Procedure Codes for Physician: Radiology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Research Article Magnetic Resonance Sialography Findings of Submandibular Ducts Imaging
Hindawi Publishing Corporation BioMed Research International Volume 2013, Article ID 417052, 6 pages http://dx.doi.org/10.1155/2013/417052 Research Article Magnetic Resonance Sialography Findings of Submandibular Ducts Imaging Nezahat Karaca ErdoLan,1 Canan Altay,2 Nesibe Özenler,3 TuLba Bozkurt,1 Engin Uluç,1 Berna Dirim Mete,1 and Esmail Özdemir4 1 Department of Radiology, Izmir Ataturk¨ Research and Training Hospital, Basın Sitesi, Karabaglar,˘ 35360 Izmir, Turkey 2 Department of Radiology, Medical School, Dokuz Eylul University, Inciralti, 35340 Izmir, Turkey 3 Department of Radiology, Balıkesir Ataturk¨ State Hospital, Yıldız Mahallesi Soma Caddesi No. 1, 10100 Balıkesir, Turkey 4 Universal Ege Health Hospital, 35220 Izmir, Turkey Correspondence should be addressed to Canan Altay; [email protected] Received 2 April 2013; Revised 29 May 2013; Accepted 12 June 2013 Academic Editor: Yoshito Tsushima Copyright © 2013 Nezahat Karaca Erdogan˘ et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Purpose. We aimed to assess the problem solving capability of magnetic resonance sialography (MR sialography), a noninvasive method for imaging submandibular gland ducts and determining duct-related pathologies, by comparing diseased and healthy cases. Materials and Methods. We conducted radiological assessment on a total of 60 submandibular glands (mean age 44.7) in 20 cases and 10 volunteers. MR sialography examinations were conducted with single-shot fast spin-echo sequence by using a surface coil placed on the submandibular gland. Each gland was evaluated in terms of the length, width and stricture of the main duct, as well as the difference between the intraparenchymal duct width, and the main duct width. -

Original Article the Imaging Characteristics of Magnetic Resonance Hysterosalpingography in Infertile Women
Int J Clin Exp Med 2020;13(6):3955-3962 www.ijcem.com /ISSN:1940-5901/IJCEM0107779 Original Article The imaging characteristics of magnetic resonance hysterosalpingography in infertile women Jiugen Ruan1, Chunyan Wu2, Changhua Zhu1, Yao Ding1, Qiuping Tan1, Tao Meng3 Departments of 1Radiology, 2Gynaecology, The People’s Hospital of Xinyu City, Xinyu, Jiangxi, China; 3RIMAG Medical Imaging Corporation, Shanghai, China Received January 13, 2020; Accepted April 1, 2020; Epub June 15, 2020; Published June 30, 2020 Abstract: Objective: We aimed to analyze the imaging characteristics of magnetic resonance hysterosalpingography (MR-HSG) in infertile women. Methods: A total of 20 infertile women admitted to our hospital from October 2018 to December 2019 were selected as the subjects of study for retrospective analysis. The MR-HSG examination was performed in all patients to analyze the examination results and imaging characteristics. Results: (1) The comple- tion rate of MR-HSG examination was 100.00% in the 20 patients, of which those with primary infertility accounted for 65.00% and those with secondary infertility accounted for 35.00%. (2) Among the 20 infertile patients, 30.00% had unobstructed fallopian tubes, 40.00% had partial fallopian tube obstruction, 20.00% had full fallopian tube obstruction and 10.00% had hydrosalpinx. (3) Among the 14 patients with abnormal fallopian tubes, 14.29% had bilateral fallopian tube obstruction, 35.71% had partial fallopian tube obstruction on both sides, 7.14% had fallo- pian tubes that were unobstructed on one side and obstructed on the other side, 21.43% had fallopian tubes that were unobstructed on one side and partially obstructed on the other side, 7.14% had fallopian tubes partially ob- structed on one side and obstructed on the other side, and 14.29% had hydrosalpinx. -

Hysterosalpingography
H y s t e r o s alp i n g o g r aph y A b o u t P r e p a r a t i o n s Hysterosalpingography is an x-ray examination of the The hysterosalpingography procedure is best uterus and fallopian tubes that uses a special form of x- performed one week after menstruation but before ray called fluoroscopy and a contrast material. During a ovulation to make certain that you are not pregnant hysterosalpingogram, the uterus and fallopian tubes are during the exam. This procedure should not be filled with a contrast material and the radiologist is able to performed if you have an active inflammatory condition. use fluoroscopy to view and assess their anatomy and You should notify your radiologist if you have a chronic function. pelvic infection or an untreated sexually transmitted disease at the time of the procedure. Hysterosalpingography is primarily used to examine women who have difficulty becoming pregnant by On the night before the procedure, you may be asked allowing the radiologist to evaluate the shape and to take a laxative or an enema to empty your bowels, so structure of the uterus, the openness of the fallopian the uterus and surrounding structures can be seen tubes, and any scarring within the uterine or abdominal clearly. Prior to the procedure, you may be given a mild cavity. sedative or over-the-counter medication to minimize any potential discomfort. The exam is used to investigate repeated miscarriages that result from abnormalities in the uterus and to You should inform your radiologist of any medications determine the presence and severity of the following you are taking and if you have any allergies, especially abnormalities: to barium or iodinated contrast materials. -
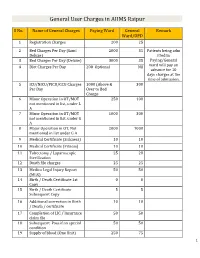
General User Charges in AIIMS Raipur
General User Charges in AIIMS Raipur S No. Name of General Charges Paying Ward General Remark Ward/OPD 1 Registration Charges 200 25 2 Bed Charges Per Day (Sami 2000 35 Patients being adm Deluxe) itted in 3 Bed Charges Per Day (Deluxe) 3000 35 Paying/General 4 Diet Charges Per Day 200 Optional Nil ward will pay an advance for 10 days charges at the time of admission. 5 ICU/NICU/PICU/CCU Charges 1000 (Above & 300 Per Day Over to Bed Charge 6 Minor Operation in OT/MOT 250 100 not mentioned in list, under L A 7 Minor Operation in OT/MOT 1000 300 not mentioned in list, under G A 8 Major Operation in OT, Not 2000 1000 mentioned in list under G A 9 Medical Certificate (Sickness) 10 10 10 Medical Certificate (Fitness) 10 10 11 Tubectomy / Laparoscopic 25 20 Sterilization 12 Death file charges 25 25 13 Medico Legal Injury Report 50 50 (MLR) 14 Birth / Death Certificate 1st 0 0 Copy 15 Birth / Death Certificate 5 5 Subsequent Copy 16 Additional correction in Birth 10 10 / Death / certificate 17 Completion of LIC / Insurance 50 50 claim file 18 Subsequent Pass if on special 50 50 condition 19 Supply of blood (One Unit) 250 75 1 20 Medical Board Certificate 500 500 On Special Case User Charges for Investigations in AIIMS Raipur S No. Name of Investigations Paying General Remark Ward Ward/OPD Anaesthsia 1 ABG 75 50 2 ABG ALONGWITH 150 100 ELECTROLYTES(NA+,K+)(Na,K) 3 ONLY ELECTROLYTES(Na+,K+,Cl,Ca+) 75 50 4 ONLY CALCIUM 50 25 5 GLUCOSE 25 20 6 LACTATE 25 20 7 UREA. -

Evidence Tables
Evidence Tables Citation: Bipat S, van Leeuwen MS, Comans EF, Pijl ME, Bossuyt PM, Zwinderman AH, Stoker J. Colorectal liver metastases: CT, MR imaging, and PET for diagnosis. Meta-analysis (DARE structured abstract). Radiology 2005; 237:123-131 Design: systematic review and meta-analysis (search ended Jan 2004) Country: the Netherlands Aim: to perform a meta-analysis to obtain sensitivity estimates of CT, MRI, and, FDG-PET for detection of colorectal liver metastases on per-patient and per-lesion basis. Inclusion criteria • Articles reported in English, French or German languages • CT, MRI, or FDG-PET were used to identify and characterise colorectal liver metastases • Histopathological analysis (performed at surgery, biopsy, and autopsy), intra-operative observation (manual palpation or intra-operative ultrasound), and/or follow up were used as the reference standard • Sufficient data was present to calculate the true positive and false negative valuses for imaging techniques • When data or subsets of data were presented in more than one article, the article with the most details or the most recent article was selected. Exclusion criteria • If results of different imaging modalities were presented in combination and could not be differentiated for performance assessment of an individual modality. • Review articles, letters, comments, articles that did not include raw data were not selected. Population 61 articles fulfilled the inclusion criteria, 3187 patients in total. Patients with colorectal cancer Age range 12-93, age mean 61 In -

Zwanger-Pesiri Radiology Provides the Latest Ability to Detect, Characterize, Stage Ultrasound (Sonography) Equipment at Each of and Treat Disease Our Offices
ESIRI P At the Forefront of Forefront the At WANGER- Z Technology, Diagnosis & Care Technology, 521 Route 111 Stony Brook Medical Park Hauppauge 11788 2500 Nesconset Hwy, Bldg 15 Stony Brook 11790 80 Maple Avenue 25A Smithtown 11787 220 Belle Mead Rd 763 Larkfield Road R Commack 11725 347 East Setauket 11733 - E 25A W - 680 Old Country Rd i 25A l l i 2087 Deer Park Ave a Plainview 11803 25 m Deer Park 11729 N G i F c 112 l 1500 William Floyd Pkwy - 111 o o y l l d s Shirley 11967 272 North Broadway kwy P P 25 R 495 k N Hicksville 11801 the t e d w r rn - No Sta 231 y S 495 a g 111 454 27 A t i 495 k o 1390 Hempstead Tpke Suffolk Ave - s Brookhaven Prof. Park 11003 Wantagh Pkwy P Elmont y M k w 135 106 w k ead North Ocean Plaza 285 Sills Road, Bldg 15 o kwy y P Hempstead Tpke P W w 107 te ta b S 1729 N. Ocean Ave Patchogue 11772 d n - r r n e o a South 443 Sunrise Hwy l 24 o 27 Medford 11763 s k I Z zprad.com Lynbrook 11563 s P s k 27A o r w lt Pkwy C y Be S nrise u Hwy 759 Montauk Hwy 160 Brentwood Rd 2012 Sunrise Hwy West Islip 11795 Bay Shore 11706 516 631 Merrick 11566 126 Hicksville Rd Massapequa 11758 150 E. Sunrise Hwy Lindenhurst 11757 CVS Plaza 355 Broadway Amityville 11701 C ontinuum of C are Echocardiography Two-dimensional imaging of the cardiovascular system Confidence Accurate assessment of the velocity Unsurpassed diagnostic technology of blood, cardiac tissue and cardiac valves The most experience with 3.0 Tesla MRI and 3D Mammography on Long Island Visualizes leaking of blood through the valves (valvular regurgitation) -

ACR–ACOG–AIUM–SRU PRACTICE PARAMETER for the PERFORMANCE of SONOHYSTEROGRAPHY and HYSTEROSALPINGO- CONTRAST-SONOGRAPHY (Hycosy)
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2020 (Resolution 4) * ACR–ACOG–AIUM–SRU PRACTICE PARAMETER FOR THE PERFORMANCE OF SONOHYSTEROGRAPHY AND HYSTEROSALPINGO- CONTRAST-SONOGRAPHY (HyCoSy) PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -

Ultrasonography in Hepatobiliary Diseases
Ultrasonography in Hepatobiliary diseases Pages with reference to book, From 189 To 194 Kunio Okuda ( Department of Medicine, Chiba University School of Medicine, Chiba, Japan (280). ) Introduction of real-time linear scan ultrasonography to clinical practice has revolutionalized the diagnostic approach to hepatobiiary disorders. 1 This modality allows the operator to scan the liver and biliary tract with a real-time effect, and obtain three dimensional images. One can follow vessels and ducts from one end to the other. The portal and hepatic venous systems are readily seen and distinguished. Real-time ultrasonography (US) using an electronically activated linear array transducer is becoming a stethoscope for the liver specialist, because a portable size real-time ültrasonograph is already available. It is now established that real-time US is useful not only in the diagnosis of gallstones, dilatation of the biliary tract, and cystic lesions, but it can also assess liver parenchyma in various diffuse liver diseases. Thus, a wide range of diffuse liver diseases beside localized hepatic lesions can he evaluated by US. It can also make the diagnosis of portal hypertension 2-4 In our unit, the patient with a suspected hepatobiiary disorder is examined by US on the first day of hospital visit, and the next investigation that will pOssibly provide a definitive diagnosis, such as ERCP, PTC, X-ray CT, angiography, scintigraphy, etc., is scheduled. Using a specially designed transducer, a needle can be guided while the vessel, a duct, or a structure is being aimed and entered (US-guided puncture). 5 ;7 US-guided puncture technique has improved the procedure for percutaneous transhepatic cholangiogrpahy 8, biliary decompression, percutaneous transhepatic catheterizatiøn for portography 9, and obliteration of bleeding varices. -

Non-Contrast MR Portography Using Time-Spatial Labeling Inversion
Mubarak et al. Egyptian Journal of Radiology and Nuclear Medicine (2019) 50:40 Egyptian Journal of Radiology https://doi.org/10.1186/s43055-019-0036-5 and Nuclear Medicine RESEARCH Open Access Non-contrast MR portography using time-spatial labeling inversion pulse for diagnosis of portal vein pathology Amr Ahmed Mubarak, Ghada Elsaed Awad, Mohamed Adel Eltomey* and Mahmoud Abd Elaziz Dawoud Abstract Background: To study the ability of non-contrast MR portography using time-spatial labeling inversion pulse (T-SLIP) as a non-invasive contrast-free imaging modality to delineate different portal vein pathological conditions. The study included 25 patients with known history of portal vein disease and another 25 age-matched patients with normal portal vein. Both groups were examined by respiratory-triggered non-contrast MR portography using time-spatial labeling inversion pulse technique. Image quality was assessed first, and findings of diagnostic scans were compared to color duplex ultrasonography and selectively in those with diseased portal vein to portal-phase images of dynamic contrast-enhanced MRI. Results: Significant relation was found between breathing regularity and image quality in T-SLIP sequence, with diagnostic scans sensitivity and specificity of 89.29% and 86.21%, respectively, for diagnosis of different portal vein pathological conditions. Conclusions: Non-contrast MR portography is a useful technique for diagnosis of portal vein pathology in carefully selected patients. Keywords: Portal vein, Portography, Non-contrast, Time-spatial, T-SLIP, Magnetic resonance Background nephrogenic systemic fibrosis with gadolinium chelates Accurate radiological assessment of portal vein is crucial used in contrast-enhanced MRI [3, 4]. Moreover, the ac- to rule out portal vein disease, to detect anatomical vari- curate timing of contrast bolus together with competent ations, and to draw a road map for surgeons planning long breath holds are mandatory to obtain good quality for hepatectomy or liver transplant [1]. -

Kidney Ureter Bladder Diagnostic Technique
KUB Kidney Ureter Bladder Diagnostic Technique . Plain KUB . Intravenous urography : IVP . Voiding cystourethrography : VCUG . Hysterosalpingography . Ultrasonography Plain KUB . The projection includes the entire urinary system . From the superior aspects of the kidneys . To the pubic symphysis . Not include the diaphragm Indication Plain films are widely used in the management of stone diseases What are you looking for? . Calcifications . Abnormal soft tissue . Air within urinary tract . Bony abnormalities Transverse Process Urinary Tract Stone . Most common cause of acute ureteral obstruction . Clinical presentation : 1. Flank pain 2. Intermittent hematuria Clinical Perspective Acute flank pain, with dramatic relief upon passage of the stone 1. UPJ stone : flank pain 2. Proximal ureteric stone : flank pain radiating to the genitals 3. UVJ stone : voiding urgency and suprapubic discomfort, and they cause pain that radiates into the groin and genitals Hematuria Radiologic Evaluation of Hematuria . The AUA guidelines recommended upper tract imaging for low- and high-risk patients with microscopic hematuria . Gross hematuria -> much higher risk of malignancy than microscopic disease Hematuria : Cause . Calculi . Infection . Cancer . Obstruction . Anticoagulation . Artifactual cause: menstrual blood, food such as beets, berries, rhubarb Radiologic Work-up of Hematuria . No universal agreement about the optimal imaging work-up of hematuria . Traditionally : IVP was the standard . Recently : . Multidetector CT scans have become routine . MRI can be used to detect urinary tract abnormalities, but has limited use because of its expense and the lack of data supporting its use ACR Appropriateness Criteria Scale for Hematuria ACR Appropriateness Criteria Scale for Hematuria ACR Appropriateness Criteria Scale for Hematuria Urinary tract stone . Increasing overall prevalence in the last decade . -

Magnetic Resonance Hysterosalpingography in Diagnostic Work-Up of Female Infertility – Comparison with Conventional Hysterosalpingography: a Randomised Study
European Radiology (2019) 29:501–508 https://doi.org/10.1007/s00330-018-5572-2 UROGENITAL Magnetic resonance hysterosalpingography in diagnostic work-up of female infertility – comparison with conventional hysterosalpingography: a randomised study Manuelle Volondat1 & Eric Fontas2 & Jerome Delotte3 & Imene Fatfouta3 & Patrick Chevallier1 & Madleen Chassang1 Received: 17 January 2018 /Revised: 17 May 2018 /Accepted: 28 May 2018 /Published online: 4 July 2018 # European Society of Radiology 2018 Abstract Objective To compare diagnostic accuracy of MR-hysterosalpingography (MR-HSG) and conventional hysterosalpingography (X-HSG) in the evaluation of female infertility. Methods Forty women received prospectively both X-HSG, the gold standard technique, and MR-HSG on the same day but the order in which they were conducted was randomised. A 1.5 Tesla MRI was performed with classical sequences for pelvic analysis and an additional 3D T1-weighted sequence with intra-uterine injection of gadolinium. Two radiologists independently interpreted X-HSG and MR-HSG according to randomisation, blinded to the other results. They both then performed a second interpretation of MR-HSG blinded to the first reading with a minimum time delay of 1 week. Diagnostic performance of MR-HSG for analysis of tubal and intracavity abnormalities was evaluated by calculating sensitivity (Se), specificity (Sp), positive predictive value (PPV) and negative predictive value (NPV). Results Twenty-six patients were included. Diagnostic performance of MR-HSG was: Se: 91.7% (95% CI 61.5–99.8); Sp: 92.9% (95% CI 66.1–99.8) ; PPV: 91.7% (95% CI 61.5–99.8); NPV: 92.9% (95% CI 66.1–99.8). -

Cholescintigraphy Stellingen
M CHOLESCINTIGRAPHY STELLINGEN - • - . • • ' - • i Cholescintigrafie is een non-invasief en betrouwbaar onderzoek in de diagnostiek bij icterische patienten_doch dient desalniettemin als een complementaire en niet als compfititieye studie beschouwd te worden. ]i i Bij de abceptatie voor levensverzekeringen van patienten met ! hypertensie wordt onvoldoende rekening gehouden met de reactie jj op de ingestelde behandeling. ! Ill | Ieder statisch scintigram is een functioneel beeld. | 1 IV ] The purpose of a liver biopsy is not to obtain the maximum \ possible quantity of liver tissue, but to obtain a sufficient 3 quantity with the minimum risk to the patient. j V ( Menghini, 1970 ) I1 Bij post-traumatische verbreding van het mediastinum superius is I angiografisdi onderzoek geindiceerd. VI De diagnostische waarde van een radiologisch of nucleair genees- kundig onderzoek wordt niet alleen bepaald door de kwaliteit van de apparatuur doch voonnamelijk door de deskundigheid van de onderzoeker. VII Ultra sound is whistling in the dark. VIII De opname van arts-assistenten, in opleiding tot specialist, in de C.A.O. van het ziekenhuiswezen is een ramp voor de opleiding. IX De gebruikelijke techniek bij een zogenaamde "highly selective vagotomy" offert meer vagustakken op dan noodzakelijk voor reductie van de zuursecretie. X Het effect van "enhancing" sera op transplantaat overleving is groter wanneer deze sera tijn opgewekt onder azathioprine. XI Gezien de contaminatiegraad van in Nederland verkrijgbare groenten is het gebraik als rauwkost ten stelligste af te raden. j Het het ontstaan van een tweede maligniteit als complicatie van 4 cytostatische therapie bij patienten met non-Hodgkin lymphoma, | maligne granuloom en epitheliale maligne aandoeningen dient, j vooral bij langere overlevingsduur, rekening gehouden te worden.