The Digestive System Functions of the Digestive System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Baseline Structure of the Enteric Nervous System and Its Role in Parkinson’S Disease
life Review The Baseline Structure of the Enteric Nervous System and Its Role in Parkinson’s Disease Gianfranco Natale 1,2,* , Larisa Ryskalin 1 , Gabriele Morucci 1 , Gloria Lazzeri 1, Alessandro Frati 3,4 and Francesco Fornai 1,4 1 Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, 56126 Pisa, Italy; [email protected] (L.R.); [email protected] (G.M.); [email protected] (G.L.); [email protected] (F.F.) 2 Museum of Human Anatomy “Filippo Civinini”, University of Pisa, 56126 Pisa, Italy 3 Neurosurgery Division, Human Neurosciences Department, Sapienza University of Rome, 00135 Rome, Italy; [email protected] 4 Istituto di Ricovero e Cura a Carattere Scientifico (I.R.C.C.S.) Neuromed, 86077 Pozzilli, Italy * Correspondence: [email protected] Abstract: The gastrointestinal (GI) tract is provided with a peculiar nervous network, known as the enteric nervous system (ENS), which is dedicated to the fine control of digestive functions. This forms a complex network, which includes several types of neurons, as well as glial cells. Despite extensive studies, a comprehensive classification of these neurons is still lacking. The complexity of ENS is magnified by a multiple control of the central nervous system, and bidirectional communication between various central nervous areas and the gut occurs. This lends substance to the complexity of the microbiota–gut–brain axis, which represents the network governing homeostasis through nervous, endocrine, immune, and metabolic pathways. The present manuscript is dedicated to Citation: Natale, G.; Ryskalin, L.; identifying various neuronal cytotypes belonging to ENS in baseline conditions. -

Relationships Between the Autonomic Nervous System and the Pancreas Including Regulation of Regeneration and Apoptosis Recent Developments
ORIGINAL ARTICLE Relationships Between the Autonomic Nervous System and the Pancreas Including Regulation of Regeneration and Apoptosis Recent Developments Takayoshi Kiba, MD, PhD organ at birth, reaches its adult size and morphology after Abstract: Substantial new information has accumulated on the weaning (3 weeks of age). mechanisms of secretion, the development, and regulation of the gene In pancreatic regeneration after cholecystokinin analog expression, and the role of growth factors in the differentiation, growth, and regeneration of the pancreas. Many genes that are re- cerulein-induced acute pancreatitis, 2 separate peaks of DNA quired for pancreas formation are active after birth and participate in synthesis have been reported. The first peak corresponded with endocrine and exocrine cell functions. Although the factors that nor- duct cell and mesenchymal cell proliferation, and the second mally regulate the proliferation of the pancreas largely remain elu- peak was associated with acinar cell proliferation.1 However, sive, several factors to influence the growth have been identified. It in this model, islet cells did not regenerate. Formation of new was also reported that the pancreas was sensitive to a number of apop-  cells can take place via 2 pathways: replication of already totic stimuli. The autonomic nervous system influences many of the differentiated  cells and neogenesis from putative islet stem functions of the body, including the pancreas. In fact, the parasympa- cells. It is generally admitted that neogenesis mostly takes thetic nervous system and the sympathetic nervous system have op- place during fetal and neonatal life. In adulthood, little increase posing effects on insulin secretion from islet  cells; feeding-induced in the -cell number seems to occur. -

Mouth Esophagus Stomach Rectum and Anus Large Intestine Small
1 Liver The liver produces bile, which aids in digestion of fats through a dissolving process known as emulsification. In this process, bile secreted into the small intestine 4 combines with large drops of liquid fat to form Healthy tiny molecular-sized spheres. Within these spheres (micelles), pancreatic enzymes can break down fat (triglycerides) into free fatty acids. Pancreas Digestion The pancreas not only regulates blood glucose 2 levels through production of insulin, but it also manufactures enzymes necessary to break complex The digestive system consists of a long tube (alimen- 5 carbohydrates down into simple sugars (sucrases), tary canal) that varies in shape and purpose as it winds proteins into individual amino acids (proteases), and its way through the body from the mouth to the anus fats into free fatty acids (lipase). These enzymes are (see diagram). The size and shape of the digestive tract secreted into the small intestine. varies in each individual (e.g., age, size, gender, and disease state). The upper part of the GI tract includes the mouth, throat (pharynx), esophagus, and stomach. The lower Gallbladder part includes the small intestine, large intestine, The gallbladder stores bile produced in the liver appendix, and rectum. While not part of the alimentary 6 and releases it into the duodenum in varying canal, the liver, pancreas, and gallbladder are all organs concentrations. that are vital to healthy digestion. 3 Small Intestine Mouth Within the small intestine, millions of tiny finger-like When food enters the mouth, chewing breaks it 4 protrusions called villi, which are covered in hair-like down and mixes it with saliva, thus beginning the first 5 protrusions called microvilli, aid in absorption of of many steps in the digestive process. -

Physiology of the Pancreas
LECTURE IV: Physiology of the Pancreas EDITING FILE IMPORTANT MALE SLIDES EXTRA FEMALE SLIDES LECTURER’S NOTES 1 PHYSIOLOGY OF THE PANCREAS Lecture Four OBJECTIVES ● Functional Anatomy ● Major components of pancreatic juice and their physiologic roles ● Cellular mechanisms of bicarbonate secretion ● Cellular mechanisms of enzyme secretion ● Activation of pancreatic enzymes ● Hormonal & neural regulation of pancreatic secretion ● Potentiation of the secretory response Pancreas Lying parallel to and beneath the stomach, it is a large compound gland with most of its internal structure similar to that of the salivary glands. It is composed of: Figure 4-1 Endocrine portion 1-2% Exocrine portion 95% (Made of Islets of Langerhans) (Acinar gland tissues) Secrete hormones into the blood Made of acinar & ductal cells.1 - ● Insulin (beta cells; 60%) secretes digestive enzymes, HCO3 ● Glucagon (alpha cells; 25%) and water into the duodenum . ● Somatostatin (delta cells; 10%). Figure 4-2 Figure 4-3 ● The pancreatic digestive enzymes are secreted by pancreatic acini. ● Large volumes of sodium bicarbonate solution are secreted by the small ductules and larger ducts leading from the acini. ● Pancreatic juice is secreted in response to the presence of chyme in the upper portions of the small intestine. ● Insulin and Glucagon are crucial for normal regulation of glucose, lipid, and protein metabolism. FOOTNOTES 1. Acinar cells arrange themselves like clusters of grapes, that eventually release their secretions into ducts. Collection of acinar cells is called acinus, acinus and duct constitute one exocrine gland. 2 PHYSIOLOGY OF THE PANCREAS Lecture Four Pancreatic Secretion: ● Amount ≈ 1.5 L/day in an adult human. ● The major functions of pancreatic secretion: To neutralize the acids in the duodenal chyme to optimum range 1 (pH=7.0-8.0) for activity of pancreatic enzymes. -

Gastrointestinal Motility Physiology
GASTROINTESTINAL MOTILITY PHYSIOLOGY JAYA PUNATI, MD DIRECTOR, PEDIATRIC GASTROINTESTINAL, NEUROMUSCULAR AND MOTILITY DISORDERS PROGRAM DIVISION OF PEDIATRIC GASTROENTEROLOGY AND NUTRITION, CHILDREN’S HOSPITAL LOS ANGELES VRINDA BHARDWAJ, MD DIVISION OF PEDIATRIC GASTROENTEROLOGY AND NUTRITION CHILDREN’S HOSPITAL LOS ANGELES EDITED BY: CHRISTINE WAASDORP HURTADO, MD REVIEWED BY: JOSEPH CROFFIE, MD, MPH NASPGHAN PHYSIOLOGY EDUCATION SERIES SERIES EDITORS: CHRISTINE WAASDORP HURTADO, MD, MSCS, FAAP [email protected] DANIEL KAMIN, MD [email protected] CASE STUDY 1 • 14 year old female • With no significant past medical history • Presents with persistent vomiting and 20 lbs weight loss x 3 months • Initially emesis was intermittent, occurred before bedtime or soon there after, 2-3 hrs after a meal • Now occurring immediately or up to 30 minutes after a meal • Emesis consists of undigested food and is nonbloody and nonbilious • Associated with heartburn and chest discomfort 3 CASE STUDY 1 • Initial screening blood work was unremarkable • A trial of acid blockade was started with improvement in heartburn only • Antiemetic therapy with ondansetron showed no improvement • Upper endoscopy on acid blockade was normal 4 CASE STUDY 1 Differential for functional/motility disorders: • Esophageal disorders: – Achalasia – Gastroesophageal Reflux – Other esophageal dysmotility disorders • Gastric disorders: – Gastroparesis – Rumination syndrome – Gastric outlet obstruction : pyloric stricture, pyloric stenosis • -

Enteric Nervous System (ENS): 1) Myenteric (Auerbach) Plexus & 2
Enteric Nervous System (ENS): 1) Myenteric (Auerbach) plexus & 2) Submucosal (Meissner’s) plexus à both triggered by sensory neurons with chemo- and mechanoreceptors in the mucosal epithelium; effector motors neurons of the myenteric plexus control contraction/motility of the GI tract, and effector motor neurons of the submucosal plexus control secretion of GI mucosa & organs. Although ENS neurons can function independently, they are subject to regulation by ANS. Autonomic Nervous System (ANS): 1) parasympathetic (rest & digest) – can innervate the GI tract and form connections with ENS neurons that promote motility and secretion, enhancing/speeding up the process of digestion 2) sympathetic (fight or flight) – can innervate the GI tract and inhibit motility & secretion by inhibiting neurons of the ENS Sections and dimensions of the GI tract (alimentary canal): Esophagus à ~ 10 inches Stomach à ~ 12 inches and holds ~ 1-2 L (full) up to ~ 3-4 L (distended) Duodenum à first 10 inches of the small intestine Jejunum à next 3 feet of small intestine (when smooth muscle tone is lost upon death, extends to 8 feet) Ileum à final 6 feet of small intestine (when smooth muscle tone is lost upon death, extends to 12 feet) Large intestine à 5 feet General Histology of the GI Tract: 4 layers – Mucosa, Submucosa, Muscularis Externa, and Serosa Mucosa à epithelium, lamina propria (areolar connective tissue), & muscularis mucosae Submucosa à areolar connective tissue Muscularis externa à skeletal muscle (in select parts of the tract); smooth muscle (at least 2 layers – inner layer of circular muscle and outer layer of longitudinal muscle; stomach has a third layer of oblique muscle under the circular layer) Serosa à superficial layer made of areolar connective tissue and simple squamous epithelium (a.k.a. -

Motility in the Large Intestine Physiology > Digestive > Digestive
Motility in the Large Intestine Physiology > Digestive > Digestive HAUSTRAL CONTRACTIONS (Definition): Slow, segmenting movements that further mix chyme. • About every 30 minutes. • Occur in haustra: small pouches caused by the teniae coli (longitudinal smooth muscle ribbons that run along outside the entire length of the colon). Because they are shorter than the large intestine, the large intestine tucks between the teniae and form sacs • Primarily occur in ascending and transverse colons. • Produced by contractions of smooth muscle layer Steps 1. Chyme fills a haustrum 2. Distension in the haustrum. 3. Smooth muscle layer contracts 4. Contractions move chyme into the next haustrum and subsequent haustra, where the sequence begins again. #Note that haustral contractions play a relatively minor role in propelling fecal waste through the large intestine; their main function to further mix waste. Contractions also bring chyme in close contact with the large intestine mucosal layer to maximize water and electrolyte absorption • Hasutral contractions also occur in the descending and sigmoid colon to further concentrate stored fecal waste prior to elimination. MASS MOVEMENTS (Definition): slow, but powerful contractions of the large intestine that move undigested waste to the rectum for defecation via the anus. • Much like stronger and sustained peristaltic contractions. • 3-4 times a day. • Mainly in the transverse, descending, and sigmoid colons. • Produced by circular layer (smooth muscle) contractions Steps 1. Undigested waste in the transverse colon. 2. Triggered by the gastrocolic reflex (initiated following ingestion of a meal when food enters the stomach causes its distension) 3. Circular layer contracts in the transverse colon 4. Contractions move waste towards the rectum. -
Digestive System
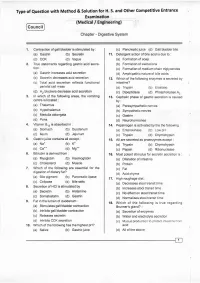
Type of Question with Method & Solution for H. S. and Other Competitive Entrance Examination (Medical / Engineering) Cou ncil Chapter - Digestive System '1. Contraction of gall bladder is stimulated by : (c) Pancreatic,uice (d) Gall bladder bile (a) Gastrin (b) Secretin 1r. Detergent action of bile acid is due to : (c) CCK (d) Vagus (a) Formation of soap 2. True statemenls regarding gastric acid secre- (b) Formation of zwitterions . tion: (c) Formation of medium chain triglycerides (a) Gastrin increases acid secretion (d) Amphipathic nature of bile acids (b) Secretin decreases acid secretion 12. Which of the following enzymes is secreted by (c) Total acid secretion reflects functional intestine? parietal cell mass (a) Trypsin (b) Elaslase (d). H2 blockers decrease acid secretion . (c) Dipeptidase (d) Phospholipase 42 3. ln which of the following areas, the vomiting 13. Cephalic phase of gastric secretion is caused centre is located : by: (a) Thalamus . (a) Parasympathetic nerves (b) Hypothalamus (b) Sympathetic nerves (c) Medulla oblongata (c) Gastrin (d) Pons (d) Neurohormones in : 4, Vitamin 8,, is absorbed '14. Pepsinogen is activated by lhe the following : (a) Stomach (b) Duodenum (a) Enterokinase (b) Low pH (c) lleum (d) Jejunum (c) Trypsin (d) Chymotrypsin 5. Gastricjuice contains all except : 15. All are secreted as proenzymes except : (a) Na" (b) K- (a) Trypsin (b) Chymotrypsin (c) Ca". (d) Ms.* (c) Pepsin (d) Ribonuclease Bilirubin is derived from : 6. 16. Most potent stimulus for secretin secretion is : . (a) Myoglobin (b) Haemoglobin (a) Dilatation of intestine (c) Cholesterol (d) Muscle (b) Protein 7. Which of the following are essential for the (c) Fat digestion of dietary fat? (d) Acid chyme (a) Bile plgment (b) Pancreatlc lipase 17. -

Digestive System Physiology of the Pancreas
Digestive System Physiology of the pancreas Dr. Hana Alzamil Objectives Pancreatic acini Pancreatic secretion Pancreatic enzymes Control of pancreatic secretion ◦ Neural ◦ Hormonal Secretin Cholecystokinin What are the types of glands? Anatomy of pancreas Objectives Pancreatic acini Pancreatic secretion Pancreatic enzymes Control of pancreatic secretion ◦ Neural ◦ Hormonal Secretin Cholecystokinin Histology of the Pancreas Acini ◦ Exocrine ◦ 99% of gland Islets of Langerhans ◦ Endocrine ◦ 1% of gland Secretory function of pancreas Acinar and ductal cells in the exocrine pancreas form a close functional unit. Pancreatic acini secrete the pancreatic digestive enzymes. The ductal cells secrete large volumes of sodium bicarbonate solution The combined product of enzymes and sodium bicarbonate solution then flows through a long pancreatic duct Pancreatic duct joins the common hepatic duct to form hepatopancreatic ampulla The ampulla empties its content through papilla of vater which is surrounded by sphincter of oddi Objectives Pancreatic acini Pancreatic secretion Pancreatic enzymes Control of pancreatic secretion ◦ Neural ◦ Hormonal Secretin Cholecystokinin Composition of Pancreatic Juice Contains ◦ Water ◦ Sodium bicarbonate ◦ Digestive enzymes Pancreatic amylase pancreatic lipase Pancreatic nucleases Pancreatic proteases Functions of pancreatic secretion Fluid (pH from 7.6 to 9.0) ◦ acts as a vehicle to carry inactive proteolytic enzymes to the duodenal lumen ◦ Neutralizes acidic gastric secretion Enzymes ◦ -

Human Body- Digestive System
Previous reading: Human Body Digestive System (Organs, Location and Function) Science, Class-7th, Rishi Valley School Next reading: Cardiovascular system Content Slide #s 1) Overview of human digestive system................................... 3-4 2) Organs of human digestive system....................................... 5-7 3) Mouth, Pharynx and Esophagus.......................................... 10-14 4) Movement of food ................................................................ 15-17 5) The Stomach.......................................................................... 19-21 6) The Small Intestine ............................................................... 22-23 7) The Large Intestine ............................................................... 24-25 8) The Gut Flora ........................................................................ 27 9) Summary of Digestive System............................................... 28 10) Common Digestive Disorders ............................................... 31-34 How to go about this module 1) Have your note book with you. You will be required to guess or answer many questions. Explain your guess with reasoning. You are required to show the work when you return to RV. 2) Move sequentially from 1st slide to last slide. Do it at your pace. 3) Many slides would ask you to sketch the figures. – Draw them neatly in a fresh, unruled page. – Put the title of the page as the slide title. – Read the entire slide and try to understand. – Copy the green shade portions in the note book. 4) -

Behaviour of Digestive Enzymes in the Pancreatic Juice and Pancreas of Rats Fed on a Low-Protein Diet (3 P
Behaviour of digestive enzymes in the pancreatic juice and pancreas of rats fed on a low-protein diet (3 p. 100 of cereal protein) then on a balanced diet (23.5 p. 100 of mixed protein) O. Kheroua, J. Belleville To cite this version: O. Kheroua, J. Belleville. Behaviour of digestive enzymes in the pancreatic juice and pancreas of rats fed on a low-protein diet (3 p. 100 of cereal protein) then on a balanced diet (23.5 p. 100 of mixed protein). Reproduction Nutrition Développement, 1981, 21 (6A), pp.901-917. hal-00897907 HAL Id: hal-00897907 https://hal.archives-ouvertes.fr/hal-00897907 Submitted on 1 Jan 1981 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Behaviour of digestive enzymes in the pancreatic juice and pancreas of rats fed on a low-protein diet (3 p. 100 of cereal protein) then on a balanced diet (23.5 p. 100 of mixed protein) O. KHEROUA, J. BELLEVILLE Laboratoire de Physiologie de la Nutrition Université d’Oran, Algérie. * Laboratoire de Physiologie de la Nutrition UER Nutrition, BP 138, 21100 Dijon Cedex, France. Summary. The aim of this study in the rat was to determine the effect of a low-protein diet (3 p. -

Effect of Acid Infusion Into Various Levels of the Intestine on Gastric and Pancreatic Secretion in the Cat
Gut: first published as 10.1136/gut.10.9.749 on 1 September 1969. Downloaded from Gut, 1969, 10, 749-753 Effect of acid infusion into various levels of the intestine on gastric and pancreatic secretion in the cat S. J. KONTUREK, J. DUBIEL, AND B. GABRY9 From the Department ofMedicine, Medical School, Krakow, Poland SUMMARY Intraduodenal infusion of increasing amounts of hydrochloric acid solution results in a stepwise increase in the volume of pancreatic secretion and output of bicarbonate, reaching about 90 % of amounts attained with exogenous secretin infused intravenously in increasing doses. Acid infusion into the different regions of the intestine stimulates pancreatic secretion only from the duodenum and upper jejunum, suggesting that the area ofendogenous release of secretin by acid is confined to the upper part ofthe small bowel in the cat. Gastric acid secretion induced by pentagastrin, but not by histamine, is inhibited by acid perfusion of the duodenum. The acidification of other parts of the small intestine does not result in any change in gastric acid secretion induced either by pentagastrin or by histamine. Previous studies have shown that acidification of the ligament of Treitz, and the third in the ileum about 25 cm duodenum in the cat inhibits gastric acid secretion proximal to the caecum. and stimulates pancreatic secretion, due to the endogenous release of secretin (Konturek, Dubiel, SECRETORY PROCEDURE The secretory tests were started and and about two weeks after the cats hadrecoveredfrom surgery. Gabryg, 1969; Konturek, Gabrys, Dubiel, http://gut.bmj.com/ 1969). No study, however, has compared the relative effects on gastric and pancreatic secretion of acid infusions into various regions of the small intestine.