Dissertation the Use of Metagenomic Sequencing As
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparative Evolutionary and Phylogenomic Analysis of Avian Avulaviruses 1 to 20
Accepted Manuscript Comparative evolutionary and phylogenomic analysis of Avian avulaviruses 1 to 20 Aziz-ul-Rahman, Muhammad Munir, Muhammad Zubair Shabbir PII: S1055-7903(17)30947-8 DOI: https://doi.org/10.1016/j.ympev.2018.06.040 Reference: YMPEV 6223 To appear in: Molecular Phylogenetics and Evolution Received Date: 1 January 2018 Revised Date: 15 May 2018 Accepted Date: 25 June 2018 Please cite this article as: Aziz-ul-Rahman, Munir, M., Zubair Shabbir, M., Comparative evolutionary and phylogenomic analysis of Avian avulaviruses 1 to 20, Molecular Phylogenetics and Evolution (2018), doi: https:// doi.org/10.1016/j.ympev.2018.06.040 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. Comparative evolutionary and phylogenomic analysis of Avian avulaviruses 1 to 20 Aziz-ul-Rahman1,3, Muhammad Munir2, Muhammad Zubair Shabbir3# 1Department of Microbiology University of Veterinary and Animal Sciences, Lahore 54600, Pakistan https://orcid.org/0000-0002-3342-4462 2Division of Biomedical and Life Sciences, Furness College, Lancaster University, Lancaster LA1 4YG United Kingdomhttps://orcid.org/0000-0003-4038-0370 3 Quality Operations Laboratory University of Veterinary and Animal Sciences 54600 Lahore, Pakistan https://orcid.org/0000-0002-3562-007X # Corresponding author: Muhammad Zubair Shabbir E. -

2020 Taxonomic Update for Phylum Negarnaviricota (Riboviria: Orthornavirae), Including the Large Orders Bunyavirales and Mononegavirales
Archives of Virology https://doi.org/10.1007/s00705-020-04731-2 VIROLOGY DIVISION NEWS 2020 taxonomic update for phylum Negarnaviricota (Riboviria: Orthornavirae), including the large orders Bunyavirales and Mononegavirales Jens H. Kuhn1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Gaya K. Amarasinghe5 · Simon J. Anthony6,7 · Tatjana Avšič‑Županc8 · María A. Ayllón9,10 · Justin Bahl11 · Anne Balkema‑Buschmann12 · Matthew J. Ballinger13 · Tomáš Bartonička14 · Christopher Basler15 · Sina Bavari16 · Martin Beer17 · Dennis A. Bente18 · Éric Bergeron19 · Brian H. Bird20 · Carol Blair21 · Kim R. Blasdell22 · Steven B. Bradfute23 · Rachel Breyta24 · Thomas Briese25 · Paul A. Brown26 · Ursula J. Buchholz27 · Michael J. Buchmeier28 · Alexander Bukreyev18,29 · Felicity Burt30 · Nihal Buzkan31 · Charles H. Calisher32 · Mengji Cao33,34 · Inmaculada Casas35 · John Chamberlain36 · Kartik Chandran37 · Rémi N. Charrel38 · Biao Chen39 · Michela Chiumenti40 · Il‑Ryong Choi41 · J. Christopher S. Clegg42 · Ian Crozier43 · John V. da Graça44 · Elena Dal Bó45 · Alberto M. R. Dávila46 · Juan Carlos de la Torre47 · Xavier de Lamballerie38 · Rik L. de Swart48 · Patrick L. Di Bello49 · Nicholas Di Paola50 · Francesco Di Serio40 · Ralf G. Dietzgen51 · Michele Digiaro52 · Valerian V. Dolja53 · Olga Dolnik54 · Michael A. Drebot55 · Jan Felix Drexler56 · Ralf Dürrwald57 · Lucie Dufkova58 · William G. Dundon59 · W. Paul Duprex60 · John M. Dye50 · Andrew J. Easton61 · Hideki Ebihara62 · Toufc Elbeaino63 · Koray Ergünay64 · Jorlan Fernandes195 · Anthony R. Fooks65 · Pierre B. H. Formenty66 · Leonie F. Forth17 · Ron A. M. Fouchier48 · Juliana Freitas‑Astúa67 · Selma Gago‑Zachert68,69 · George Fú Gāo70 · María Laura García71 · Adolfo García‑Sastre72 · Aura R. Garrison50 · Aiah Gbakima73 · Tracey Goldstein74 · Jean‑Paul J. Gonzalez75,76 · Anthony Grifths77 · Martin H. Groschup12 · Stephan Günther78 · Alexandro Guterres195 · Roy A. -

Differential Features of Fusion Activation Within the Paramyxoviridae
viruses Review Differential Features of Fusion Activation within the Paramyxoviridae Kristopher D. Azarm and Benhur Lee * Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-212-241-2552 Received: 17 December 2019; Accepted: 29 January 2020; Published: 30 January 2020 Abstract: Paramyxovirus (PMV) entry requires the coordinated action of two envelope glycoproteins, the receptor binding protein (RBP) and fusion protein (F). The sequence of events that occurs during the PMV entry process is tightly regulated. This regulation ensures entry will only initiate when the virion is in the vicinity of a target cell membrane. Here, we review recent structural and mechanistic studies to delineate the entry features that are shared and distinct amongst the Paramyxoviridae. In general, we observe overarching distinctions between the protein-using RBPs and the sialic acid- (SA-) using RBPs, including how their stalk domains differentially trigger F. Moreover, through sequence comparisons, we identify greater structural and functional conservation amongst the PMV fusion proteins, as compared to the RBPs. When examining the relative contributions to sequence conservation of the globular head versus stalk domains of the RBP, we observe that, for the protein-using PMVs, the stalk domains exhibit higher conservation and find the opposite trend is true for SA-using PMVs. A better understanding of conserved and distinct features that govern the entry of protein-using versus SA-using PMVs will inform the rational design of broader spectrum therapeutics that impede this process. Keywords: paramyxovirus; viral envelope proteins; type I fusion protein; henipavirus; virus entry; viral transmission; structure; rubulavirus; parainfluenza virus 1. -
Final Rule to List Reticulated Python And
Vol. 80 Tuesday, No. 46 March 10, 2015 Part II Department of the Interior Fish and Wildlife 50 CFR Part 16 Injurious Wildlife Species; Listing Three Anaconda Species and One Python Species as Injurious Reptiles; Final Rule VerDate Sep<11>2014 18:14 Mar 09, 2015 Jkt 235001 PO 00000 Frm 00001 Fmt 4717 Sfmt 4717 E:\FR\FM\10MRR2.SGM 10MRR2 mstockstill on DSK4VPTVN1PROD with RULES2 12702 Federal Register / Vol. 80, No. 46 / Tuesday, March 10, 2015 / Rules and Regulations DEPARTMENT OF THE INTERIOR Services Office, U.S. Fish and Wildlife 3330) to list Burmese (and Indian) Service, 1339 20th Street, Vero Beach, pythons, Northern African pythons, Fish and Wildlife Service FL 32960–3559; telephone 772–562– Southern African pythons, and yellow 3909 ext. 256; facsimile 772–562–4288. anacondas as injurious wildlife under 50 CFR Part 16 FOR FURTHER INFORMATION CONTACT: Bob the Lacey Act. The remaining five RIN 1018–AV68 Progulske, Everglades Program species (reticulated python, boa Supervisor, South Florida Ecological constrictor, green anaconda, [Docket No. FWS–R9–FHC–2008–0015; Services Office, U.S. Fish and Wildlife DeSchauensee’s anaconda, and Beni FXFR13360900000–145–FF09F14000] Service, 1339 20th Street, Vero Beach, anaconda) were not listed at that time and remained under consideration for Injurious Wildlife Species; Listing FL 32960–3559; telephone 772–469– 4299. If you use a telecommunications listing. With this final rule, we are Three Anaconda Species and One listing four of those species (reticulated Python Species as Injurious Reptiles device for the deaf (TDD), please call the Federal Information Relay Service python, green anaconda, AGENCY: Fish and Wildlife Service, (FIRS) at 800–877–8339. -

RETICULATED PYTHON Malayopython Reticulatus (SCHNEIDER 1801) : RESCUE, RECOVERY and RECENT SIGHTINGS from GREAT NICOBAR ISLAND-A CONSERVATION APPROACH
ECOPRINT 22: 50-55, 2015 ISSN 1024-8668 DOI: http://dx.doi.org/10.3126/eco.v22i0.15470 Ecological Society (ECOS), Nepal www.nepjol.info/index.php/eco; www.ecosnepal.com RETICULATED PYTHON Malayopython reticulatus (SCHNEIDER 1801) : RESCUE, RECOVERY AND RECENT SIGHTINGS FROM GREAT NICOBAR ISLAND-A CONSERVATION APPROACH S. Rajeshkumar 1*, C. Raghunathan 1 and Kailash Chandra 2 1Zoological Survey of India, Andaman and Nicobar Regional Centre Port Blair-744 102, Andaman and Nicobar Islands, India 2Zoological Survey of India, M-Block, New Alipore, Kolkatta-700 053, India *Email: [email protected] ABSTRACT Previously the Reticulated python was recorded by few researchers from Nicobar Islands In 2006, four individuals were observed, but there was no more information added in their literature about sightings in Great Nicobar Island. Pythons were considered as an uncommon and rare encountered species in India also to the Nicobar Islands. Pythons considered relatively rare appearance to have declined due to frequent eradication by habitat destruction On 25 th August 2013, first individual of reticulated python was caught by the local people at Govind Nagar (Lat: 07° 00.074' N, Long: 093° 54.128' E, Altitude at 49.4 meter) in Great Nicobar Island The second one was rescued on 31 st August 2013 in the same area by the local people. Both the recovered individuals were appeared as juvenile. Investigations on population census of this threatened species and their habitat have been felt from the present incidences. Key words : .................................... INTRODUCTION as Malayopython reticulatus (Schneider 1801). Snakes are perhaps one of the most difficult Python is locally (in Nicobarese) called as vertebrate groups to survey (Groombridge and ‘Yammai’ or ‘Tulanth’ (Chandi 2006) and Luxmoore 1991). -

Volume 2. Animals
AC20 Doc. 8.5 Annex (English only/Seulement en anglais/Únicamente en inglés) REVIEW OF SIGNIFICANT TRADE ANALYSIS OF TRADE TRENDS WITH NOTES ON THE CONSERVATION STATUS OF SELECTED SPECIES Volume 2. Animals Prepared for the CITES Animals Committee, CITES Secretariat by the United Nations Environment Programme World Conservation Monitoring Centre JANUARY 2004 AC20 Doc. 8.5 – p. 3 Prepared and produced by: UNEP World Conservation Monitoring Centre, Cambridge, UK UNEP WORLD CONSERVATION MONITORING CENTRE (UNEP-WCMC) www.unep-wcmc.org The UNEP World Conservation Monitoring Centre is the biodiversity assessment and policy implementation arm of the United Nations Environment Programme, the world’s foremost intergovernmental environmental organisation. UNEP-WCMC aims to help decision-makers recognise the value of biodiversity to people everywhere, and to apply this knowledge to all that they do. The Centre’s challenge is to transform complex data into policy-relevant information, to build tools and systems for analysis and integration, and to support the needs of nations and the international community as they engage in joint programmes of action. UNEP-WCMC provides objective, scientifically rigorous products and services that include ecosystem assessments, support for implementation of environmental agreements, regional and global biodiversity information, research on threats and impacts, and development of future scenarios for the living world. Prepared for: The CITES Secretariat, Geneva A contribution to UNEP - The United Nations Environment Programme Printed by: UNEP World Conservation Monitoring Centre 219 Huntingdon Road, Cambridge CB3 0DL, UK © Copyright: UNEP World Conservation Monitoring Centre/CITES Secretariat The contents of this report do not necessarily reflect the views or policies of UNEP or contributory organisations. -

Investigations Into the Presence of Nidoviruses in Pythons Silvia Blahak1, Maria Jenckel2,3, Dirk Höper2, Martin Beer2, Bernd Hoffmann2 and Kore Schlottau2*
Blahak et al. Virology Journal (2020) 17:6 https://doi.org/10.1186/s12985-020-1279-5 RESEARCH Open Access Investigations into the presence of nidoviruses in pythons Silvia Blahak1, Maria Jenckel2,3, Dirk Höper2, Martin Beer2, Bernd Hoffmann2 and Kore Schlottau2* Abstract Background: Pneumonia and stomatitis represent severe and often fatal diseases in different captive snakes. Apart from bacterial infections, paramyxo-, adeno-, reo- and arenaviruses cause these diseases. In 2014, new viruses emerged as the cause of pneumonia in pythons. In a few publications, nidoviruses have been reported in association with pneumonia in ball pythons and a tiger python. The viruses were found using new sequencing methods from the organ tissue of dead animals. Methods: Severe pneumonia and stomatitis resulted in a high mortality rate in a captive breeding collection of green tree pythons. Unbiased deep sequencing lead to the detection of nidoviral sequences. A developed RT-qPCR was used to confirm the metagenome results and to determine the importance of this virus. A total of 1554 different boid snakes, including animals suffering from respiratory diseases as well as healthy controls, were screened for nidoviruses. Furthermore, in addition to two full-length sequences, partial sequences were generated from different snake species. Results: The assembled full-length snake nidovirus genomes share only an overall genome sequence identity of less than 66.9% to other published snake nidoviruses and new partial sequences vary between 99.89 and 79.4%. Highest viral loads were detected in lung samples. The snake nidovirus was not only present in diseased animals, but also in snakes showing no typical clinical signs. -

Aspidites Melanocephalus) in the Wild
Northern Territory Naturalist (2019) 29: 37-39 Short Note An observation of excavating behaviour by a Black-headed Python (Aspidites melanocephalus) in the wild Gerry Swan1 and Christy Harvey2 12 Acron Road, St Ives, NSW 2075, Australia Email: [email protected] 216 Fleetwood Cres, Frankston South, VIC 3199, Australia Abstract The Black-headed Python (Aspidites melanocephalus) and the Woma (Aspidites ramsayi) have both been reported as carrying out burrowing or excavating behaviour. These reports have been based mainly on observations of captive individuals, with the only observations of specimens in the wild being those of Bruton (2013) on Womas. Here we report on a Black-headed Python scooping out sand with its head and fore-body to create a depression in the wild. The pythonid genus Aspidites has been reported as exhibiting burrowing behaviour (Ross & Marzec 1990; Ehmann 1993; Barker & Barker 1994), based mainly on the report by Murphy, Lamoreaux & Barker (1981) that four captive Black-headed Pythons (A. melanocephalus) excavated gravel by using their head and neck to scoop loose material and create a cavity. O’Brien & Naylor (1987) reported that a young specimen that had been recently removed from the wild and was being held pending release, was observed digging beneath rocks and logs, ultimately creating a cavity in which it concealed itself. Fyfe & Harvey (1981) recorded similar behaviour by six captive Womas (Aspidites ramsayi). The floor of the vivaria in which they were housed was covered with 5–15 cm of sand and the pythons scooped this out in large quantities until they reached the base of the vivarium. -

Bearded Dragon Care Notes
CHILDREN’S, STIMSON’S AND SPOTTED PYTHON CARE This group of pythons are non-venomous snakes native to Australia. They belong to the genus Antaresia. There are four known species in this genus including the Children’s python A.childreni, Stimson’s python A.stimsoni, Spotted python A.maculosa & Pygmy python A.perthensis. They are generally relatively easy & low maintenance reptiles to keep in captivity. They are gentle creatures though some individuals may be more temperamental. These pythons rarely grow over 1m in length & may live for over 20 years. Below outlines some ‘basic’ requirements for keeping these pythons as pets. Please note: All Australian snakes are protected species in Australia. Seek individual state & territory requirements for legalities on keeping snakes as pets. Housing .Pythons can be housed indoors. They require suitable artificial heat & light sources as outlined below .Suitable enclosures include ventilated glass/clear plastic fronted wooden or plastic cabinets at least 0.8m long x 0.5m wide x 0.4m high. Juveniles can be kept in smaller plastic tubs – beware their ability to escape! .Furnish the cage with a hide box, branches for climbing & a water bowl heavy/large enough for the snake to bathe in .Substrates (enclosure floor covering) are most simply & hygienically provided by means of newspaper sheets. These pythons may like to ‘burrow’ so using recycled paper ‘cat litter’ pellets is suitable. They can also be housed on Artificial grass .Enclosures should be disinfected at least once weekly (use household bleach diluted 1:10 with water & rinse well afterwards) & ‘spot’ cleaned as necessary .Pythons can be housed individually or in pairs, but beware that fighting may occur. -
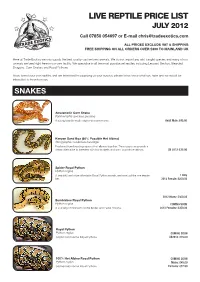
LIVE REPTILE PRICE LIST JULY 2012 Call 07850 054697 Or E-Mail [email protected]
LIVE REPTILE PRICE LIST JULY 2012 Call 07850 054697 or E-mail [email protected] ALL PRICES EXCLUDE VAT & SHIPPING FREE SHIPPING ON ALL ORDERS OVER £300 TO MAINLAND UK Here at Trade Exotics we only supply the best quality captive bred animals. We do not import any wild caught species and many of our animals are bred right here in our own facility. We specialise in all the most popular pet reptiles including Leopard Geckos, Bearded Dragons, Corn Snakes and Royal Pythons. If you breed your own reptiles and are interested in supplying us your surplus, please let us know what you have and we would be interested to hear from you. SNAKES Amelanistic Corn Snake Pantherophis guttatus guttatus A young breeder male surplus to requirements. Adult Male: £45.00 Kenyan Sand Boa (66% Possible Het Albino) Gongylophis colubrinus loveridgei Produced from breeding a pair of het albinos together. These guys can provide a cheap alternative to breeders with low budgets and want to produce albinos. CB 2012: £35.00 Spider Royal Python Python regius A beautiful and more affordable Royal Python morph, we have just the one female 1 Only left. 2012 Female: £200.00 2012 Males: £300.00 Bumblebee Royal Python Python regius COMING SOON A stunning combination of the Spider and Pastel morphs. 2012 Females: £350.00 Royal Python Python regius COMING SOON Captive bred normal Royal Pythons. CB2012: £35.00 100% Het Albino Royal Python COMING SOON Python regius Males: £45.00 Captive bred normal Royal Pythons. Females: £97.50 LEOPARD GECKOS The majority of the Leopard Geckos on our list are bred by ourselves. -

A Rapid Survey of Online Trade in Live Birds and Reptiles in The
S H O R T R E P O R T 0ൾඍඁඈൽඌ A rapid online survey was undertaken EHWZHHQDQG)HEUXDU\ GD\V DSSUR[LPDWHO\KRXUVVXUYH\GD\ RQ pre-selected Facebook groups specializing in the trade of live pets. Ten groups each for reptiles and birds were selected based on trading activities in the previous six months. The survey was carried out during ZHHN GD\V 0RQGD\ WR )ULGD\ E\ JRLQJ through each advertisement posted in A rapid survey of online trade in the groups. Information, including that live birds and reptiles in the Philippines relating to species, quantity, and asking HYDROSAURUS PUSTULATUS WWF / URS WOY WOY WWF / URS PUSTULATUS HYDROSAURUS SULFH ZDV QRWHG 6SHFLHV ZHUH LGHQWL¿HG Report by Cristine P. Canlas, Emerson Y. Sy, to the lowest taxonomic level whenever and Serene Chng possible. Taxonomy follows Gill and 'RQVNHU IRU ELUGV DQG 8HW] et al. IRUUHSWLOHV7KHDXWKRUVFDOFXODWHG ,ඇඍඋඈൽඎർඍංඈඇ WKH WRWDO SRWHQWLDO YDOXH R൵HUHG IRU ELUGV and reptiles based on prices indicated he Philippines is the second largest archipelago in the world by traders. Advertisements that did not comprising 7641 islands and is both a mega-biodiverse specify prices were assigned the lowest country for harbouring wildlife species found nowhere known price for each taxon. Valuations in else in the world, and one of eight biodiversity hotspots this report were based on a conversion rate having a disproportionate number of species threatened with RI86' 3+3 $QRQ ,WLV ,//8675$7,213+,/,33,1(6$,/),1/,=$5' TH[WLQFWLRQIXUWKHULWKDVVRPHRIWKHKLJKHVWUDWHVRIHQGHPLFLW\LQWKH not always possible during online surveys world (Myers et al 7KHLOOHJDOZLOGOLIHWUDGHLVRQHRIWKHPDLQ WRYHULI\WKDWDOOR൵HUVDUHJHQXLQH UHDVRQVEHKLQGVLJQL¿FDQWGHFOLQHVRIVRPHZLOGOLIHSRSXODWLRQVLQ$VLD LQFOXGLQJWKH3KLOLSSLQHV $QRQ6RGKLet al1LMPDQDQG 5ൾඌඎඅඍඌ 6KHSKHUG'LHVPRVet al5DRet al 7KHWildlife Act of 2001 (Republic Act No. -

Biosecurity Risk Assessment
An Invasive Risk Assessment Framework for New Animal and Plant-based Production Industries RIRDC Publication No. 11/141 RIRDCInnovation for rural Australia An Invasive Risk Assessment Framework for New Animal and Plant-based Production Industries by Dr Robert C Keogh February 2012 RIRDC Publication No. 11/141 RIRDC Project No. PRJ-007347 © 2012 Rural Industries Research and Development Corporation. All rights reserved. ISBN 978-1-74254-320-8 ISSN 1440-6845 An Invasive Risk Assessment Framework for New Animal and Plant-based Production Industries Publication No. 11/141 Project No. PRJ-007347 The information contained in this publication is intended for general use to assist public knowledge and discussion and to help improve the development of sustainable regions. You must not rely on any information contained in this publication without taking specialist advice relevant to your particular circumstances. While reasonable care has been taken in preparing this publication to ensure that information is true and correct, the Commonwealth of Australia gives no assurance as to the accuracy of any information in this publication. The Commonwealth of Australia, the Rural Industries Research and Development Corporation (RIRDC), the authors or contributors expressly disclaim, to the maximum extent permitted by law, all responsibility and liability to any person, arising directly or indirectly from any act or omission, or for any consequences of any such act or omission, made in reliance on the contents of this publication, whether or not caused by any negligence on the part of the Commonwealth of Australia, RIRDC, the authors or contributors. The Commonwealth of Australia does not necessarily endorse the views in this publication.