Services That Do Not Require Precertification
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Endoscopic Ultrasound for the Diagnosis of Disease and Staging of Cancers in Adult Patients with Gastroenterological Or Oncological Disease: Guidelines
TITLE: Endoscopic Ultrasound for the Diagnosis of Disease and Staging of Cancers in Adult Patients with Gastroenterological or Oncological Disease: Guidelines DATE: 26 February 2014 RESEARCH QUESTION What are the evidence-based guidelines for the use of endoscopic ultrasound in the diagnosis of disease and staging of cancers in adult patient with gastroenterological or oncological disease? KEY MESSAGE Thirteen evidence-based guidelines regarding the use of endoscopic ultrasound in the diagnosis of disease and staging of cancers in adult patient with gastroenterological or oncological disease were identified. METHODS A limited literature search was conducted on key resources including PubMed, The Cochrane Library (2014, Issue 2), University of York Centre for Reviews and Dissemination (CRD) databases, Canadian and major international health technology agencies, as well as a focused Internet search. Methodological filters were applied to limit retrieval to guidelines. The search was also limited to English language documents published between January 1, 2009 and February 11, 2014. Internet links were provided, where available. The summary of findings was prepared from the abstracts of the relevant information. Please note that data contained in abstracts may not always be an accurate reflection of the data contained within the full article. RESULTS Thirteen evidence-based guidelines regarding the staging and diagnosis of cancer and of gastrointestinal diseases were identified. Additional references of potential interest are provided in the appendix. Disclaimer: The Rapid Response Service is an information service for those involved in planning and providing health care in Canada. Rapid responses are based on a limited literature search and are not comprehensive, systematic reviews. -

Research Article Magnetic Resonance Sialography Findings of Submandibular Ducts Imaging
Hindawi Publishing Corporation BioMed Research International Volume 2013, Article ID 417052, 6 pages http://dx.doi.org/10.1155/2013/417052 Research Article Magnetic Resonance Sialography Findings of Submandibular Ducts Imaging Nezahat Karaca ErdoLan,1 Canan Altay,2 Nesibe Özenler,3 TuLba Bozkurt,1 Engin Uluç,1 Berna Dirim Mete,1 and Esmail Özdemir4 1 Department of Radiology, Izmir Ataturk¨ Research and Training Hospital, Basın Sitesi, Karabaglar,˘ 35360 Izmir, Turkey 2 Department of Radiology, Medical School, Dokuz Eylul University, Inciralti, 35340 Izmir, Turkey 3 Department of Radiology, Balıkesir Ataturk¨ State Hospital, Yıldız Mahallesi Soma Caddesi No. 1, 10100 Balıkesir, Turkey 4 Universal Ege Health Hospital, 35220 Izmir, Turkey Correspondence should be addressed to Canan Altay; [email protected] Received 2 April 2013; Revised 29 May 2013; Accepted 12 June 2013 Academic Editor: Yoshito Tsushima Copyright © 2013 Nezahat Karaca Erdogan˘ et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Purpose. We aimed to assess the problem solving capability of magnetic resonance sialography (MR sialography), a noninvasive method for imaging submandibular gland ducts and determining duct-related pathologies, by comparing diseased and healthy cases. Materials and Methods. We conducted radiological assessment on a total of 60 submandibular glands (mean age 44.7) in 20 cases and 10 volunteers. MR sialography examinations were conducted with single-shot fast spin-echo sequence by using a surface coil placed on the submandibular gland. Each gland was evaluated in terms of the length, width and stricture of the main duct, as well as the difference between the intraparenchymal duct width, and the main duct width. -

Three-Way Comparative Study of Endoscopic Ultrasound-Guided
Surgical Endoscopy (2019) 33:1260–1270 and Other Interventional Techniques https://doi.org/10.1007/s00464-018-6406-7 Three-way comparative study of endoscopic ultrasound-guided transmural gallbladder drainage using lumen-apposing metal stents versus endoscopic transpapillary drainage versus percutaneous cholecystostomy for gallbladder drainage in high-risk surgical patients with acute cholecystitis: clinical outcomes and success in an International, Multicenter Study Ali Siddiqui1 · Rastislav Kunda3 · Amy Tyberg2 · Mustafa A. Arain4 · Arish Noor1 · Tayebah Mumtaz1 · Usama Iqbal1 · David E. Loren1 · Thomas E. Kowalski1 · Douglas G. Adler5 · Monica Saumoy2 · Monica Gaidhane2 · Shawn Mallery4 · Eric M. Christiansen4 · Jose Nieto6 · Michel Kahaleh2 Received: 9 November 2017 / Accepted: 24 August 2018 / Published online: 12 September 2018 © Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract Background Percutaneous cholecystostomy tube (PTGBD), endoscopic retrograde cholangiopancreatography with trans- papillary gallbladder drainage (TP), and endoscopic ultrasound-guided transmural gallbladder drainage (EGBD) using lumen-apposing metal stents (LAMS) have been offered for gallbladder decompression for acute cholecystitis in high-risk surgical patients. Yet, there are limited data comparing these therapies. Our aim was to compare the safety and efficacy of EGBD to TP and PTGBD for gallbladder drainage. Methods We retrospectively collected high-risk surgical patients from six centers with acute cholecystitis who underwent gallbladder drainage by EGBD, TP, or PTGBD. Data included technical success (gallbladder drainage), clinical success (acute cholecystitis resolution), adverse events (AE), and follow-up. Results From 2010 to 2016, 372 patients underwent gallbladder drainage, with 146 by PTGBD, 124 by TP, and 102 drained by EGBD. Technical (98% vs. 88% vs. 94%; p = 0.004) and Clinical (97% vs. -

Impact of Preoperative Endoscopic Ultrasound in Surgical Oncology
REVIEW Impact of preoperative endoscopic ultrasound in surgical oncology Endoscopic ultrasound (EUS) has a strong impact on the imaging and staging of solid tumors within or in close proximity of the upper GI tract. Technological developments during the last two decades have increased the image quality and allowed very detailed visualization of local tumor spread and lymph node affection. Current indications for EUS of the upper GI tract encompass the differentiation between benign and malignant lesions, the staging of esophageal, gastric and pancreatic cancer, and the procurement of a biopsy specimen through fine-needle aspiration. Various technical innovations during the past two decades have increased the diagnostic quality and have simultaneously strengthened the role of EUS in the clinical setting. This article will give a compressed summary on the current state of EUS and possible further technical developments. 1 KEYWORDS: 3D imaging elastosonography endoscopic ultrasound miniprobes Sascha S Chopra & oncologic surgery Michael Hünerbein† 1Department of General & Transplantation Surgery, Charité Campus Virchow-Clinic, Berlin, Conventional endoscopic ultrasound the so-called ‘miniprobes’ into the biliary system Germany Linear versus radial systems or the pancreatic duct in order to obtain high-res- †Author for correspondence: Department of Surgery & Surgical Endoscopic ultrasound (EUS) with flex- olution radial ultrasound images locally. Present Oncology, Helios Hospital Berlin, ible endoscopes is an important diagnostic and mini probes show a diameter of 2–3 mm and oper- 13122 Berlin, Germany Tel.: +49 309 417 1480 therapeutic tool, especially for the local staging ate with frequencies between 12 and 30 MHz. Fax: +49 309 417 1404 of gastrointestinal (GI) cancers, the differen- The main drawbacks of these devices are the lim- michael.huenerbein@ tiation between benign and malignant tumors, ited durability and the decreased depth of penetra- helios-kliniken.de and interventional procedures, such as biopsies tion (~2 cm). -

Cigna Medical Coverage Policies – Radiology Neck Imaging Effective November 15, 2018
Cigna Medical Coverage Policies – Radiology Neck Imaging Effective November 15, 2018 ______________________________________________________________________________________ Instructions for use The following coverage policy applies to health benefit plans administered by Cigna. Coverage policies are intended to provide guidance in interpreting certain standard Cigna benefit plans and are used by medical directors and other health care professionals in making medical necessity and other coverage determinations. Please note the terms of a customer’s particular benefit plan document may differ significantly from the standard benefit plans upon which these coverage policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a coverage policy. In the event of a conflict, a customer’s benefit plan document always supersedes the information in the coverage policy. In the absence of federal or state coverage mandates, benefits are ultimately determined by the terms of the applicable benefit plan document. Coverage determinations in each specific instance require consideration of: 1. The terms of the applicable benefit plan document in effect on the date of service 2. Any applicable laws and regulations 3. Any relevant collateral source materials including coverage policies 4. The specific facts of the particular situation Coverage policies relate exclusively to the administration of health benefit plans. Coverage policies are not recommendations for treatment and should never be used as treatment guidelines. This evidence-based medical coverage policy has been developed by eviCore, Inc. Some information in this coverage policy may not apply to all benefit plans administered by Cigna. These guidelines include procedures eviCore does not review for Cigna. -
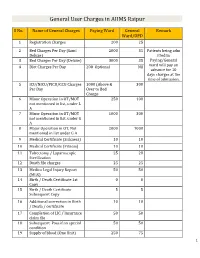
General User Charges in AIIMS Raipur
General User Charges in AIIMS Raipur S No. Name of General Charges Paying Ward General Remark Ward/OPD 1 Registration Charges 200 25 2 Bed Charges Per Day (Sami 2000 35 Patients being adm Deluxe) itted in 3 Bed Charges Per Day (Deluxe) 3000 35 Paying/General 4 Diet Charges Per Day 200 Optional Nil ward will pay an advance for 10 days charges at the time of admission. 5 ICU/NICU/PICU/CCU Charges 1000 (Above & 300 Per Day Over to Bed Charge 6 Minor Operation in OT/MOT 250 100 not mentioned in list, under L A 7 Minor Operation in OT/MOT 1000 300 not mentioned in list, under G A 8 Major Operation in OT, Not 2000 1000 mentioned in list under G A 9 Medical Certificate (Sickness) 10 10 10 Medical Certificate (Fitness) 10 10 11 Tubectomy / Laparoscopic 25 20 Sterilization 12 Death file charges 25 25 13 Medico Legal Injury Report 50 50 (MLR) 14 Birth / Death Certificate 1st 0 0 Copy 15 Birth / Death Certificate 5 5 Subsequent Copy 16 Additional correction in Birth 10 10 / Death / certificate 17 Completion of LIC / Insurance 50 50 claim file 18 Subsequent Pass if on special 50 50 condition 19 Supply of blood (One Unit) 250 75 1 20 Medical Board Certificate 500 500 On Special Case User Charges for Investigations in AIIMS Raipur S No. Name of Investigations Paying General Remark Ward Ward/OPD Anaesthsia 1 ABG 75 50 2 ABG ALONGWITH 150 100 ELECTROLYTES(NA+,K+)(Na,K) 3 ONLY ELECTROLYTES(Na+,K+,Cl,Ca+) 75 50 4 ONLY CALCIUM 50 25 5 GLUCOSE 25 20 6 LACTATE 25 20 7 UREA. -

Endoscopic Ultrasound: What Is It and When Should It Be Used?
CMJ0906-Willert.qxd 11/10/09 7:54 PM Page 539 ■ CLINICAL PRACTICE Clinical Medicine 2009, Vol 9, No 6: 539–43 Endoscopic ultrasound: what is it and when should it be used? Yogananda Reddy and Robert P Willert ABSTRACT – Endoscopic ultrasound (EUS) is an increasingly There are two types of commonly used echoendoscopes each available diagnostic and therapeutic tool used within the UK. with differing characteristics. Radial EUS was the first to be It has wide applications both in the gastrointestinal tract and developed and provides a 360-degree view in a plane perpendic- mediastinum with its current main uses being in the staging ular to that of the scope, similar to a computed tomography (CT) of luminal malignancies and assessment of pancreatic and image (Fig 2). Linear EUS provides a localised oblique image subepithelial lesions. The emergence of linear EUS has parallel to the scope and enables therapeutic intervention under opened up new therapeutic avenues with fine needle aspira- ultrasound (Fig 3). High frequency EUS mini-probes are also tion, trucut biopsies, coeliac plexus blocks and transmural available which can be passed down a standard biopsy channel of pseudocyst drainage all now possible. Future developments an endoscope in cases where strictures cannot be passed using a include localised brachytherapy/chemotherapy and alcohol standard EUS scope. ablation of unresectable pancreatic malignancies and EUS- guided endoscopic surgery. Indications for endoscopic ultrasound KEY WORDS: cancer staging, endoscopic ultrasound, fine The indications for EUS can be divided into several categories: needle aspiration • staging of GI malignancies • evaluating pancreaticobiliary disease Introduction • evaluating subepithelial abnormalities • evaluating extraluminal abnormalities Endoscopic ultrasound (EUS) was developed in the 1980s • staging of lung cancer but was rarely used within most of the UK. -

Procedure Codes for Physician: Radiology
NEW YORK STATE MEDICAID PROGRAM PHYSICIAN - PROCEDURE CODES SECTION 4 - RADIOLOGY Physician – Procedure Codes, Section 4 - Radiology Table of Contents GENERAL INSTRUCTIONS ............................................................................................................ 4 GENERAL RULES AND INFORMATION ......................................................................................... 6 MMIS RADIOLOGY MODIFIERS .................................................................................................... 8 DIAGNOSTIC RADIOLOGY (DIAGNOSTIC IMAGING)................................................................. 9 HEAD AND NECK.................................................................................................................... 9 CHEST .................................................................................................................................. 10 SPINE AND PELVIS .............................................................................................................. 11 UPPER EXTREMITIES .......................................................................................................... 12 LOWER EXTREMITIES ......................................................................................................... 13 ABDOMEN ............................................................................................................................ 14 GASTROINTESTINAL TRACT ............................................................................................... 15 URINARY -

Endoscopic Ultrasound-Guided Placement of the Lumen-Apposing Self-Expandable Metallic Stent for Gallbladder Drainage: a Promising Technique
REVIEW ARTICLE Annals of Gastroenterology (2016) 29, 162-167 Endoscopic ultrasound-guided placement of the lumen-apposing self-expandable metallic stent for gallbladder drainage: a promising technique Rashmee Patila, Mel A. Onab, Charilaos Papafragkakisc, Sury Anandb, Sushil Duddempudib Mount Sinai Health Systems New York, USA; The Brooklyn Hospital Center Academic Affiliate of The Icahn School of Medicine at Mount Sinai Clinical Affiliate of The Mount Sinai Hospital, Brooklyn, New York; MD Anderson Cancer Center Academic and Clinical Affiliate of the University of Texas, Houston, USA Abstract Acute cholecystitis and other clinical problems requiring gallbladder removal or drainage have conventionally been treated with surgery, endoscopic retrograde cholangiopancreatography or percutaneous transhepatic drainage of the gallbladder and/or extrahepatic bile duct. Patients unable to undergo these procedures due to functional status or anatomical anomalies are candidates for endoscopic ultrasound (EUS)-guided gallbladder drainage with stent placement. The aim of this review was to evaluate the technical feasibility and efficacy of EUS-guided placement of the recently developed lumen-apposing self-expandable metallic stent (LASEMS). A literature review was performed to identify the studies describing this technique. In this review article we have summarized case series or reports describing EUS-guided LASEMS placement. The indications, techniques, limitations and complications reported are discussed. A total of 78 patients were included across all studies described thus far in the literature. Studies have reported near 100% technical and clinical success rates in selected cases. No major complications were reported. EUS-guided gallbladder drainage and LASEMS placement can be a safe and effective alternative approach in the management of selected patients. -
MRCP Vs. ERCP
MRCPMRCP vs.vs. ERCPERCP SteveSteve Harrell,Harrell, MD,MD, MSPHMSPH AdvancedAdvanced TherapeuticTherapeutic EndoscopyEndoscopy DecemberDecember 6,6, 20072007 University of Louisville InitialInitial ThoughtsThoughts ““So,So, itit isis mymy predictionprediction thatthat MRCPMRCP willwill havehave aa hugehuge effecteffect onon ERCPERCP practicepractice inin thethe UnitedUnited States.States.”” ““IfIf II hadhad aa pancreaticpancreatic oror biliarybiliary problemproblem II wouldwould searchsearch outout …… aa centercenter withwith thethe mostmost sophisticatedsophisticated noninvasivenoninvasive techniquestechniques…… veryvery quickly.quickly.”” ““WeWe allall wantwant thethe bestbest forfor ourour patients;patients; shouldshould wewe treattreat themthem differentlydifferently thanthan wewe wouldwould ourselves?ourselves?”” 5/15/985/15/98 Peter B. Cotton, MD, FRCP Medical University of South Carolina Charleston, South Carolina Universityhttp://www.ddc.musc.edu/ddc_pro/pro_development of Louisville /hot_topics/impact_MRCP-cotton.htm LearningLearning GoalsGoals KnowKnow whatwhat ERCPERCP andand MRCPMRCP standstand forfor AdvantagesAdvantages andand disadvantagesdisadvantages ofof MRCPMRCP IndicationsIndications forfor ERCPERCP PoorPoor IndicationsIndications forfor ERCPERCP ClinicalClinical UseUse inin commoncommon disordersdisorders forfor MRCPMRCP EffectsEffects ofof MRCPMRCP onon ERCPERCP inin trainingtraining CasesCases University of Louisville ERCPERCP EndoscopicEndoscopic retrograderetrograde cholangiopancreatographycholangiopancreatography -

TAR and Non-Benefit List: Codes 40000 Thru 49999 Page Updated: January 2021
tar and non cd4 1 TAR and Non-Benefit List: Codes 40000 thru 49999 Page updated: January 2021 Surgery Digestive System Note: Refer to the TAR and Non-Benefit: Introduction to List in this manual for more information about the categories of benefit restrictions. Lips Excision Code Description Benefit Restrictions 40490 Biopsy of lip Assistant Surgeon services not payable Other Procedures Code Description Benefit Restrictions 40799 Unlisted procedure, lips Requires TAR, Primary Surgeon/ Provider Vestibule of Mouth Incision Code Description Benefit Restrictions 40800 Drainage of abscess/cyst, mouth, simple Assistant Surgeon services not payable 40801 Drainage of abscess/cyst, mouth, complicated Assistant Surgeon services not payable 40804 Removal of embedded foreign body, mouth, simple Assistant Surgeon services not payable 40805 Removal of embedded foreign body, mouth, Assistant Surgeon complicated services not payable 40806 Incision labial frenum Non-Benefit Excision Code Description Benefit Restrictions 40808 Biopsy, vestibule of mouth Assistant Surgeon services not payable 40810 Excision of lesion mucosa/submucosa, mouth, without Non-Benefit repair Part 2 – TAR and Non-Benefit List: Codes 40000 thru 49999 tar and non cd4 2 Page updated: January 2021 Excision (continued) Code Description Benefit Restrictions 40812 Excision of lesion mucosa/submucosa, mouth, simple Assistant Surgeon repair services not payable 40816 Excision of lesion, mouth, mucosa/submucosa, Assistant Surgeon complex services not payable 40819 Excision of frenum, labial -

Endoscopic Ultrasonography (EUS) [For the List of Services and Procedures That Need Preauthorization, Please Refer To
Clinical Medical Policy Department Clinical Affairs Division Endoscopic Ultrasonography (EUS) [For the list of services and procedures that need preauthorization, please refer to http://www.mcs.com.pr. Go to “Proveedores”, and clic “Políticas Médicas”.] Medical Policy: MP-SU-03-08 Original Effective Date: June 12, 2008 Revised: May 3, 2021 Next Revision: April, 2022 This policy applies to products subscribed by the following corporations, MCS Life Insurance Company (Commercial), and MCS Advantage, Inc. (Classicare) and Medical Card System, Inc., provider’s contract; unless specific contract limitations, exclusions or exceptions apply. Please refer to the member’s benefit certification language for benefit availability. Managed care guidelines related to referral authorization, and precertification of inpatient hospitalization, home health, home infusion and hospice services apply subject to the aforementioned exceptions. DESCRIPTION Endoscopy Ultrasonography (EUS) combines endoscopy and ultrasound in order to obtain images and information about the digestive tract and the surrounding tissue and organ. Endoscopy procedure is the insertion of a long flexible tube via the mouth or the rectum to visualize the digestive tract. Whereas ultrasound uses high frequency sound waves to produce images of the organs and structures inside the body such as ovaries, uterus, liver, gallbladder, pancreas and aorta, etc. Traditional ultrasound sends sound waves to the organ(s) and back with a transducer placed on the skin overlying the organs(s) of interest. Images obtained by traditional ultrasound are not always on high quality. In EUS a small ultrasound transducer is installed on the tip of the endoscope which is inserted into the upper or the lower digestive tract and one can obtain high quality ultrasound images of the organs inside the body (MedicineNet, Inc., 2021).