Malignant Catarrhal Fever
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Camelids: New Players in the International Animal Production Context
Tropical Animal Health and Production (2020) 52:903–913 https://doi.org/10.1007/s11250-019-02197-2 REVIEWS Camelids: new players in the international animal production context Mousa Zarrin1 & José L. Riveros2 & Amir Ahmadpour1,3 & André M. de Almeida4 & Gaukhar Konuspayeva5 & Einar Vargas- Bello-Pérez6 & Bernard Faye7 & Lorenzo E. Hernández-Castellano8 Received: 30 October 2019 /Accepted: 22 December 2019 /Published online: 2 January 2020 # Springer Nature B.V. 2020 Abstract The Camelidae family comprises the Bactrian camel (Camelus bactrianus), the dromedary camel (Camelus dromedarius), and four species of South American camelids: llama (Lama glama),alpaca(Lama pacos)guanaco(Lama guanicoe), and vicuña (Vicugna vicugna). The main characteristic of these species is their ability to cope with either hard climatic conditions like those found in arid regions (Bactrian and dromedary camels) or high-altitude landscapes like those found in South America (South American camelids). Because of such interesting physiological and adaptive traits, the interest for these animals as livestock species has increased considerably over the last years. In general, the main animal products obtained from these animals are meat, milk, and hair fiber, although they are also used for races and work among other activities. In the near future, climate change will likely decrease agricultural areas for animal production worldwide, particularly in the tropics and subtropics where competition with crops for human consumption is a major problem already. In such conditions, extensive animal production could be limited in some extent to semi-arid rangelands, subjected to periodical draughts and erratic patterns of rainfall, severely affecting conventional livestock production, namely cattle and sheep. -

Boselaphus Tragocamelus</I>
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln USGS Staff -- Published Research US Geological Survey 2008 Boselaphus tragocamelus (Artiodactyla: Bovidae) David M. Leslie Jr. U.S. Geological Survey, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/usgsstaffpub Leslie, David M. Jr., "Boselaphus tragocamelus (Artiodactyla: Bovidae)" (2008). USGS Staff -- Published Research. 723. https://digitalcommons.unl.edu/usgsstaffpub/723 This Article is brought to you for free and open access by the US Geological Survey at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in USGS Staff -- Published Research by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. MAMMALIAN SPECIES 813:1–16 Boselaphus tragocamelus (Artiodactyla: Bovidae) DAVID M. LESLIE,JR. United States Geological Survey, Oklahoma Cooperative Fish and Wildlife Research Unit and Department of Natural Resource Ecology and Management, Oklahoma State University, Stillwater, OK 74078-3051, USA; [email protected] Abstract: Boselaphus tragocamelus (Pallas, 1766) is a bovid commonly called the nilgai or blue bull and is Asia’s largest antelope. A sexually dimorphic ungulate of large stature and unique coloration, it is the only species in the genus Boselaphus. It is endemic to peninsular India and small parts of Pakistan and Nepal, has been extirpated from Bangladesh, and has been introduced in the United States (Texas), Mexico, South Africa, and Italy. It prefers open grassland and savannas and locally is a significant agricultural pest in India. It is not of special conservation concern and is well represented in zoos and private collections throughout the world. DOI: 10.1644/813.1. -
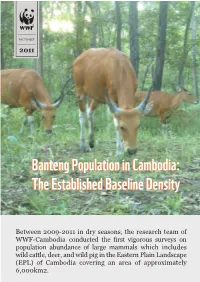
Bantengbanteng Populationpopulation Inin Cambodia:Cambodia: Thethe Establishedestablished Baselinebaseline Densitydensity © FA / WWF-Cambodia
FACTSHEET 2011 BantengBanteng PopulationPopulation inin Cambodia:Cambodia: TheThe EstablishedEstablished BaselineBaseline DensityDensity © FA / WWF-Cambodia Between 2009-2011 in dry seasons, the research team of WWF-Cambodia conducted the first vigorous surveys on population abundance of large mammals which includes wild cattle, deer, and wild pig in the Eastern Plain Landscape (EPL) of Cambodia covering an area of approximately 6,000km2. Banteng: Globally Endangered Species Banteng (bos javanicus) is a species of wild cattle that historically inhabited deciduous and semi- evergreen forests from Northeast India and Southern Yunnan through mainland Southeast Asia and Peninsular Malaysia to Borneo and Java. Since 1996, banteng has been listed by IUCN as globally endangered on the basis of an inferred decline over the last 30 years of more than 50%. Banteng is most likely the ancestor of Southeast Asia’s domestic cattle and it is considered to be one of the most beautiful and graceful of all wild cattle species. In Cambodia, banteng populations have decreased dramatically since the late 1960s. Poaching to sell the meat and horns as trophies constitutes a major threat to remnant populations even though banteng is legally protected. © FA / WWF-Cambodia Monitoring Banteng Population in the Landscape Knowledge of animal populations is central to understanding their status and to planning their management and conservation. That is why WWF has several research projects in the EPL to gain more information about the biodiversity values of PPWS and MPF. Regular line transect surveys are conducted to collect data on large ungulates like banteng, gaur, and Eld’s deer--all potential prey species for large carnivores including tigers. -

Mule Deer and Antelope Staff Specialist Peregrine Wolff, Wildlife Health Specialist
STATE OF NEVADA Steve Sisolak, Governor DEPARTMENT OF WILDLIFE Tony Wasley, Director GAME DIVISION Brian F. Wakeling, Chief Mike Cox, Bighorn Sheep and Mountain Goat Staff Specialist Pat Jackson, Predator Management Staff Specialist Cody McKee, Elk Staff Biologist Cody Schroeder, Mule Deer and Antelope Staff Specialist Peregrine Wolff, Wildlife Health Specialist Western Region Southern Region Eastern Region Regional Supervisors Mike Scott Steve Kimble Tom Donham Big Game Biologists Chris Hampson Joe Bennett Travis Allen Carl Lackey Pat Cummings Clint Garrett Kyle Neill Cooper Munson Sarah Hale Ed Partee Kari Huebner Jason Salisbury Matt Jeffress Kody Menghini Tyler Nall Scott Roberts This publication will be made available in an alternative format upon request. Nevada Department of Wildlife receives funding through the Federal Aid in Wildlife Restoration. Federal Laws prohibit discrimination on the basis of race, color, national origin, age, sex, or disability. If you believe you’ve been discriminated against in any NDOW program, activity, or facility, please write to the following: Diversity Program Manager or Director U.S. Fish and Wildlife Service Nevada Department of Wildlife 4401 North Fairfax Drive, Mailstop: 7072-43 6980 Sierra Center Parkway, Suite 120 Arlington, VA 22203 Reno, Nevada 8911-2237 Individuals with hearing impairments may contact the Department via telecommunications device at our Headquarters at 775-688-1500 via a text telephone (TTY) telecommunications device by first calling the State of Nevada Relay Operator at 1-800-326-6868. NEVADA DEPARTMENT OF WILDLIFE 2018-2019 BIG GAME STATUS This program is supported by Federal financial assistance titled “Statewide Game Management” submitted to the U.S. -

Level of Estradiol 17-Β Serum and Ovarian Folliculare Dynamics in Short Estrous Cycle of Bali Cattle
LEVEL OF ESTRADIOL 17-β SERUM AND OVARIAN FOLLICULARE DYNAMICS IN SHORT ESTROUS CYCLE OF BALI CATTLE C.M Airin1, P. P. Putro2, P. Astuti3 and E. Baliarti4 1Faculty of Veterinary Medicine, Gadjah Mada University, Jl Fauna No. 2 Karangmalang Yogyakarta - Indonesia 2Department of Obstetric and Gynaecology, Faculty of Veterinary Medicine, Gadjah Mada University, Jl Fauna No 2 Karangmalang Yogyakarta - Indonesia 3Department of Physiology, Faculty of Veterinary Medicine, Gadjah Mada University, Jl Fauna No 2 Karangmalang Yogyakarta - Indonesia, 4Department of Animal Production, Faculty of Animal Husbandry, Gadjah Mada University,Jl Fauna No 2 Karangmalang Yogyakarta - Indonesia Corresponding E-mail : [email protected] Received December 27, 2013; Accepted February 10, 2014 ABSTRAK Penelitian ini bertujuan untuk mengetahui kadar estradiol 17-β dan gambaran dinamika folikel yang menyertai kejadian siklus estrus yang pendek Penelitian ini menggunakan 7 ekor sapi Bali yang ada di Kebun Pengembangan Penelitian Pertanian, dan Peternakan (KP4), betina, umur 2 tahun, sehat dan bersiklus estrus normal. Pengukuran diameter folikel menggunakan ultrasonografi (USG) dan darah diambil dari vena jugularus dimulai hari pertama setiap hari dalam waktu yang bersamaan selama 3 siklus. Kadar estradiol 17-β dianalisis menggunakan metode Enzyme Immuno Assay (EIA) Hasil penelitian menunjukkan 4 ekor sapi Bali mempunyai siklus estrus pendek (n=7) diantara siklus estrus normal. Sapi Bali tersebut mempunyai 1 gelombang perkembangan folikel dengan panjang siklus 7-10 hari, diameter folikel ovulasi maksimal dan kadar estradiol 17-β menyerupai siklus normal. Kadar tertinggi estradiol 17-β pada siklus tersebut 107,77 ± 55.94 pg/ml pada hari ke 7-10 saat ukuran folikel ovulasi mencapai 10.5 ± 0,38 mm. -

Cuticle and Cortical Cell Morphology of Alpaca and Other Rare Animal Fibres
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Repositorio Institucional Universidad Nacional Autónoma de Chota The Journal of The Textile Institute ISSN: 0040-5000 (Print) 1754-2340 (Online) Journal homepage: http://www.tandfonline.com/loi/tjti20 Cuticle and cortical cell morphology of alpaca and other rare animal fibres B. A. McGregor & E. C. Quispe Peña To cite this article: B. A. McGregor & E. C. Quispe Peña (2017): Cuticle and cortical cell morphology of alpaca and other rare animal fibres, The Journal of The Textile Institute, DOI: 10.1080/00405000.2017.1368112 To link to this article: http://dx.doi.org/10.1080/00405000.2017.1368112 Published online: 18 Sep 2017. Submit your article to this journal Article views: 7 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=tjti20 Download by: [181.64.24.124] Date: 25 September 2017, At: 13:39 THE JOURNAL OF THE TEXTILE INSTITUTE, 2017 https://doi.org/10.1080/00405000.2017.1368112 Cuticle and cortical cell morphology of alpaca and other rare animal fibres B. A. McGregora and E. C. Quispe Peñab aInstitute for Frontier Materials, Deakin University, Geelong, Australia; bNational University Autonoma de Chota, Chota, Peru ABSTRACT ARTICLE HISTORY The null hypothesis of the experiments reported is that the cuticle and cortical morphology of rare Received 6 March 2017 animal fibres are similar. The investigation also examined if the productivity and age of alpacas were Accepted 11 August 2017 associated with cuticle morphology and if seasonal nutritional conditions were related to cuticle scale KEYWORDS frequency. -

Antelope, Deer, Bighorn Sheep and Mountain Goats: a Guide to the Carpals
J. Ethnobiol. 10(2):169-181 Winter 1990 ANTELOPE, DEER, BIGHORN SHEEP AND MOUNTAIN GOATS: A GUIDE TO THE CARPALS PAMELA J. FORD Mount San Antonio College 1100 North Grand Avenue Walnut, CA 91739 ABSTRACT.-Remains of antelope, deer, mountain goat, and bighorn sheep appear in archaeological sites in the North American west. Carpal bones of these animals are generally recovered in excellent condition but are rarely identified beyond the classification 1/small-sized artiodactyl." This guide, based on the analysis of over thirty modem specimens, is intended as an aid in the identifi cation of these remains for archaeological and biogeographical studies. RESUMEN.-Se han encontrado restos de antilopes, ciervos, cabras de las montanas rocosas, y de carneros cimarrones en sitios arqueol6gicos del oeste de Norte America. Huesos carpianos de estos animales se recuperan, por 10 general, en excelentes condiciones pero raramente son identificados mas alIa de la clasifi cacion "artiodactilos pequeno." Esta glia, basada en un anaIisis de mas de treinta especlmenes modemos, tiene el proposito de servir como ayuda en la identifica cion de estos restos para estudios arqueologicos y biogeogrMicos. RESUME.-On peut trouver des ossements d'antilopes, de cerfs, de chevres de montagne et de mouflons des Rocheuses, dans des sites archeologiques de la . region ouest de I'Amerique du Nord. Les os carpeins de ces animaux, generale ment en excellente condition, sont rarement identifies au dela du classement d' ,I artiodactyles de petite taille." Le but de ce guide base sur 30 specimens recents est d'aider aidentifier ces ossements pour des etudes archeologiques et biogeo graphiques. -
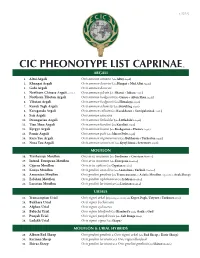
Cic Pheonotype List Caprinae©
v. 5.25.12 CIC PHEONOTYPE LIST CAPRINAE © ARGALI 1. Altai Argali Ovis ammon ammon (aka Altay Argali) 2. Khangai Argali Ovis ammon darwini (aka Hangai & Mid Altai Argali) 3. Gobi Argali Ovis ammon darwini 4. Northern Chinese Argali - extinct Ovis ammon jubata (aka Shansi & Jubata Argali) 5. Northern Tibetan Argali Ovis ammon hodgsonii (aka Gansu & Altun Shan Argali) 6. Tibetan Argali Ovis ammon hodgsonii (aka Himalaya Argali) 7. Kuruk Tagh Argali Ovis ammon adametzi (aka Kuruktag Argali) 8. Karaganda Argali Ovis ammon collium (aka Kazakhstan & Semipalatinsk Argali) 9. Sair Argali Ovis ammon sairensis 10. Dzungarian Argali Ovis ammon littledalei (aka Littledale’s Argali) 11. Tian Shan Argali Ovis ammon karelini (aka Karelini Argali) 12. Kyrgyz Argali Ovis ammon humei (aka Kashgarian & Hume’s Argali) 13. Pamir Argali Ovis ammon polii (aka Marco Polo Argali) 14. Kara Tau Argali Ovis ammon nigrimontana (aka Bukharan & Turkestan Argali) 15. Nura Tau Argali Ovis ammon severtzovi (aka Kyzyl Kum & Severtzov Argali) MOUFLON 16. Tyrrhenian Mouflon Ovis aries musimon (aka Sardinian & Corsican Mouflon) 17. Introd. European Mouflon Ovis aries musimon (aka European Mouflon) 18. Cyprus Mouflon Ovis aries ophion (aka Cyprian Mouflon) 19. Konya Mouflon Ovis gmelini anatolica (aka Anatolian & Turkish Mouflon) 20. Armenian Mouflon Ovis gmelini gmelinii (aka Transcaucasus or Asiatic Mouflon, regionally as Arak Sheep) 21. Esfahan Mouflon Ovis gmelini isphahanica (aka Isfahan Mouflon) 22. Larestan Mouflon Ovis gmelini laristanica (aka Laristan Mouflon) URIALS 23. Transcaspian Urial Ovis vignei arkal (Depending on locality aka Kopet Dagh, Ustyurt & Turkmen Urial) 24. Bukhara Urial Ovis vignei bocharensis 25. Afghan Urial Ovis vignei cycloceros 26. -
Vega Etal Procroyalsocb Synchronous Diversification
Canterbury Christ Church University’s repository of research outputs http://create.canterbury.ac.uk Please cite this publication as follows: Frantz, Laurent A. F., Rudzinski, A., Mansyursyah Surya Nugraha, A., Evin, A., Burton, J., Hulme-Beaman, A., Linderholm, A., Barnett, R., Vega, R., Irving-Pease, E., Haile, J., Allen, R., Leus, K., Shephard, J., Hillyer, M., Gillemot, S., van den Hurk, J., Ogle, S., Atofanei, C., Thomas, M., Johansson, F., Haris Mustari, A., Williams, J., Mohamad, K., Siska Damayanti, C., Djuwita Wiryadi, I., Obbles, D., Mona, S., Day, H., Yasin, M., Meker, S., McGuire, J., Evans, B., von Rintelen, T., Hoult, S., Searle, J., Kitchener, A., Macdonald, A., Shaw, D., Hall, R., Galbusera, P. and Larson, G. (2018) Synchronous diversification of Sulawesi’s iconic artiodactyls driven by recent geological events. Proceedings of the Royal Society B: Biological Sciences. Link to official URL (if available): http://dx.doi.org/10.1098/rspb.2017.2566. This version is made available in accordance with publishers’ policies. All material made available by CReaTE is protected by intellectual property law, including copyright law. Any use made of the contents should comply with the relevant law. Contact: [email protected] Synchronous diversification of Sulawesi’s iconic artiodactyls driven by recent geological events Authors Laurent A. F. Frantz1,2,a,*, Anna Rudzinski3,*, Abang Mansyursyah Surya Nugraha4,c,*, , Allowen Evin5,6*, James Burton7,8*, Ardern Hulme-Beaman2,6, Anna Linderholm2,9, Ross Barnett2,10, Rodrigo Vega11 Evan K. Irving-Pease2, James Haile2,10, Richard Allen2, Kristin Leus12,13, Jill Shephard14,15, Mia Hillyer14,16, Sarah Gillemot14, Jeroen van den Hurk14, Sharron Ogle17, Cristina Atofanei11, Mark G. -

Late Quaternary Extinction of Ungulates in Sub-Saharan Africa: a Reductionist's Approach
Late Quaternary Extinction of Ungulates in Sub-Saharan Africa: a Reductionist's Approach Joris Peters Ins/itu/ für Palaeoanatomie, Domestikationsforschung und Geschichte der Tiermedizin, Universität München. Feldmochinger Strasse 7, D-80992 München, Germany AchilIes Gautier Laboratorium VDor Pa/eonlo/agie, Seclie Kwartairpaleo1ltologie en Archeozoölogie, Universiteit Gent, Krijgs/aon 2811S8, B-9000 Gent, Belgium James S. Brink National Museum, P. 0. Box 266. Bloemfontein 9300. Republic of South Africa Wim Haenen Instituut voor Gezandheidsecologie, Katholieke Universiteit Leuven, Capucijnenvoer 35, B-3000 Leuven, Belgium (Received 24 January 1992, revised manuscrip/ accepted 6 November 1992) Comparative osteomorphology and sta ti st ical analysis cf postcranial limb bone measurements cf modern African wildebeest (Collnochaetes), eland (Taura/ragus) and Africa n buffala (Sy" cer"s) have heen applied to reassess the systematic affiliations between these bovids and related extinct Pleistocene forms. The fossil sam pies come from the sites of Elandsfontein (Cape Province) .nd Flarisb.d (Orange Free State) in South Afrie • . On the basis of differenees in skull morphology and size of the appendicular skeleton between fossil and modern blaek wildebeest (ConlJochaeus gnou). the subspecies name anliquus, proposed earlier to designate the Pleistoeene form, ean be retained. The same taxonomie level is accepted for the large Pleistocene e1and, whieh could be named Taurolragus oryx antiquus. The long horned or giant buffa1o, Pelorovis antiquus, can be inc1uded in the polymorphous Syncerus caffer stock and could therefore be called Syncerus caffer antiquus. The ecology of Pleistocene and modern Connochaetes, Taurolragus and Syncerus is discussed. A relationship between herbivore body size and c1imate, as Bergmann's Rule predicts, could not be demonstrated. -

Reproductive Seasonality in Captive Wild Ruminants: Implications for Biogeographical Adaptation, Photoperiodic Control, and Life History
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2012 Reproductive seasonality in captive wild ruminants: implications for biogeographical adaptation, photoperiodic control, and life history Zerbe, Philipp Abstract: Zur quantitativen Beschreibung der Reproduktionsmuster wurden Daten von 110 Wildwiederkäuer- arten aus Zoos der gemässigten Zone verwendet (dabei wurde die Anzahl Tage, an denen 80% aller Geburten stattfanden, als Geburtenpeak-Breite [BPB] definiert). Diese Muster wurden mit verschiede- nen biologischen Charakteristika verknüpft und mit denen von freilebenden Tieren verglichen. Der Bre- itengrad des natürlichen Verbreitungsgebietes korreliert stark mit dem in Menschenobhut beobachteten BPB. Nur 11% der Spezies wechselten ihr reproduktives Muster zwischen Wildnis und Gefangenschaft, wobei für saisonale Spezies die errechnete Tageslichtlänge zum Zeitpunkt der Konzeption für freilebende und in Menschenobhut gehaltene Populationen gleich war. Reproduktive Saisonalität erklärt zusätzliche Varianzen im Verhältnis von Körpergewicht und Tragzeit, wobei saisonalere Spezies für ihr Körpergewicht eine kürzere Tragzeit aufweisen. Rückschliessend ist festzuhalten, dass Photoperiodik, speziell die abso- lute Tageslichtlänge, genetisch fixierter Auslöser für die Fortpflanzung ist, und dass die Plastizität der Tragzeit unterstützend auf die erfolgreiche Verbreitung der Wiederkäuer in höheren Breitengraden wirkte. A dataset on 110 wild ruminant species kept in captivity in temperate-zone zoos was used to describe their reproductive patterns quantitatively (determining the birth peak breadth BPB as the number of days in which 80% of all births occur); then this pattern was linked to various biological characteristics, and compared with free-ranging animals. Globally, latitude of natural origin highly correlates with BPB observed in captivity, with species being more seasonal originating from higher latitudes. -

Species of the Day: Banteng
Images © Brent Huffman / Ultimate Ungulate © Brent Huffman Species of the Day: Banteng The Banteng, Bos javanicus, is listed as ‘Endangered’ on the IUCN Red List of Threatened SpeciesTM. A species of wild cattle, the Banteng occurs in Southeast Asia from Myanmar to Indonesia, with a large introduced population in northern Australia. The Banteng has been eradicated from much of its historical range, and the remaining wild population, estimated at no more than 8,000 individuals, is continuing to decline. Habitat loss Geographical range and hunting present the greatest threats to its survival, with the illegal trade in meat and horns www.iucnredlist.org still being widespread in Southeast Asia. www.asianwildcattle.org Help Save Species Although the Banteng is legally protected across its range and occurs in a number of www.arkive.org protected areas, the natural resources of reserves in Southeast Asia often continue to be exploited. The northern Australian population may offer a conservation alternative, although genetic studies hint that the stock may originate from domesticated Bali cattle. Fortunately, a captive population is maintained worldwide which, if managed effectively and supplemented occasionally, can provide a buffer against total extinction, and offer the potential for future re- introductions into the wild. The production of the IUCN Red List of Threatened Species™ is made possible through the IUCN Red List Partnership: Species of the Day IUCN (including the Species Survival Commission), BirdLife is sponsored by International, Conservation International, NatureServe and Zoological Society of London..