Enteric Nervous System (ENS): 1) Myenteric (Auerbach) Plexus & 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Baseline Structure of the Enteric Nervous System and Its Role in Parkinson’S Disease
life Review The Baseline Structure of the Enteric Nervous System and Its Role in Parkinson’s Disease Gianfranco Natale 1,2,* , Larisa Ryskalin 1 , Gabriele Morucci 1 , Gloria Lazzeri 1, Alessandro Frati 3,4 and Francesco Fornai 1,4 1 Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, 56126 Pisa, Italy; [email protected] (L.R.); [email protected] (G.M.); [email protected] (G.L.); [email protected] (F.F.) 2 Museum of Human Anatomy “Filippo Civinini”, University of Pisa, 56126 Pisa, Italy 3 Neurosurgery Division, Human Neurosciences Department, Sapienza University of Rome, 00135 Rome, Italy; [email protected] 4 Istituto di Ricovero e Cura a Carattere Scientifico (I.R.C.C.S.) Neuromed, 86077 Pozzilli, Italy * Correspondence: [email protected] Abstract: The gastrointestinal (GI) tract is provided with a peculiar nervous network, known as the enteric nervous system (ENS), which is dedicated to the fine control of digestive functions. This forms a complex network, which includes several types of neurons, as well as glial cells. Despite extensive studies, a comprehensive classification of these neurons is still lacking. The complexity of ENS is magnified by a multiple control of the central nervous system, and bidirectional communication between various central nervous areas and the gut occurs. This lends substance to the complexity of the microbiota–gut–brain axis, which represents the network governing homeostasis through nervous, endocrine, immune, and metabolic pathways. The present manuscript is dedicated to Citation: Natale, G.; Ryskalin, L.; identifying various neuronal cytotypes belonging to ENS in baseline conditions. -

Relationships Between the Autonomic Nervous System and the Pancreas Including Regulation of Regeneration and Apoptosis Recent Developments
ORIGINAL ARTICLE Relationships Between the Autonomic Nervous System and the Pancreas Including Regulation of Regeneration and Apoptosis Recent Developments Takayoshi Kiba, MD, PhD organ at birth, reaches its adult size and morphology after Abstract: Substantial new information has accumulated on the weaning (3 weeks of age). mechanisms of secretion, the development, and regulation of the gene In pancreatic regeneration after cholecystokinin analog expression, and the role of growth factors in the differentiation, growth, and regeneration of the pancreas. Many genes that are re- cerulein-induced acute pancreatitis, 2 separate peaks of DNA quired for pancreas formation are active after birth and participate in synthesis have been reported. The first peak corresponded with endocrine and exocrine cell functions. Although the factors that nor- duct cell and mesenchymal cell proliferation, and the second mally regulate the proliferation of the pancreas largely remain elu- peak was associated with acinar cell proliferation.1 However, sive, several factors to influence the growth have been identified. It in this model, islet cells did not regenerate. Formation of new was also reported that the pancreas was sensitive to a number of apop-  cells can take place via 2 pathways: replication of already totic stimuli. The autonomic nervous system influences many of the differentiated  cells and neogenesis from putative islet stem functions of the body, including the pancreas. In fact, the parasympa- cells. It is generally admitted that neogenesis mostly takes thetic nervous system and the sympathetic nervous system have op- place during fetal and neonatal life. In adulthood, little increase posing effects on insulin secretion from islet  cells; feeding-induced in the -cell number seems to occur. -

Secretin-Induced Gastric Relaxation Is Mediated by Vasoactive Intestinal Polypeptide and Prostaglandin Pathways
Neurogastroenterol Motil (2009) 21, 754–e47 doi: 10.1111/j.1365-2982.2009.01271.x Secretin-induced gastric relaxation is mediated by vasoactive intestinal polypeptide and prostaglandin pathways Y. LU & C. OWYANG Division of Gastroenterology, Department of Internal Medicine, University of Michigan, Ann Arbor, MI, USA Abstract Secretin has been shown to delay gastric vagally mediated pathway. Through nicotinic emptying and inhibit gastric motility. We have dem- synapses, secretin stimulates VIP release from post- onstrated that secretin acts on the afferent vagal ganglionic neurons in the gastric myenteric plexus, pathway to induce gastric relaxation in the rat. How- which in turn induces gastric relaxation through a ever, the efferent pathway that mediates the action of prostaglandin-dependent pathway. secretin on gastric motility remains unknown. We Keywords gastric relaxation, indomethacin, vagus recorded the response of intragastric pressure to graded nerve. doses of secretin administered intravenously to anaesthetized rats using a balloon attached to a cath- eter and placed in the body of the stomach. Secretin INTRODUCTION evoked a dose-dependent decrease in intragastric Secretin has been shown to inhibit gastric contrac- pressure. The threshold dose of secretin was 1.4 pmol tions and delay gastric emptying of liquids and kg)1 h)1 and the effective dose, 50% was 5.6 pmol kg)1 solids.1–3 However, the mechanisms of secretinÕs h)1. Pretreatment with hexamethonium markedly inhibitory effects on gastric motility remain unclear. reduced gastric relaxation induced by secretin The gene expression of secretin receptor has been (5.6 pmol kg)1 h)1). Bilateral vagotomy also signifi- demonstrated in the rat nodose ganglia.4 We have cantly reduced gastric motor responses to secretin. -

Physiology of the Pancreas
LECTURE IV: Physiology of the Pancreas EDITING FILE IMPORTANT MALE SLIDES EXTRA FEMALE SLIDES LECTURER’S NOTES 1 PHYSIOLOGY OF THE PANCREAS Lecture Four OBJECTIVES ● Functional Anatomy ● Major components of pancreatic juice and their physiologic roles ● Cellular mechanisms of bicarbonate secretion ● Cellular mechanisms of enzyme secretion ● Activation of pancreatic enzymes ● Hormonal & neural regulation of pancreatic secretion ● Potentiation of the secretory response Pancreas Lying parallel to and beneath the stomach, it is a large compound gland with most of its internal structure similar to that of the salivary glands. It is composed of: Figure 4-1 Endocrine portion 1-2% Exocrine portion 95% (Made of Islets of Langerhans) (Acinar gland tissues) Secrete hormones into the blood Made of acinar & ductal cells.1 - ● Insulin (beta cells; 60%) secretes digestive enzymes, HCO3 ● Glucagon (alpha cells; 25%) and water into the duodenum . ● Somatostatin (delta cells; 10%). Figure 4-2 Figure 4-3 ● The pancreatic digestive enzymes are secreted by pancreatic acini. ● Large volumes of sodium bicarbonate solution are secreted by the small ductules and larger ducts leading from the acini. ● Pancreatic juice is secreted in response to the presence of chyme in the upper portions of the small intestine. ● Insulin and Glucagon are crucial for normal regulation of glucose, lipid, and protein metabolism. FOOTNOTES 1. Acinar cells arrange themselves like clusters of grapes, that eventually release their secretions into ducts. Collection of acinar cells is called acinus, acinus and duct constitute one exocrine gland. 2 PHYSIOLOGY OF THE PANCREAS Lecture Four Pancreatic Secretion: ● Amount ≈ 1.5 L/day in an adult human. ● The major functions of pancreatic secretion: To neutralize the acids in the duodenal chyme to optimum range 1 (pH=7.0-8.0) for activity of pancreatic enzymes. -

Cells Using Gene Expression Profiling and Insulin Gene Methylation
RESEARCH ARTICLE Comparison of enteroendocrine cells and pancreatic β-cells using gene expression profiling and insulin gene methylation ☯ ☯ Gyeong Ryul Ryu , Esder Lee , Jong Jin Kim, Sung-Dae MoonID, Seung-Hyun Ko, Yu- Bae Ahn, Ki-Ho SongID* Division of Endocrinology & Metabolism, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea ☯ These authors contributed equally to this work. a1111111111 * [email protected] a1111111111 a1111111111 a1111111111 a1111111111 Abstract Various subtypes of enteroendocrine cells (EECs) are present in the gut epithelium. EECs and pancreatic β-cells share similar pathways of differentiation during embryonic develop- ment and after birth. In this study, similarities between EECs and β-cells were evaluated in OPEN ACCESS detail. To obtain specific subtypes of EECs, cell sorting by flow cytometry was conducted Citation: Ryu GR, Lee E, Kim JJ, Moon S-D, Ko S- from STC-1 cells (a heterogenous EEC line), and each single cell was cultured and pas- H, Ahn Y-B, et al. (2018) Comparison of saged. Five EEC subtypes were established according to hormone expression, measured enteroendocrine cells and pancreatic β-cells using by quantitative RT-PCR and immunostaining: L, K, I, G and S cells expressing glucagon-like gene expression profiling and insulin gene methylation. PLoS ONE 13(10): e0206401. https:// peptide-1, glucose-dependent insulinotropic polypeptide, cholecystokinin, gastrin and doi.org/10.1371/journal.pone.0206401 secretin, respectively. Each EEC subtype was found to express not only the corresponding Editor: Wataru Nishimura, International University gut hormone but also other gut hormones. Global microarray gene expression profiles of Health and Welfare School of Medicine, JAPAN revealed a higher similarity between each EEC subtype and MIN6 cells (a β-cell line) than Received: March 29, 2018 between C2C12 cells (a myoblast cell line) and MIN6 cells, and all EEC subtypes were highly similar to each other. -

Download PDF Enteric Nervous System Development in Cavitary
Romanian Journal of Morphology and Embryology 2008, 49(1):63–67 ORIGINAL PAPER Enteric nervous system development in cavitary viscera allocated to the celiac plexus ALINA MARIA ŞIŞU1), CODRUŢA ILEANA PETRESCU1), C. C. CEBZAN1), M. C. NICULESCU1), V. NICULESCU1), P. L. MATUSZ1), M. C. RUSU2) 1)Department of Anatomy and Embryology, “Victor Babeş” University of Medicine and Pharmacy, Timisoara 2)Department of Anatomy and Embryology, Faculty of Dental Medicine, “Carol Davila” University of Medicine and Pharmacy, Bucharest Abstract Enteric nervous system (ENS) is a network made of neuronal cells and nervous fibers. There are two plexuses: myenteric of Auerbach and sub mucous of Meissner and Henle. Many substances are involved in neurotransmission at ENS level. ENS assures all gastrointestinal system functions: digestion, absorption, etc. Our study is made on 23 human fetal specimens at different ages of evolution with crown-rump lengths from 9 to 28 cm, and three new born human specimens. We used the Trichrome Masson stain technique and the argental impregnation Bielschowsky on block technique for microscopic evidence. Our study concerned the cavitary viscera allocated to the celiac plexus, involving all layers of each studied viscera. Keywords: viscera, neurons, celiac plexus, argental impregnation. Introduction Auerbach myenteric plexus, with location between the longitudinal and circular muscular layers and sub The enteric nervous system (ENS) is from mucous plexus (Meissner and Henle) between the morphological and neurochemistry point of view a real circular muscle and mucous muscle layer. “brain”. At a complex network level made from neurons The ultra structural studies show that the ENS and nervous fibers we find much more structure is closer to the central nervous system than the neurotransmitters and neuromodulaters than anywhere sympathetic and parasympathetic ganglia [5–7]. -

S41467-019-14258-Z.Pdf
ARTICLE https://doi.org/10.1038/s41467-019-14258-z OPEN Erythroid differentiation regulator-1 induced by microbiota in early life drives intestinal stem cell proliferation and regeneration Hirohito Abo1, Benoit Chassaing 1,2,3,4, Akihito Harusato 1, Miguel Quiros5, Jennifer C. Brazil5, Vu L. Ngo1, Emilie Viennois6, Didier Merlin6,7, Andrew T. Gewirtz1, Asma Nusrat5 & Timothy L. Denning1* 1234567890():,; Gut microbiota and their metabolites are instrumental in regulating intestinal homeostasis. However, early-life microbiota associated influences on intestinal development remain incompletely understood. Here we demonstrate that co-housing of germ-free (GF) mice with specific-pathogen free (SPF) mice at weaning (exGF) results in altered intestinal gene expression. Our results reveal that one highly differentially expressed gene, erythroid dif- ferentiation regulator-1 (Erdr1), is induced during development in SPF but not GF or exGF mice and localizes to Lgr5+ stem cells and transit amplifying (TA) cells. Erdr1 functions to induce Wnt signaling in epithelial cells, increase Lgr5+ stem cell expansion, and promote intestinal organoid growth. Additionally, Erdr1 accelerates scratch-wound closure in vitro, increases Lgr5+ intestinal stem cell regeneration following radiation-induced injury in vivo, and enhances recovery from dextran sodium sulfate (DSS)-induced colonic damage. Col- lectively, our findings indicate that early-life microbiota controls Erdr1-mediated intestinal epithelial proliferation and regeneration in response to mucosal damage. 1 Center for Inflammation, Immunity & Infection, Institute for Biomedical Sciences, Georgia State University, 100 Piedmont Ave, Atlanta, GA 30303, USA. 2 Neuroscience Institute and Institute for Biomedical Sciences, Georgia State University, Atlanta, Georgia, USA. 3 INSERM, U1016, Paris, France. 4 Université de Paris, Paris, France. -
Neural and Neuroendocrine Control of Digestion: Regulation of Gastrointestinal Hormone Secretion
Neural and Neuroendocrine Control of Digestion: Regulation of Gastrointestinal Hormone Secretion (Chapter 15 in “Eckert Animal Physiology) (Chapter 4 in Hill, Wise & Anderson: “Animal Physiology”) (Chapter 10 in Hadley: “Endocrinology”) General Concepts Covered: — neural and neuroendocrine integration of a complex physiological process — co-ordination of endocrine and exocrine secretion — exocrine secretion affecting endocrine status — endocrine influences on neural, muscle and secretory functions — paracrine and autocrine effects — local influences — positive and negative “feed-back” actions — enzymatic cascades — integration of carbohydrate, fat and protein digestion and appetite control General Introduction — digestion requires co-ordination of movement of food particles, mechanical and chemical digestion of food — opening and closing of sphincter muscles to contain food particles in certain gut compartments for appropriate processing, also control passage through compartments — proper sequential enzymatic processing General Introduction (cont.) — peristaltic action to move food through gut — kneading movement to mix food particles with enzymes and to expose new surfaces for digestion, as well as for absorption From Eckert Secretin - first proposed hormone — 1902, WM Baylist and EH Starling (observations in dogs) — addition of food or acid in stomach is usually followed by pancreatic enzyme secretion into intestine — dennervate and tie off duodenum from stomach, then 1) add acid to stomach - no pancreatic enzyme secretion 2) add acid to -
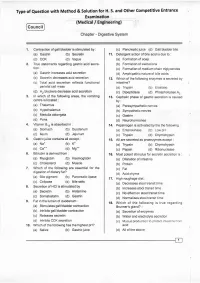
Digestive System
Type of Question with Method & Solution for H. S. and Other Competitive Entrance Examination (Medical / Engineering) Cou ncil Chapter - Digestive System '1. Contraction of gall bladder is stimulated by : (c) Pancreatic,uice (d) Gall bladder bile (a) Gastrin (b) Secretin 1r. Detergent action of bile acid is due to : (c) CCK (d) Vagus (a) Formation of soap 2. True statemenls regarding gastric acid secre- (b) Formation of zwitterions . tion: (c) Formation of medium chain triglycerides (a) Gastrin increases acid secretion (d) Amphipathic nature of bile acids (b) Secretin decreases acid secretion 12. Which of the following enzymes is secreted by (c) Total acid secretion reflects functional intestine? parietal cell mass (a) Trypsin (b) Elaslase (d). H2 blockers decrease acid secretion . (c) Dipeptidase (d) Phospholipase 42 3. ln which of the following areas, the vomiting 13. Cephalic phase of gastric secretion is caused centre is located : by: (a) Thalamus . (a) Parasympathetic nerves (b) Hypothalamus (b) Sympathetic nerves (c) Medulla oblongata (c) Gastrin (d) Pons (d) Neurohormones in : 4, Vitamin 8,, is absorbed '14. Pepsinogen is activated by lhe the following : (a) Stomach (b) Duodenum (a) Enterokinase (b) Low pH (c) lleum (d) Jejunum (c) Trypsin (d) Chymotrypsin 5. Gastricjuice contains all except : 15. All are secreted as proenzymes except : (a) Na" (b) K- (a) Trypsin (b) Chymotrypsin (c) Ca". (d) Ms.* (c) Pepsin (d) Ribonuclease Bilirubin is derived from : 6. 16. Most potent stimulus for secretin secretion is : . (a) Myoglobin (b) Haemoglobin (a) Dilatation of intestine (c) Cholesterol (d) Muscle (b) Protein 7. Which of the following are essential for the (c) Fat digestion of dietary fat? (d) Acid chyme (a) Bile plgment (b) Pancreatlc lipase 17. -

1 the Anatomy and Physiology of the Oesophagus
111 2 3 1 4 5 6 The Anatomy and Physiology of 7 8 the Oesophagus 9 1011 Peter J. Lamb and S. Michael Griffin 1 2 3 4 5 6 7 8 911 2011 location deep within the thorax and abdomen, 1 Aims a close anatomical relationship to major struc- 2 tures throughout its course and a marginal 3 ● To develop an understanding of the blood supply, the surgical exposure, resection 4 surgical anatomy of the oesophagus. and reconstruction of the oesophagus are 5 ● To establish the normal physiology and complex. Despite advances in perioperative 6 control of swallowing. care, oesophagectomy is still associated with the 7 highest mortality of any routinely performed ● To determine the structure and function 8 elective surgical procedure [1]. of the antireflux barrier. 9 In order to understand the pathophysiol- 3011 ● To evaluate the effect of surgery on the ogy of oesophageal disease and the rationale 1 function of the oesophagus. for its medical and surgical management a 2 basic knowledge of oesophageal anatomy and 3 physiology is essential. The embryological 4 Introduction development of the oesophagus, its anatomical 5 structure and relationships, the physiology of 6 The oesophagus is a muscular tube connecting its major functions and the effect that surgery 7 the pharynx to the stomach and measuring has on them will all be considered in this 8 25–30 cm in the adult. Its primary function is as chapter. 9 a conduit for the passage of swallowed food and 4011 fluid, which it propels by antegrade peristaltic 1 contraction. It also serves to prevent the reflux Embryology 2 of gastric contents whilst allowing regurgita- 3 tion, vomiting and belching to take place. -

Pancreatic Amylase
1. Functional Anatomy • The pancreas which lies parallel to and beneath the stomach is composed of: 1. The endocrine islets of Langerhans which secrete: Hormone Type of cell % of secretion Insulin Beta cells 60% crucial for normal regulation of glucose, Glucagon Alpha cells ~25% lipid & protein metabolism Somatostatin delta cells ~10% 1. Acinar gland tissues which produce pancreatic juice (the main source of digestive enzymes). • The pancreatic digestive enzymes are secreted by pancreatic acini. • Large volumes of sodium Bicarbonate solution are secreted by the small ductules and larger ducts leading from the acini. • Pancreatic juice is secreted in Response to the presence of Chyme in the upper portions of the small intestine. 2. Major Components of Pancreatic Secretion and Their Physiologic Roles & 5. Activation of Pancreatic Enzymes • The major functions of pancreatic secretion: 1. To neutralize the acids in the duodenal chyme to optimum range (pH= 7.0-8.0) for activity of pancreatic enzymes. 2. To prevent damage to duodenal mucosa by acid & pepsin. 3. To produce enzymes involved in the digestion of dietary carbohydrate, fat, and protein. Pancreatic Enzymes: The pancreas secrests enzymes that act on all major types of food stuffs. 1. Pancreatic Proteolytic Enzymes (Trypsin, Chymotrypsin, Carboxypolypeptidase, Elastase) • Trypsin & Chymotrypsin split whole and partially digested proteins into peptides of various sizes but do not cause release of individual amino acids. • Carboxypolypeptidase splits some peptides into individual amino acids, thus completing digestion of some proteins to amino acids. • When first synthesized in the pancreatic cells, digestive enzymes are in the inactive forms; these enzymes become activated only after they are secreted into the intestinal tract. -

Secretin Stimulates the Secretion of Bile from the Liver. It Also Increases Watery Bicarbonate Solution from Pancreatic Duct Epithelium
Name Secretin acetate Cat # PP-1670 Size 1 g, 10 g, 100, g and bulk custom packages CAS# 17034-35-4 Mol. Mass 3055.47 Formula C130H220N44O41 Sequence H-His-Ser-Asp-Gly-Thr-Phe-Thr-Ser-Glu-Leu-Ser-Arg-Leu-Arg-Asp-Ser- Ala-Arg-Leu-Gln-Arg-Leu-Leu-Gln-Gly-Leu-Val-NH2 Purity >95% Secretin is a peptide hormone produced in the S cells of the duodenum in the crypts of Lieberkühn. Its primary effect is to regulate the pH of the duodenal contents via the control of gastric acid secretion and buffering with bicarbonate. Secretin stimulates the secretion of bile from the liver. It also increases watery bicarbonate solution from pancreatic duct epithelium. Pancreatic acinar cells have secretin receptors in their plasma membrane. As secretin binds to these receptors, it stimulates adenylate cyclase activity and converts ATP to cyclic AMP.[12] Cyclic AMP acts as second messenger in intracellular signal transduction and leads to increase in release of watery carbonate.It is known to promote the normal growth and maintenance of the pancreas. Secretin increases water and bicarbonate secretion from duodenal Brunner's glands in order to buffer the incoming protons of the acidic chyme.[13] It also enhances the effects of cholecystokinin to induce the secretion of digestive enzymes and bile from pancreas and gallbladder, respectively. It counteracts blood glucose concentration spikes by triggering increased insulin release from pancreas, following oral glucose intake.<[14] It also reduces acid secretion from the stomach by inhibiting gastrin release from G cells.[citation needed] This helps neutralize the pH of the digestive products entering the duodenum from the stomach, as digestive enzymes from the pancreas (eg, pancreatic amylase and pancreatic lipase) function optimally at neutral pH.[citation needed] In addition, secretin simulates pepsin secretion which can help break down proteins in food digestion.