country’s economic development. • The International Finance Corporation: to inform its support to the Solomon Islands Regulatory Simplification and Investment Policy and Promotion Program and ensure that gender issues are incorporated in the program’s design and implementation. • AusAID: to assist development programs to mainstream gender and to enable women to benefit equitably from improvements in the business climate. -

Malaita Province
Environmental Assessment Document Project Number: 46014 June 2013 Solomon Islands: Provincial Renewable Energy Project Fiu River Hydropower Project – Malaita Province Initial Environmental Examination The Initial Environmental Examination is a document of the borrower. The views expressed herein do not necessarily represent those of ADB’s Board of Directors, Management or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. ABBREVIATIONS ADB Asian Development Bank AMNH American Museum of Natural History BMP Building Material Permit CBSI Central Bank of Solomon Islands CDM Clean development mechanism CITES Convention on International Trade in Endangered Species DSC Design and supervision consultant EA Executing agency ECD Environment and Conservation Division (of MECDM) EBRD European Bank for Reconstruction and Development EIS Environmental Impact Statement EHSG Environmental Health and Safety Guidelines (of World Bank Group) EMP Environmental Management Plan EPC Engineer Procure and Construct ESP Environmental Sector Policy FRI National Forest Resources Inventory GDP Gross Domestic Product GFP Grievance focal point GNI Gross National Income GRM Grievance Redress Mechanism HDPE High density polyethylene HDR Human Development Report HSP Health and Safety -

Isabel Province
159°15'E 159°30'E 159°45'E 160°00'E Reta Is Malakobo Is Malakobi Is Sesehura Faa Is ISABEL PROVINCE BubulinaBubulinaBubulina Pt PtPt Naghono Is Sesehura Is EAST SOLOMON ISLANDS ((( ((( BoliteiBoliteiBolitei Bani Leghahana Is TOPOGRAPHIC MAP SERIES 2005 wqq AHCAHC SCALE 1:150,000 R api Rar KesuoKesuoKesuo Logging LoggingLogging Camp CampCamp 5 0 10 20 ((( ((( KesuoKesuoKesuo 1 11 (((( (((( R kilometres u KesuoKesuoKesuo Pt PtPt h g e u h Elevation (m) g E Is Anchorage ; Town / Builtup Area Capital Cities -- #(### -- #### 0 to 200 600 to 800 1200 to 1400 (((( MaptainMaptain (((( MaptainMaptain Barrier Reef Coastline Airports Large Settlement (( Sikale 200 to 400 800 to 1000 1400 to 1600 Bay Reef Buildings Medium Settlement ((( (((( (((( 400 to 600 1000 to 1200 GhahiratetuGhahiratetu PtPt Rivers / Lake Roads Small Settlement (((( GhahiratetuGhahiratetu PtPt SisigaSisigaSisiga Pt PtPt #### r Mountains f Tracks Unknown Settlement #### ve Ghatere qq i ((( R ((( SisigaSisigaSisiga e Bay Depth (m) al qq ik NadinaNadinaNadina Pt PtPt NAPNAPw Swamp Trail Education Facilities qq S NadinaNadinaNadina Pt PtPt ver 0 to 100 1000 to 2000 3000 to 4000 re Ri Ghasetatauro Rock Is Ghate Orchard Bridges } Health Facilities w SoviriSoviriSoviri Pt PtPt Kes uo 100 to 1000 2000 to 3000 4000 to 5000 C Crop Language Areas o A A ve Ghehe Or Estrella Bay Grid...................................Longitude/Latitude WGS84 Caution: The depiction of an area name on this map is not to be taken as evidence of customary land ownership. Ghehe Anchorage SalenaSalenaSalena Pt PtPt Projection................................................Geographical ; Prepared, printed and published by the Ministry of Lands, Housing and Survey based upon reductions of Australian Department of #(#(#(#( ((((SakalenaSakalenaSakalena Spheriod..........................................................WGS84 #(#(#(#( ((((SakalenaSakalenaSakalena #(#(#(#( DovanareDovanare Defence data. -

Indigenous People Development of SIRA Executive
Social Assessment- Indigenous People Development of SIRA Executive: People who will be involved in training and capacity building and setting up of SIRA. Indigenous people of the Project Area Solomon Islands The Solomon Islands is one of the Melanesian countries in the Pacific Region. It is inhabited by more than 500,000 people. The population consists of the three major races, the Polynesians, Micronesian and the Melanesians. Inter-marriage to Europeans and Asians has accounts for certain percentage of the total population as well. There are 9 main Provinces scattered across the ocean close to Vanuatu and PNG and more than 1000 small Islands and Islets formed by volcanic activity thousands of years ago. The Islands are mainly volcanic and raised limestone Islands. The country is known for its pristine forest and marine resources as the centre of Biodiversity hot spots next to PNG and some South East Asian countries like Indonesia. However over-harvesting, unsustainable logging and prospecting (mining) are continuous and emerging threats to the biodiversity. Conservation and resource management programs are in placed to ease some of the negative impacts impose by these threats. Methods used by communities are integrating traditional knowledge and modern science to protect the resources. Most of these programs however can be found in most remote areas of the country, which is very challenging. Despite the challenges, efforts have been made in encouraging networking and partnership to manage the challenges and utilize the potentials available. Thus Solomon Islands Ranger Association (SIRA) was established and intended to play the role of supporting the local village rangers that employed by Community- based Organization (CBOs). -
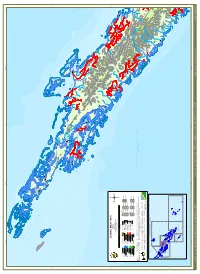
ISABEL PROVINCE V G #### I #(### H #### R I
158°00'E 158°15'E 158°30'E 158°45'158°45'E 159°00'E Suki Is Maduko Reef Is Dughai shoal Malaghara Is LaveLaveLave Pt PtPt Kolohirio Is Nohabuna Is GahuruGahuru PtPt Paregho Shoal M Pareipoga Is Bates Is Telenetera Is Zaka Is Malakobi Is Remark Is A Kologilo Passage Sibau Is N Ghebira Is ge I ssa Kologilo Is Popu Is pa pu P A K A K A L E Po N BikoliaBikoliaBikolia Pt PtPt Hihibana Is Kologhose Is G Zabana Is Korapagho Is S Kale Is T ZABANA Vakao Is Arnavon Is R MT BEAUMONT Kukudaka Reef P A OPU C HANNE L Gateghe Is Kerehikapa Is I T Viketonggana Is ((( KupikoloKupikoloKupikolo Sesehura Ite Is ((( KupikoloKupikoloKupikolo ! KupikoloKupikoloKupikolo ! MT SEARS Golora Is (((( Sesehura Fa Is (((( KerehikapaKerehikapaKerehikapa Rapita Is (((( (((( RitamalaRitamala V A H A (((( ValidoValidoValido Pt PtPt (((( ValidoValidoValido Pt PtPt Legaha Is (((( Higere Is Retu Is Kakatina Is Sekoa Reef Hataheta Is Kumarara Hira Is !! Sogumao Ite Is ! Kumarara Is ! Kia Hetaheta Is Sogomauhiti Is IsaisaoIsaisaoIsaisaoIsaisao Pt PtPtPt Bay 7°30'S IsaisaoIsaisaoIsaisaoIsaisao Pt PtPtPt 7°30'S Sogumao Is Libeiena Is Zaosodu Reef E M A LitunaoLitunaoLitunao Pt PtPt #### #(### T O B I ####B A BARORA FA ((( D ((( TobiTobiTobi A Penrose TobiTobiTobi H Omona Is Zaoponoe Reef Patches #(### A Z A M O T E #### I R O Paenaha Fa Is Paenaha Ite Is V A R U K O I L O Ghizunabeana BoeBoeBoe Pt PtPt Ghanitapi Reef Passage P A Z E G H E R E Ghahipakagili Reef Memehana Fa Is Hulbrow Is Bitters Is B A H A N A Draper Is #### Memehana ite Is #(### PaehenaPaehenaPaehena Pt PtPt -

Solomon Islands Fisheries Bibliography
Solomon Islands Fisheries Bibliography Robert Gillett March 1987 Document 87/1 FAO/UNDP Regional Fishery Support Programme TABLE of CONTENTS I. Introduction ............................................................................................ iii II. Location of reference ............................................................................ v III. References listed alphabetically by author ....................................... 1 IV. References listed by subject .............................................................. 27 Aquaculture ............................................................................... 27 Annual reports ........................................................................... 27 Baitfish ....................................................................................... 28 Beche-de-mer ........................................................................... 29 Boats and Boatbuilding.............................................................. 29 Bottomfish ................................................................................. 30 Charts, Topography, and Boundaries ....................................... 31 Computer ................................................................................... 32 Coral .......................................................................................... 32 Crayfish-lobster.......................................................................... 32 Fish handling and processing .................................................. -

Solomon Islands Blooming Flower Industry
Solomon Islands blooming flower industry. A smallholder’s dream November 2009 Solomon Islands Flower Industry: A Case Study of Agriculture for Growth in the Pacific Agriculture for Growth: learning from experience in the Pacific Solomon Islands Flower Case Study Prepared by Anne Maedia and Grant Vinning The views expressed in this paper do not represent the position of the Food and Agricultural Organization of the United Nations.The depiction employed and the presentation of material in this paper do not imply the expression of any opinion whatsoever on the part of the Food and Agricultural Organisation of the United Nations covering the legal or development status of any country, territory, city or area or its authorities or concerning the deliberations of its frontiers or boundaries. 2 Solomon Islands Flower Industry: A Case Study of Agriculture for Growth in the Pacific Table of contents Acknowledgements 4 Acronyms 5 Executive summary 6 1. Introduction 9 1.1 Case study background 9 1.2 Country economy and agriculture sector 10 1.3 National policy framework 13 1.4 Floriculture sector in Solomon Islands 15 2. Study methodology 17 3. Key findings and discussions 18 3.1 Value chain 18 3.2 SWOT 27 3.3 Technical, institutional, and policy issues 30 3.4 Maintaining competitive advantage 32 3.5 Options for growth 35 4. Conclusions 38 5. Bibliography 39 3 Solomon Islands Flower Industry: A Case Study of Agriculture for Growth in the Pacific Acknowledgements This paper is based on countless interviews and discussions with producers, sellers and buyers of floriculture products at the Honiara Central Market. -
Do Your Part, Disaster Is Everybody's Business
THE SOLOMON ISLANDS NATIONAL EMERGENCY OPERATIONS CENTRE [NEOC] P.O.Box 21 Tel: 00 677 27936/27063/955 Mob: 00 677 749741 Fax: 00 677 27060/24293 Email: [email protected] SI NEOC NATIONAL SITUATIONAL REPORT *************************************************************************************************************** National Emergency Operations Centre National Disaster Management Office Ministry of Environment, Climate Change, Disaster Management and Meteorology Solomon Islands Government Honiara *************************************************************************************************************** SI NEOC SITUATION REPORT NUMBER 08 EVENT SEVERE FLASH FLOODS AND LANDSLIDES Compiled by: Dated issued: Time issued: Next update: George Baragamu 14th April 2014 12:00Hrs 12:00Hrs, 16th April 2014 From: To: N-DOC & NDC Chairs and Members, P-DOC National Emergency Operation Centre and PDC Chairs and Members, PEOCs Honiara Copies: NDMO Stakeholders, Donor Partners, Local Solomon Islands & International NGOs, UN Agencies, Diplomatic Agencies, SIRPF, SIRC and SI Government Ministries and all SI Government Overseas Missions 1. INFORMATION OF PEOPLE Total affected Total affected Total Male Total female Total children population: Household: affected: affected: affected: Estimate 52,000 5465 5188 Number of deaths: No of people missing: No of people Total people displaced: 21 2 injured: 10,653(these are people from 18 : Honiara Evacuation Centres HCC and GP 2 : Isabel combined. Source: SIRC) 2 : Guadalcanal 2. SITUATION DESCRIPTION All new information is in red coloured font. The current situation now is that the floods are now recedes in almost all the flood inundated areas, and humanitarian responses are slowly being delivered by the Government and the Humanitarian Actors. Initial Damaged Assessments (IDA) is now being undertaken by the Honiara City Council and Guadalcanal Province whilst Detail Sectoral Assessments (DSA) is being conducted by the responsible Government Ministries through the relevant Sectors. -
Basic Tables Census Description
Solomon Islands Government Statistical Bulletin 06/2011 REPORT ON 2009 POPULATION & HOUSING CENSUS Basic Tables and Census Description Solomon Islands National Statistics Office Solomon Islands2009 Population and Housing Census CONTENTS Introduction................................................................................................................................................................ iv Map Of Solomon Islands .......................................................................................................................................... vi Section A: Tables1 ...................................................................................................................................................... 1 Summary of main Indicators, Solomon Islands: 2009........................................................................................................................1 I. Population Characteristics.............................................................................................................................................................3 P1.1: Total population and number of private households, by census year and province, Solomon Islands: 1970- 2009 .........................................................................................................................................................................................................................3 P1.2: Total population by sex and number of private households and institutions by urban-rural distribution and ward, -

Solomon Islands
PROTECTING DUGONGS CONSERVING SEAGRASS CHANGE FOR COMMUNITIES COUNTRY PRESENTATION: Solomon Islands INCEPTION WORKSHOP THE GEF DUGONG AND SEAGRASS CONSERVATION PROJECT 20-21 October 2015 Colombo, Sri Lanka Content • Overview: Solomon Islands - Physical, socio-economical and ecological features • Seagrass and Dugongs in Solomon Islands • Our Project : - Solomon Islands Dugong and Seagrass Conservation Project 20 - 21 October 2015 Colombo, Sri Lanka 2 Solomon Islands 20 - 21 October 2015 Colombo, Sri Lanka 3 Bio-physical characteristics • 992 islands • Total land area – 28,000km2 • Total sea area – 1,340,000km2 • Total coral reef area – 3,591km2 • Total mangrove area – 65,000ha • Total seagrass area – 10,000ha • 80% of land is under Customary Tenure (recognized by Constitution). 20 - 21 October 2015 Colombo, Sri Lanka 4 Socio-Economic facts • Population (2009 Census) : Total Urban (Honiara + Provincial Rural centers) 515,870 101,798 (25%) 414,072 (75%) • Annual growth rate: 3.5% • Male/Female Ratio: 1.05: 1 (nearly half of population • Children <15yrs: make up 41 % • Literacy rate: 84.1 % • Poverty lines (UNDP HIES, 2008) Gini Coefficient of inequality Per capita a.e expenditure Gini coefficient National average 0.39 Honiara 0.30 Provincial urban 0.31 Rural areas 0.32 20 - 21 October 2015 Colombo, Sri Lanka 5 • Diverse culture and people: – Melanesians (highest), Polynesians and Micronesians - ~ 80 different languages • Dual economy: formal and informal - Commercial: natural resource dependent on forestry, fisheries, copra, cocoa, etc . Limited manufacturing and processing exist. - Subsistence: fishers, farmers • 85% of people live in rural communities = heavily depend on the land & sea resources for food, income and livelihood. • 61% of all HHs involved in fishing activities; 22% urban and 69% of rural. -

Solomon Islands: Malaita Hub Scoping Report Project Report: AAS-2013-18 Solomon Islands: Malaita Hub Scoping Report
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Aquatic Commons Project Report: AAS-2013-18 Solomon Islands: Malaita Hub Scoping Report Project Report: AAS-2013-18 Solomon Islands: Malaita Hub Scoping Report Authors Acknowledgment Anne-Maree Schwarz, Neil Andrew, Hugh Govan, Daykin Harohau We are grateful to all of the people who took the time to talk and Janet Oeta. with the scoping team and to contribute information, especially Mr. Patrick Taloboe, Mr. Michael Laumani and Ms. Clera Rikimani, the attendees of the stakeholder consultation workshop in Auki This publication should be cited as: and community members of Kwai and Ngongosila. Publication was facilitated by Catherine Jones, Joelle Albert and the Schwarz, A.M., Andrew, N., Govan, H., Harohau, D., Oeta, J. (2013). communications team at WorldFish Penang. Solomon Islands Malaita Hub Scoping Report. CGIAR Research Program on Aquatic Agricultural Systems. Penang, Malaysia This document was prepared through financial support from the Project Report: AAS-2013-18. CGIAR Research Program on Aquatic Agricultural Systems and the Scaling-out community-based marine resource governance in Solomon Islands, Kiribati and Vanuatu Project (FIS/2012/056) funded by the Australian Centre for International Agricultural Research (ACIAR). 2 Table of contents 1. Executive Summary 4 2. Introduction 4 3. Scoping Process 6 4. Description of the three provinces 7 5. Synthesized scoping findings 15 6. Overarching research questions 20 7. Stakeholder consultation workshop 22 8. Target communities for community based research in Malaita 25 9. Institutional context, development programs, investments and key partners in the hub 25 10. -

National Situational Report 08
NATIONAL DISASTER MANAGEMENT OFFICE Ministry of Environment, Climate Change, Disaster Management & Meteorology, Post Office Box 21, Honiara, Solomon Islands | Phone: (677) 27936/7, 27063 |Toll-free: 955 | Fax: (677) 24293 / 27060 | E-mail : [email protected] NATIONAL SITUATIONAL REPORT- 08 Ref: NSR08_05/20 EVENT ID: COVID-19 Contents EVENT: SIG Response to COVID-19 A. HIGHLIGHTS ................................................. 1 DATE OF ISSUE: Wednesday, 27 May 2020 B. CURRENT SITUATION ................................. 2 C. SOLOMON ISLANDS GOVERNMENT TIME OF ISSUE: 1630 Hours RESPONSE ..................................................... 3 APPROVED BY: Chairman, National Disaster Council D. N-DOC SECTOR COMMITTEE UPDATES . 4 E. P-DOC SECTOR RESPONSE ...................... 13 ISSUED BY: National Emergency Operations Centre (NEOC) F. OTHER NATIONAL SUPPORT .................. 14 NEXT UPDATE: Upon availability of new info G. OPERATIONAL CHALLENGES AND GAPS ............................................................. 14 H. RECOMMENDATIONS ............................... 14 I. NEXT UPDATE ............................................ 15 All new information in red coloured font J. ANNEXE ....................................................... 16 A. HIGHLIGHTS The Government established Joint Oversight Committee (OSC) for COVID-19 under the Office GLOBAL SITUATION IN NUMBERS of the Prime Minister and Cabinet maintains its role The numbers are based on WHO Situation Report 127 as in providing strategic direction. at 26th May 2020 (total