Gastrointestinal Motility Physiology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glossary - Cellbiology
1 Glossary - Cellbiology Blotting: (Blot Analysis) Widely used biochemical technique for detecting the presence of specific macromolecules (proteins, mRNAs, or DNA sequences) in a mixture. A sample first is separated on an agarose or polyacrylamide gel usually under denaturing conditions; the separated components are transferred (blotting) to a nitrocellulose sheet, which is exposed to a radiolabeled molecule that specifically binds to the macromolecule of interest, and then subjected to autoradiography. Northern B.: mRNAs are detected with a complementary DNA; Southern B.: DNA restriction fragments are detected with complementary nucleotide sequences; Western B.: Proteins are detected by specific antibodies. Cell: The fundamental unit of living organisms. Cells are bounded by a lipid-containing plasma membrane, containing the central nucleus, and the cytoplasm. Cells are generally capable of independent reproduction. More complex cells like Eukaryotes have various compartments (organelles) where special tasks essential for the survival of the cell take place. Cytoplasm: Viscous contents of a cell that are contained within the plasma membrane but, in eukaryotic cells, outside the nucleus. The part of the cytoplasm not contained in any organelle is called the Cytosol. Cytoskeleton: (Gk. ) Three dimensional network of fibrous elements, allowing precisely regulated movements of cell parts, transport organelles, and help to maintain a cell’s shape. • Actin filament: (Microfilaments) Ubiquitous eukaryotic cytoskeletal proteins (one end is attached to the cell-cortex) of two “twisted“ actin monomers; are important in the structural support and movement of cells. Each actin filament (F-actin) consists of two strands of globular subunits (G-Actin) wrapped around each other to form a polarized unit (high ionic cytoplasm lead to the formation of AF, whereas low ion-concentration disassembles AF). -
General Principles of GIT Physiology Objectives
General Principles of GIT Physiology Objectives: ❖ Physiologic Anatomy of the Gastrointestinal Wall. ❖ The General & Specific Characteristics of Smooth Muscle. ❖ Neural & Hormonal Control of Gastrointestinal Function. ❖ Types of Neurotransmitters Secreted by Enteric Neurons. ❖ Functional Types of Movements in the GIT. ❖ Gastrointestinal Blood Flow "Splanchnic Circulation". ❖ Effect of Gut Activity and Metabolic Factors on GI Blood Flow. Done by : ➔ Team leader: Rahaf AlShammari ➔ Team members: ◆ Renad AlMigren, Rinad Alghoraiby ◆ Yazeed AlKhayyal, Hesham AlShaya Colour index: ◆ Turki AlShammari, Abdullah AlZaid ● Important ◆ Dana AlKadi, Alanoud AlEssa ● Numbers ◆ Saif AlMeshari, Ahad AlGrain ● Extra َ Abduljabbar AlYamani ◆ َوأن َّل ْي َ َس ِلْ ِْلن َسا ِنَ ِإََّلَ َما َس َع ىَ Gastrointestinal System: GIT Gastrointestinal System Associated Organs (Liver,gallbladder,pancreas,salivary gland) Gastrointestinal Function: ● The alimentary tract provides the body with a continual supply of water, electrolytes, and nutrients. To achieve this function, it requires: 1 Movement of food through the alimentary tract (motility). 2 Secretion of digestive juices and digestion of the food. 3 Absorption of water, various electrolytes, and digestive products. 4 Circulation of blood through the gastrointestinal organs to carry away the absorbed substances. ● Control of all these functions is by local, nervous, and hormonal systems. The Four Processes Carried Out by the GIT: 2 Physiologic Anatomy of the Gastrointestinal Wall ● The following layers structure the GI wall from inner surface outward: ○ The mucosa ○ The submucosa ○ Circular muscle layer ○ longitudinal muscle layer Same layers in Same layers Histology lecture Histology ○ The serosa. ● In addition, sparse bundles of smooth muscle fibers, the mucosal muscle, lie in the deeper layers of the mucosa. The General Characteristics of Smooth Muscle 1- Two Smooth Muscle Classification: Unitary type ● Contracts spontaneously in response to stretch, in the Rich in gap junctions absence of neural or hormonal influence. -

The Baseline Structure of the Enteric Nervous System and Its Role in Parkinson’S Disease
life Review The Baseline Structure of the Enteric Nervous System and Its Role in Parkinson’s Disease Gianfranco Natale 1,2,* , Larisa Ryskalin 1 , Gabriele Morucci 1 , Gloria Lazzeri 1, Alessandro Frati 3,4 and Francesco Fornai 1,4 1 Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, 56126 Pisa, Italy; [email protected] (L.R.); [email protected] (G.M.); [email protected] (G.L.); [email protected] (F.F.) 2 Museum of Human Anatomy “Filippo Civinini”, University of Pisa, 56126 Pisa, Italy 3 Neurosurgery Division, Human Neurosciences Department, Sapienza University of Rome, 00135 Rome, Italy; [email protected] 4 Istituto di Ricovero e Cura a Carattere Scientifico (I.R.C.C.S.) Neuromed, 86077 Pozzilli, Italy * Correspondence: [email protected] Abstract: The gastrointestinal (GI) tract is provided with a peculiar nervous network, known as the enteric nervous system (ENS), which is dedicated to the fine control of digestive functions. This forms a complex network, which includes several types of neurons, as well as glial cells. Despite extensive studies, a comprehensive classification of these neurons is still lacking. The complexity of ENS is magnified by a multiple control of the central nervous system, and bidirectional communication between various central nervous areas and the gut occurs. This lends substance to the complexity of the microbiota–gut–brain axis, which represents the network governing homeostasis through nervous, endocrine, immune, and metabolic pathways. The present manuscript is dedicated to Citation: Natale, G.; Ryskalin, L.; identifying various neuronal cytotypes belonging to ENS in baseline conditions. -

Autonomic Dysfunction in Cystic Fibrosis
JOURNAL OF THE ROYAL SOCIETY OF MEDICINE Supplement No. 43 Volume 96 2003 Autonomic dysfunction in cystic fibrosis AMirakhur MB MRCP MJWalshaw MD FRCP J R Soc Med 2003;96(Suppl. 43):11–17 SECTION OF PAEDIATRICS & CHILD HEALTH, 26 NOVEMBER 2002 INTRODUCTION thetic nervous system, has both pre- and postganglionic The autonomic nervous system (ANS) is a complex neural fibres. However, in general, the preganglionic fibres pass network largely responsible for the regulation of visceral uninterrupted to the organ that is to be controlled; function and maintenance of homeostasis of the internal postganglionic neurons are located in the wall of the organ.3 environment.1 This is achieved primarily through interac- The neurotransmitter for all preganglionic and para- tions with the endocrine system and via autonomic reflexes. sympathetic postganglionic fibres is acetylcholine. All The latter comprise specialized sensory receptors in the postganglionic sympathetic nerves are adrenergic except viscera which provide information regarding visceral for those fibres innervating the sweat glands which are function to higher ANS centres in the brain. At these sites cholinergic.1 sensory information is processed and integrated, and appropriate autonomic motor responses to the viscera are Higher centres relayed through the ANS efferent system. In many The supraspinal integration of ANS function is accomplished circumstances, the ANS reflexes are capable of responding by a complex interaction of many brainstem, mesencephalic very quickly to alterations in the internal environment and and cortical areas, the hypothalamus being the principal can rapidly return the system to its homeostatic baseline. higher centre for integration of ANS function. It receives sensory afferents as well as connections from the limbic GENERAL ANATOMICAL ORGANIZATION system and sensorimotor cortex, and exerts its effects via The ANS has two major divisions: the sympathetic and interactions with the endocrine system and through 2 parasympathetic nervous systems. -

Current Strategies in the Management of Irritable Bowel Syndrome
icine- O ed pe M n l A a c n c r e e s t s n I Internal Medicine: Open Access Randall et al., Intern Med 2014, S1:006 DOI: 10.4172/2165-8048.S1-006 ISSN: 2165-8048 Review Article Open Access Current Strategies in the Management of Irritable Bowel Syndrome Randall CW1,2*, Saurez AV3 and Zaga-Galante J3 1Clinical Professor of Medicine, University of Texas Health Science Ctr, San Antonio, USA 2CEO, Gastroenterology Research of America, USA 3Anahuac University, Mexico City, Mexico *Corresponding author: Charles W Randall, Clinical Professor of Medicine, University of Texas Health Science Ctr, San Antonio, USA and CEO, Gastroenterology Research of America, USA, Tel: (210) 410 2515; E-mail: [email protected] Rec date: Jan 17, 2014, Acc date: Feb 28, 2014, Pub date: Mar 09, 2014 Copyright: ©2014 Randall CW, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Irritable bowel syndrome (IBS) is one of the most studied and discussed problems in the field of gastroenterology, yet it often remains perplexing to both clinicians and patients. Some of the apprehension comes from a void of objective data that defines a diagnosis in most disorders. This level of comfort is not appreciated in the evaluation of IBS, where the art of medicine and subjective impressions are the cornerstones of proper assessment. Though this paper focuses on management, a review of pathophysiology and specific guidelines establishing a diagnosis of IBS will be addressed. -

Marine Microplankton Ecology Reading
Marine Microplankton Ecology Reading Microbes dominate our planet, especially the Earth’s oceans. The distinguishing feature of microorganisms is their small size, usually defined as less than 200 micrometers (µm); they are all invisible to the naked eye. As a group, sea microbes are extremely diverse, and extremely versatile with respect to their abilities to make and eat food. All marine microbes are too small to swim against the current and are therefore classified as plankton. First we will discuss several ways to classify marine microbes. 1. Size Planktonic marine organisms can be divided into the following size categories: Category Size femtoplankton <0.2 µm picoplankton 0.2-2 µm nanoplankton 2-20 µm microplankton 20-200 µm mesoplankton 200-2000 µm In this laboratory we are concerned with the microscopic portion of the plankton, less than 200 µm. These organisms are not visible to the naked eye (Figure 1). Figure 1. Size classes of marine plankton 2. Type A. Viruses Viruses are the smallest and simplest microplankton. They range from 0.01 to 0.3 um in diameter. Externally, viruses have a capsid, or protein coat. Viruses can also have simple or complex external morphologies with tail fibers and structures that are used to inject DNA or RNA into their host. Viruses have little internal morphology. They do not have a nucleus or organelles. They do not have chlorophyll. Inside a virus there is only nucleic acid, either DNA or RNA. Viruses do not grow and have no metabolism. Marine viruses are highly abundant. There are up to 10 billion in one liter of seawater! B. -
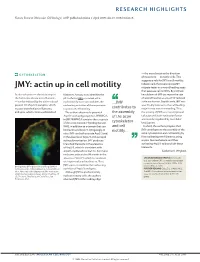
JMY: Actin up in Cell Motility Migrate Faster in a Wound Healing Assay That Assesses Cell Motility
RESEARCH HIGHLIGHTS Nature Reviews Molecular Cell Biology | AOP, published online 2 April 2009; doi:10.1038/nrm2678 — the area closest to the direction CYTOSKELETON of movement — in motile cells. This suggests a role for JMY in cell motility. Indeed, cells that overexpress JMY JMY: actin up in cell motility migrate faster in a wound healing assay that assesses cell motility. By contrast, Actin nucleation — the initial step in filaments. A study now identifies the knockdown of JMY decreases the rate the formation of new actin filaments p53 cofactor JMY as a novel actin of wound healing as a result of reduced — can be induced by the actin-related nucleation factor that combines the ...JMY actin nucleation. Significantly, JMY was protein 2/3 (Arp2/3) complex, which nucleating activities of these proteins specifically induced to the cell leading creates branched actin filaments, to promote cell motility. contributes to edge in response to wounding. Thus, and spire, which creates unbranched The authors observed a potential the assembly the activity of JMY as a transcriptional Arp2/3-activating sequence, WWWCA, of the actin cofactor and actin nucleation factor in JMY. WWWCA contains three repeats seems to be regulated by its cellular of the actin monomer-binding domain cytoskeleton localization. WH2, in addition to a domain that can and cell In short, the authors propose that bind actin and Arp2/3. Intriguingly, in motility... JMY contributes to the assembly of the vitro, JMY can both activate Arp2/3 and, actin cytoskeleton and cell motility by in the absence of Arp2/3, induce rapid first nucleating new filaments, using actin polymerization. -

Gastrointestinal Motility
Gastrointestinal Motility H. J. Ehrlein and M.Schemann 1. Motility of the stomach Anatomic regions of the stomach are the fundus, corpus (body), antrum and pylorus. The functional regions of the stomach do not correspond to the anatomic regions. Functionally, the stomach can be divided into the gastric reservoir and the gastric pump (Fig. 1). The gastric reservoir consists of the fundus and corpus. The gastric pump is represented by the area at which peristaltic waves occur: it includes the distal part of the corpus and the antrum. Due to different properties of the smooth muscle cells the gastric reservoir is characterised by tonic activity and the gastric pump by phasic activity. AB Gastric reservoir Fundus tonic contractions Pylorus Corpus Antrum Gastric pump phasic contractions Figure 1 . The stomach can be divided into three anatomic (A) and two functional regions (B) 1.1 Function of the gastric reservoir At the beginning of the 20 th century it was already observed that with increasing volume of the stomach the internal pressure of the stomach increases only slightly. In dogs, for instance, the increase in pressure is only 1.2 cm of water/100 ml volume. The small increase in gastric pressure indicates that the stomach does not behave like an elastic balloon but that it relaxes as it fills. Three kinds of gastric relaxation can be differentiated: a receptive, an adaptive and a feedback-relaxation of the gastric reservoir. The receptive relaxation consists of a brief relaxation during chewing and swallowing. The stimulation of mechano-receptors in the mouth and pharynx induces vago-vagal reflexes which cause a relaxation of the gastric reservoir (Fig. -

The Effect of Azide on Phototaxis in Chlamydomonas Reinhardi (Motility)
Proc. Nat. Acad. Sci. USA Vol. 71, No. 5, pp. 1824-1827, May 1974 The Effect of Azide on Phototaxis in Chlamydomonas reinhardi (motility) ROBERT L. STAVIS Department of Molecular Biology, Division of Biological Sciences, Albert Einstein College of Medicine, Bronx, New York 10461 Communicated by Alfred Gilman, February 25, 1974 ABSTRACT Phototaxis in Chlamydomonas reinhardi section of a cuvette. The maximum rate of accumulation was specifically inhibited by azide. The effect of azide was divided by the concentration of cells rapid and reversible, and did not depend upon the intensity .(AOD8wo/min) (ODwo) of actinic light. Under conditions of completely inhibited is the phototaxis coefficient, a measure of phototaxis indepen- phototaxis, azide had no effect on the number of motile dent of cell density. The actinic light used in these studies was cells in the population or on the rate of motility. The an Osram 150-W xenon lamp in an Oriel 6137 lamp housing effect was not related to changes in oxygen uptake or (Oriel Corp. of America, Stamford, Conn.). Light below 350 cellular ATP concentration. Apparently, a cellular com- ponent or process specifically involved in phototaxis is nm or above 650 nm was excluded by filtering the light source inactivated by azide. with an Oriel C-722-3900 long-pass filter, a G-774-4450 band-pass filter, and a G-776-7100 infrared-absorbing filter. The stimulus-response system that mediates the tactic be- The resulting light had a maximum intensity at 445 nm, with havior of microorganisms may be thought of as consisting a half-maximum band width of about 100 nm and an intensity of components that function as stimulus receptor, a transmis- of about 100 J/m2 per see at the phototaxis cuvette. -

Human Body- Digestive System
Previous reading: Human Body Digestive System (Organs, Location and Function) Science, Class-7th, Rishi Valley School Next reading: Cardiovascular system Content Slide #s 1) Overview of human digestive system................................... 3-4 2) Organs of human digestive system....................................... 5-7 3) Mouth, Pharynx and Esophagus.......................................... 10-14 4) Movement of food ................................................................ 15-17 5) The Stomach.......................................................................... 19-21 6) The Small Intestine ............................................................... 22-23 7) The Large Intestine ............................................................... 24-25 8) The Gut Flora ........................................................................ 27 9) Summary of Digestive System............................................... 28 10) Common Digestive Disorders ............................................... 31-34 How to go about this module 1) Have your note book with you. You will be required to guess or answer many questions. Explain your guess with reasoning. You are required to show the work when you return to RV. 2) Move sequentially from 1st slide to last slide. Do it at your pace. 3) Many slides would ask you to sketch the figures. – Draw them neatly in a fresh, unruled page. – Put the title of the page as the slide title. – Read the entire slide and try to understand. – Copy the green shade portions in the note book. 4) -

Actin-Based Motility of Pathogenic Bacteria
Journal of Cell Science 112, 1697-1708 (1999) 1697 Printed in Great Britain © The Company of Biologists Limited 1999 JCS9942 A comparative study of the actin-based motilities of the pathogenic bacteria Listeria monocytogenes, Shigella flexneri and Rickettsia conorii E. Gouin1, H. Gantelet1, C. Egile2, I. Lasa1,*, H. Ohayon3, V. Villiers1, P. Gounon3, P. J. Sansonetti2 and P. Cossart1,‡ 1Unité des Interactions Bactéries-Cellules, 2Unité de Pathogénie Microbienne Moléculaire, 3Station Centrale de Microscopie Electronique, Institut Pasteur, 25 and 28 Rue du Dr Roux, 75724 Paris Cedex 15, France *Present address: Dpto. Producción agraria, Universidad Pública de Navarra, Campus de Arrosadia s/n, Pamplona-31006, Spain ‡Author for correspondence (e-mail: [email protected]) Accepted 17 March; published on WWW 11 May 1999 SUMMARY Listeria monocytogenes, Shigella flexneri, and Rickettsia of actin with the S1 subfragment of myosin in infected cells conorii are three bacterial pathogens that are able to showed that the comet tails of Rickettsia have a structure polymerize actin into ‘comet tail’ structures and move strikingly different from those of L. monocytogenes or S. within the cytosol of infected cells. The actin-based flexneri. In Listeria and Shigella tails, actin filaments form motilities of L. monocytogenes and S. flexneri are known to a branching network while Rickettsia tails display longer require the bacterial proteins ActA and IcsA, respectively, and not cross-linked actin filaments. Immunofluorescence and several mammalian cytoskeleton proteins including studies revealed that the two host proteins, VASP and α- the Arp2/3 complex and VASP (vasodilator-stimulated actinin colocalized with actin in the tails of Rickettsia but phosphoprotein) for L. -

Kaplan USMLE Step 1 Prep: Which Substance Will Confirm Diagnosis?
Kaplan USMLE Step 1 prep: Which substance will confirm diagnosis? JUL 6, 2020 Staff News Writer If you’re preparing for the United States Medical Licensing Examination® (USMLE®) Step 1 exam, you might want to know which questions are most often missed by test-prep takers. Check out this example from Kaplan Medical, and read an expert explanation of the answer. Also check out all posts in this series. The AMA selected Kaplan as a preferred provider to support you in reaching your goal of passing the USMLE® or COMLEX-USA®. AMA members can save 30% on access to additional study resources, such as Kaplan’s Qbank and High-yield courses. Learn more. This month’s stumper A 55-year-old man is admitted to the hospital because of hematemesis. Measurement fasting serum gastrin levels show them to be 8-fold higher compared with a normal individual and an upper gastrointestinal endoscopy shows multiple ulcers in the duodenum. A multiple endocrine neoplasia type 1 is suspected. Administration of which of the following substances will most likely confirm the diagnosis? A. Cholecystokinin. B. Gastric inhibitory peptide. C. Motilin. D. Pentagastrin. E. Secretin. URL: https://www.ama-assn.org/residents-students/usmle/kaplan-usmle-step-1-prep-which-substance-will-confirm- diagnosis Copyright 1995 - 2021 American Medical Association. All rights reserved. The correct answer is E. Kaplan Medical explains why The patient has Zollinger-Ellison syndrome (ZES); a positive secretin stimulation test is diagnostic. Zollinger-Ellison syndrome: Caused by a gastrin-secreting tumor (gastrinoma) typically located in the pancreas or duodenal wall.