3 Macronutrient Digestion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Relationships Between the Autonomic Nervous System and the Pancreas Including Regulation of Regeneration and Apoptosis Recent Developments
ORIGINAL ARTICLE Relationships Between the Autonomic Nervous System and the Pancreas Including Regulation of Regeneration and Apoptosis Recent Developments Takayoshi Kiba, MD, PhD organ at birth, reaches its adult size and morphology after Abstract: Substantial new information has accumulated on the weaning (3 weeks of age). mechanisms of secretion, the development, and regulation of the gene In pancreatic regeneration after cholecystokinin analog expression, and the role of growth factors in the differentiation, growth, and regeneration of the pancreas. Many genes that are re- cerulein-induced acute pancreatitis, 2 separate peaks of DNA quired for pancreas formation are active after birth and participate in synthesis have been reported. The first peak corresponded with endocrine and exocrine cell functions. Although the factors that nor- duct cell and mesenchymal cell proliferation, and the second mally regulate the proliferation of the pancreas largely remain elu- peak was associated with acinar cell proliferation.1 However, sive, several factors to influence the growth have been identified. It in this model, islet cells did not regenerate. Formation of new was also reported that the pancreas was sensitive to a number of apop-  cells can take place via 2 pathways: replication of already totic stimuli. The autonomic nervous system influences many of the differentiated  cells and neogenesis from putative islet stem functions of the body, including the pancreas. In fact, the parasympa- cells. It is generally admitted that neogenesis mostly takes thetic nervous system and the sympathetic nervous system have op- place during fetal and neonatal life. In adulthood, little increase posing effects on insulin secretion from islet  cells; feeding-induced in the -cell number seems to occur. -

Physiology of the Pancreas
LECTURE IV: Physiology of the Pancreas EDITING FILE IMPORTANT MALE SLIDES EXTRA FEMALE SLIDES LECTURER’S NOTES 1 PHYSIOLOGY OF THE PANCREAS Lecture Four OBJECTIVES ● Functional Anatomy ● Major components of pancreatic juice and their physiologic roles ● Cellular mechanisms of bicarbonate secretion ● Cellular mechanisms of enzyme secretion ● Activation of pancreatic enzymes ● Hormonal & neural regulation of pancreatic secretion ● Potentiation of the secretory response Pancreas Lying parallel to and beneath the stomach, it is a large compound gland with most of its internal structure similar to that of the salivary glands. It is composed of: Figure 4-1 Endocrine portion 1-2% Exocrine portion 95% (Made of Islets of Langerhans) (Acinar gland tissues) Secrete hormones into the blood Made of acinar & ductal cells.1 - ● Insulin (beta cells; 60%) secretes digestive enzymes, HCO3 ● Glucagon (alpha cells; 25%) and water into the duodenum . ● Somatostatin (delta cells; 10%). Figure 4-2 Figure 4-3 ● The pancreatic digestive enzymes are secreted by pancreatic acini. ● Large volumes of sodium bicarbonate solution are secreted by the small ductules and larger ducts leading from the acini. ● Pancreatic juice is secreted in response to the presence of chyme in the upper portions of the small intestine. ● Insulin and Glucagon are crucial for normal regulation of glucose, lipid, and protein metabolism. FOOTNOTES 1. Acinar cells arrange themselves like clusters of grapes, that eventually release their secretions into ducts. Collection of acinar cells is called acinus, acinus and duct constitute one exocrine gland. 2 PHYSIOLOGY OF THE PANCREAS Lecture Four Pancreatic Secretion: ● Amount ≈ 1.5 L/day in an adult human. ● The major functions of pancreatic secretion: To neutralize the acids in the duodenal chyme to optimum range 1 (pH=7.0-8.0) for activity of pancreatic enzymes. -

Enteric Nervous System (ENS): 1) Myenteric (Auerbach) Plexus & 2
Enteric Nervous System (ENS): 1) Myenteric (Auerbach) plexus & 2) Submucosal (Meissner’s) plexus à both triggered by sensory neurons with chemo- and mechanoreceptors in the mucosal epithelium; effector motors neurons of the myenteric plexus control contraction/motility of the GI tract, and effector motor neurons of the submucosal plexus control secretion of GI mucosa & organs. Although ENS neurons can function independently, they are subject to regulation by ANS. Autonomic Nervous System (ANS): 1) parasympathetic (rest & digest) – can innervate the GI tract and form connections with ENS neurons that promote motility and secretion, enhancing/speeding up the process of digestion 2) sympathetic (fight or flight) – can innervate the GI tract and inhibit motility & secretion by inhibiting neurons of the ENS Sections and dimensions of the GI tract (alimentary canal): Esophagus à ~ 10 inches Stomach à ~ 12 inches and holds ~ 1-2 L (full) up to ~ 3-4 L (distended) Duodenum à first 10 inches of the small intestine Jejunum à next 3 feet of small intestine (when smooth muscle tone is lost upon death, extends to 8 feet) Ileum à final 6 feet of small intestine (when smooth muscle tone is lost upon death, extends to 12 feet) Large intestine à 5 feet General Histology of the GI Tract: 4 layers – Mucosa, Submucosa, Muscularis Externa, and Serosa Mucosa à epithelium, lamina propria (areolar connective tissue), & muscularis mucosae Submucosa à areolar connective tissue Muscularis externa à skeletal muscle (in select parts of the tract); smooth muscle (at least 2 layers – inner layer of circular muscle and outer layer of longitudinal muscle; stomach has a third layer of oblique muscle under the circular layer) Serosa à superficial layer made of areolar connective tissue and simple squamous epithelium (a.k.a. -
Digestive System
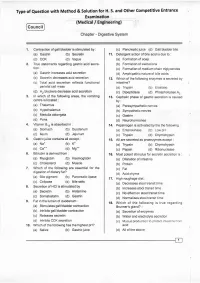
Type of Question with Method & Solution for H. S. and Other Competitive Entrance Examination (Medical / Engineering) Cou ncil Chapter - Digestive System '1. Contraction of gall bladder is stimulated by : (c) Pancreatic,uice (d) Gall bladder bile (a) Gastrin (b) Secretin 1r. Detergent action of bile acid is due to : (c) CCK (d) Vagus (a) Formation of soap 2. True statemenls regarding gastric acid secre- (b) Formation of zwitterions . tion: (c) Formation of medium chain triglycerides (a) Gastrin increases acid secretion (d) Amphipathic nature of bile acids (b) Secretin decreases acid secretion 12. Which of the following enzymes is secreted by (c) Total acid secretion reflects functional intestine? parietal cell mass (a) Trypsin (b) Elaslase (d). H2 blockers decrease acid secretion . (c) Dipeptidase (d) Phospholipase 42 3. ln which of the following areas, the vomiting 13. Cephalic phase of gastric secretion is caused centre is located : by: (a) Thalamus . (a) Parasympathetic nerves (b) Hypothalamus (b) Sympathetic nerves (c) Medulla oblongata (c) Gastrin (d) Pons (d) Neurohormones in : 4, Vitamin 8,, is absorbed '14. Pepsinogen is activated by lhe the following : (a) Stomach (b) Duodenum (a) Enterokinase (b) Low pH (c) lleum (d) Jejunum (c) Trypsin (d) Chymotrypsin 5. Gastricjuice contains all except : 15. All are secreted as proenzymes except : (a) Na" (b) K- (a) Trypsin (b) Chymotrypsin (c) Ca". (d) Ms.* (c) Pepsin (d) Ribonuclease Bilirubin is derived from : 6. 16. Most potent stimulus for secretin secretion is : . (a) Myoglobin (b) Haemoglobin (a) Dilatation of intestine (c) Cholesterol (d) Muscle (b) Protein 7. Which of the following are essential for the (c) Fat digestion of dietary fat? (d) Acid chyme (a) Bile plgment (b) Pancreatlc lipase 17. -

Digestive System Physiology of the Pancreas
Digestive System Physiology of the pancreas Dr. Hana Alzamil Objectives Pancreatic acini Pancreatic secretion Pancreatic enzymes Control of pancreatic secretion ◦ Neural ◦ Hormonal Secretin Cholecystokinin What are the types of glands? Anatomy of pancreas Objectives Pancreatic acini Pancreatic secretion Pancreatic enzymes Control of pancreatic secretion ◦ Neural ◦ Hormonal Secretin Cholecystokinin Histology of the Pancreas Acini ◦ Exocrine ◦ 99% of gland Islets of Langerhans ◦ Endocrine ◦ 1% of gland Secretory function of pancreas Acinar and ductal cells in the exocrine pancreas form a close functional unit. Pancreatic acini secrete the pancreatic digestive enzymes. The ductal cells secrete large volumes of sodium bicarbonate solution The combined product of enzymes and sodium bicarbonate solution then flows through a long pancreatic duct Pancreatic duct joins the common hepatic duct to form hepatopancreatic ampulla The ampulla empties its content through papilla of vater which is surrounded by sphincter of oddi Objectives Pancreatic acini Pancreatic secretion Pancreatic enzymes Control of pancreatic secretion ◦ Neural ◦ Hormonal Secretin Cholecystokinin Composition of Pancreatic Juice Contains ◦ Water ◦ Sodium bicarbonate ◦ Digestive enzymes Pancreatic amylase pancreatic lipase Pancreatic nucleases Pancreatic proteases Functions of pancreatic secretion Fluid (pH from 7.6 to 9.0) ◦ acts as a vehicle to carry inactive proteolytic enzymes to the duodenal lumen ◦ Neutralizes acidic gastric secretion Enzymes ◦ -

Behaviour of Digestive Enzymes in the Pancreatic Juice and Pancreas of Rats Fed on a Low-Protein Diet (3 P
Behaviour of digestive enzymes in the pancreatic juice and pancreas of rats fed on a low-protein diet (3 p. 100 of cereal protein) then on a balanced diet (23.5 p. 100 of mixed protein) O. Kheroua, J. Belleville To cite this version: O. Kheroua, J. Belleville. Behaviour of digestive enzymes in the pancreatic juice and pancreas of rats fed on a low-protein diet (3 p. 100 of cereal protein) then on a balanced diet (23.5 p. 100 of mixed protein). Reproduction Nutrition Développement, 1981, 21 (6A), pp.901-917. hal-00897907 HAL Id: hal-00897907 https://hal.archives-ouvertes.fr/hal-00897907 Submitted on 1 Jan 1981 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Behaviour of digestive enzymes in the pancreatic juice and pancreas of rats fed on a low-protein diet (3 p. 100 of cereal protein) then on a balanced diet (23.5 p. 100 of mixed protein) O. KHEROUA, J. BELLEVILLE Laboratoire de Physiologie de la Nutrition Université d’Oran, Algérie. * Laboratoire de Physiologie de la Nutrition UER Nutrition, BP 138, 21100 Dijon Cedex, France. Summary. The aim of this study in the rat was to determine the effect of a low-protein diet (3 p. -

Effect of Acid Infusion Into Various Levels of the Intestine on Gastric and Pancreatic Secretion in the Cat
Gut: first published as 10.1136/gut.10.9.749 on 1 September 1969. Downloaded from Gut, 1969, 10, 749-753 Effect of acid infusion into various levels of the intestine on gastric and pancreatic secretion in the cat S. J. KONTUREK, J. DUBIEL, AND B. GABRY9 From the Department ofMedicine, Medical School, Krakow, Poland SUMMARY Intraduodenal infusion of increasing amounts of hydrochloric acid solution results in a stepwise increase in the volume of pancreatic secretion and output of bicarbonate, reaching about 90 % of amounts attained with exogenous secretin infused intravenously in increasing doses. Acid infusion into the different regions of the intestine stimulates pancreatic secretion only from the duodenum and upper jejunum, suggesting that the area ofendogenous release of secretin by acid is confined to the upper part ofthe small bowel in the cat. Gastric acid secretion induced by pentagastrin, but not by histamine, is inhibited by acid perfusion of the duodenum. The acidification of other parts of the small intestine does not result in any change in gastric acid secretion induced either by pentagastrin or by histamine. Previous studies have shown that acidification of the ligament of Treitz, and the third in the ileum about 25 cm duodenum in the cat inhibits gastric acid secretion proximal to the caecum. and stimulates pancreatic secretion, due to the endogenous release of secretin (Konturek, Dubiel, SECRETORY PROCEDURE The secretory tests were started and and about two weeks after the cats hadrecoveredfrom surgery. Gabryg, 1969; Konturek, Gabrys, Dubiel, http://gut.bmj.com/ 1969). No study, however, has compared the relative effects on gastric and pancreatic secretion of acid infusions into various regions of the small intestine. -

Aloe Vera and the Human Digestive System Excerpts by Lawrence Plaskett, B.A., Ph.D., C.Chem., F.R.I.C
COMPANY NAME Aloe Vera and the Human Digestive System Excerpts By Lawrence Plaskett, B.A., Ph.D., C.Chem., F.R.I.C. Trials indicate that Aloe vera heals peptic ulcers, controls intestinal secretions to normal levels, influences the bowel flora, controls gastric and intestinal pH, improves the functioning of the pancreas and limits adverse bacteria in the colon, reducing putrification. The Normal Digestive System In looking closely at the functions of the Digestive System, it is much the usual thing to examine minutely the functions of its individual parts. Whilst it may well be necessary to do some analysis of that kind, it is usually far more instructive to consider the digestive system as a whole. The reason why this is so important is that the functions of each part of this system interact with those of every other part. Hence, if the digestive system is in difficulties, the job of restoring it to normal should not be tackled piecemeal, but rather in a completely wholistic manner. Before we can consider exactly what Aloe vera does within the Digestive System it is necessary to understand the normal functions of digestion and the more common forms of malfunction which may be encountered in practice. Whilst the first part may be accomplished by reading the appropriate chapter of any textbook of anatomy and physiology, asimple overall explanation is provided here by reference to the diagram below. The food, upon entering through the mouth and undergoing mastication, becomes mixed with the saliva. As saliva contains a starch digesting enzyme, salivary amylase, the digestion of starch begins almost at once. -

Stimulatory Effect Ofpancreozymin-Cholecystokinin on Calcium Secretion in Pancreatic Juice of Dogs 479
Gut: first published as 10.1136/gut.13.6.477 on 1 June 1972. Downloaded from Gut, 1972, 13, 477-482 Stimulatory effect of pancreozymin-cholecystokinin on calcium secretion in pancreatic juice of dogs2'3 H. GOEBELL1, Ch. STEFFEN, AND Ch. BODE From the Department of Medicine, Philipps-Universitdt, Marburg/Lahn, Germany SUMMARY In four dogs with a permanent duodenal Thomas fistula the secretion ofcalcium, sodium, potassium, protein, and two pancreatic enzymes in pancreatic juice was studied. Infusion of secretin led to a decrease in concentration of calcium and of protein with increasing rates of fluid production. Pancreozymin-cholecystokininwas given in single injections superimposed on the secretin-stimulated flow of juice. This hormone stimulated the secretion of both calcium and enzyme protein in a parallel and closely correlated fashion. The secretion of this protein-bound calcium fraction I is assumed to occur in the acinar cell. A calcium fraction II, which was independent of protein secretion and pancreozymin stimulation, was demonstrated in concentrations of about 0.4 to 0.6 m-equiv/l. This fraction is thought to originate in the interstitial fluid. The secretion of two calcium-containing fluids is in accordance with the two-component theory of secretion proposed by Hollander and Birnbaum (1952). The concentration of sodium and potassium in pancreatic juice of dogs, using a permanent duodenal pancreatic juice has been found to lie in the same Thomas cannula. range as that in the serum under different rates of http://gut.bmj.com/ flow (Johnston and Ball, 1930; Solomon, 1952; Methods Dreiling and Janowitz, 1956); In contrast, it has been known since the investigations of Ball (1930) Four male mongrel dogs with a mean weight of 25 kg that the concentration of calcium in pancreatic were equipped under pentobarbital anaesthesia with juice, at 1-2 m-equiv/l, is much lower than in the a permanent duodenal cannula according to the serum. -

Recent Advances in Pancreatic Hormone Research R. G. LONG M.D., M.R.C.P
Postgrad Med J: first published as 10.1136/pgmj.59.691.277 on 1 May 1983. Downloaded from Postgraduate Medical Journal (May 1983) 59, 277-282 LEADING ARTICLE Recent advances in pancreatic hormone research R. G. LONG M.D., M.R.C.P. Gastrointestinal Laboratory, St Thomas' Hospital, London SEI 7EH Introduction investigated has been gastric inhibitory polypeptide (also known as glucose-dependent insulinotropic The pancreas secretes 4 major polypeptide hor- polypeptide or GIP) which is a 43 amino acid mones: insulin from the beta cells; pancreatic gluca- polypeptide found in the K cells of the duodenum gon from the alpha cells; somatostatin from the D and jejunum. GIP is released after oral (but not cells in the islets of Langerhans, and pancreatic intravenous) glucose and infusion studies have polypeptide (PP) from the PP cells which are spread shown that, when the blood glucose level is raised more diffusely through pancreatic exocrine and above normal fasting levels, GIP releases insulin. It endocrine tissue. Some or all of these 4 hormones therefore appears that GIP is an incretin, but it may also have paracrine effects; this means that the probably does not explain the whole effect (Sarson peptide is secreted locally and has metabolic effects and Bloom, 1981). This means that the search for copyright. on neighbouring cells. Gastrin is synthesized in G other incretins continues and it seems likely that cells in the foetal pancreas, but these cells disappear interest will now be turned towards the newly postnatally. Certain other polypeptides such as vaso- isolated glicentin. active intestinal polypeptide (VIP) have also been The effects of glycogenolysis and gluconeogenesis demonstrated in human pancreas, but appear pre- of pancreatic glucagon and its release by hypoglycae- dominantly localized to nerves; these substances, mia and infusions of alanine and arginine are well which were initially classified as 'gut hormones', are known. -

Pancreas and Fat/Lipid Digestion
Exocrine Pancreas Physiology Pancreatic Anatomy Pancreatic secretion Pancreatic enzymes Daniel S. Kamin MD Boston Children’s Hospital [email protected] Content Reviewers: Sohail Z. Husain, MD Veronique Morinville MD, FRCP(C) NASPGHAN Physiology Education Series Series Editors: Christine Waasdorp Hurtado, MD, MSCS, FAAP [email protected] Daniel Kamin, MD [email protected] Learning Objectives • Understand the normal development and anatomy of the pancreas • Understand the stimuli and cellular factors giving rise to pancreatic secretion • Know the mechanisms by which pancreatic enzymes are activated and remain functional • Be aware of age-related deficiency in exocrine pancreatic function Night blindness • A young man with morbid obesity undergoes roux-en-y gastric bypass. • 1 year later he notices that in the evening he falls down his stairs. • Vitamin A deficiency is diagnosed. Understanding the physiology of pancreatic and bile secretion, Used with permission intraluminal lipolysis, and micellar function explains why this happens! http://www.citelighter.com/science/surgery/knowledgecards/gastric-bypass Pancreas Physiology Overview • Bulk of bicarbonate secretion (more than what secreted in bile and from duodenum) • Enzymes for intra- luminal digestion • Secretin and CCK regulate • Maturational pancreatic insufficiency Used with permission Image from http://www.aboutcancer.com/pancreas1.htm Pancreatic Development • See Embryology and Anatomy of the Gastrointestinal Tract Pancreatic Microanatomy Pancreatic Acinar Secretory Products A • Proteases • Trypsinogen* • Chymotrypsinogen* A • Proelastase* • Procarboxypeptidase* • Procarboxypeptidase B* • Amylolytic enzyme • Amylase A • Lipases • Lipase • B Nonspecific esterase • Prophospholipase A2* • Nucleases • Deoxyribonuclease • Ribonuclease • Others • Pro-colipase* • Trypsin inhibitors A. Exocrine pancreas-- ascinar cells filled • Monitor peptid with secretory granules, cuboidal duct Stored and secreted in inactive form cells secrete bicarbonate-rich fluid B. -

ERCP) and Pure Pancreatic Juice Cytology in Patients with Pancreatic Disease
Gut: first published as 10.1136/gut.17.1.14 on 1 January 1976. Downloaded from Gut, 1976, 17, 14.21 Assessment of endoscopic retrograde cholangio- pancreatography (ERCP) and pure pancreatic juice cytology in patients with pancreatic disease A. R. W. HATFIELDI, A. SMITHIES, R. WILKINS, AND A. J. LEVI From Northwick Park Hospital and Clinical Research Centre, Middlesex SUMMARY Pure pancreatic juice has been collected from 61 patients at the time of endoscopic retrograde cholangio-pancreatography (ERCP) for the purpose of cytodiagnosis. The ERCP and cytological findings are discussed. Pure pancreatic juice cytology may help in the interpretation of the pancreatogram in both pancreatitis and pancreatic carcinoma. In patients with pancreatic carcinoma, ERCP alone was diagnostic in 65%, cytology alone in 54 %. By combining these two approaches, a diagnostic result was obtained in 92 % of patients. The introduction of ERCP to Great Britain in the trast medium. In two-thirds of the patients studied, last four years has been a major advance in the pancreatic juice was collected before the injection investigation of pancreatic and biliary disease of contrast medium. (Cotton, 1972). This investigation is both practical Pancreatic juice was collected in all but two and safe, but there can be considerable difficulties patients using the following two methods. in the interpretation of the pancreatogram. Although the exfoliative cytology of duodenal Method I The cannula was inserted through the http://gut.bmj.com/ aspirates for the diagnosis of pancreatic disease has papilla of Vater into the pancreatic duct to a depth been practised since 1949 (Lemon and Byrnes, 1949), of 2-3 cm.