2019 PROVINCIAL GUIDELINE Trauma Services BC
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Request for Decision
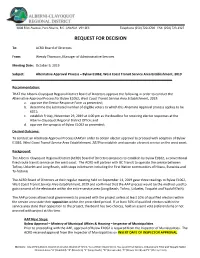
3008 Fifth Avenue, Port Alberni, B.C. CANADA V9Y 2E3 Telephone (250) 720-2700 FAX: (250) 723-1327 REQUEST FOR DECISION To: ACRD Board of Directors From: Wendy Thomson, Manager of Administrative Services Meeting Date: October 9, 2019 Subject: Alternative Approval Process – Bylaw E1062, West Coast Transit Service Area Establishment, 2019 Recommendation: THAT the Alberni-Clayoquot Regional District Board of Directors approve the following in order to conduct the Alternative Approval Process for Bylaw E1062, West Coast Transit Service Area Establishment, 2019: a. approve the Elector Response Form as presented; b. determine the estimated number of eligible voters to which this Alternate Approval process applies to be 6021; c. establish Friday, November 29, 2019 at 4:00 pm as the deadline for receiving elector responses at the Alberni-Clayoquot Regional District Office; and d. approve the synopsis of Bylaw E1062 as presented; Desired Outcome: To conduct an Alternate Approval Process (AAP) in order to obtain elector approval to proceed with adoption of Bylaw E1062, West Coast Transit Service Area Establishment, 2019 to establish and operate a transit service on the west coast. Background: The Alberni-Clayoquot Regional District (ACRD) Board of Directors proposes to establish by bylaw E0162, a conventional fixed route transit service on the west coast. The ACRD will partner with BC Transit to operate the service between Tofino, Ucluelet and Long Beach, with stops in between including the First Nation communities of Hitacu, Esowista and Ty-histanis. The ACRD Board of Directors at their regular meeting held on September 11, 2019 gave three readings to Bylaw E1062, West Coast Transit Service Area Establishment, 2019 and confirmed that the AAP process would be the method used to gain consent of the electorate within the entire service area (Long Beach, Tofino, Ucluelet, Toquaht and Yuułuʔiłʔatḥ). -

Spirits of Our Whaling Ancestors
Spirits of Our Whaling Ancestors SpiritS of our Whaling anceStorS Revitalizing Makah and Nuu-chah-nulth Traditions charlotte coté Foreword by MiCah MCCarty A Capell Family Book University of Washington Press Seattle & London UBC Press Vancouver & Toronto the CaPell faMily endoWed Book Fund supports the publication of books that deepen the understanding of social justice through historical, cultural, and environmental studies. Preference is given to books about the American West and to outstanding first books in order to foster scholarly careers. © 2010 by the University of Washington Press Library of Congress Cataloging-in-Publica- Printed in the United States of America tion Data and Library and Archives Canada Design by Thomas Eykemans Cataloging in Publication can be found at the 15 14 13 12 11 10 5 4 3 2 1 end of the book. All rights reserved. No part of this publica- The paper used in this publication is acid-free tion may be reproduced or transmitted in and 90 percent recycled from at least 50 per- any form or by any means, electronic or cent post-consumer waste. It meets the mini- mechanical, including photocopy, record- mum requirements of American National ing, or any information storage or retrieval Standard for Information Sciences—Perma- system, without permission in writing from nence of Paper for Printed Library Materials, the publisher. ANSI Z39.48–1984.∞ Published in the United States of America by frontisPieCe: Whaler photograph by University of Washington Press Edward S. Curtis; Courtesy Royal British P.o. Box 50096, Seattle, Wa 98145 U.s.a. Columbia Museum, Victoria. www.washington.edu/uwpress Published in Canada by UBC Press University of British Columbia 2029 West Mall, Vancouver, B.C. -

IDP-List-2012.Pdf
INFANT DEVELOPMENT PROGRAMS OF BRITISH COLUMBIA Revised January 2012 Website: www.idpofbc.ca 1 Contact information for each Program including addresses and telephone numbers is listed on the pages noted below. This information is also available on our website: www.idpofbc.ca *Aboriginal Infant Development Program Pages 2-3 VANCOUVER COASTAL REGION Vancouver Sheway Richmond *So-Sah-Latch Health & Family Centre, N Vancouver North Shore Sea to Sky, Squamish Burnaby Sunshine Coast, Sechelt New Westminster Powell River Coquitlam *Bella Coola Ridge Meadows, Maple Ridge Pages 4-5 FRASER REGION Delta *Kla-how-eya, Surrey Surrey/White Rock Upper Fraser Valley Langley Pages 6-8 VANCOUVER ISLAND REGION Victoria * Laichwiltach Family Life Society *South Vancouver Island AIDP *Nuu-chah-nulth Tribal Council, Gold River Cowichan Valley, Duncan *‘Namgis First Nation, Alert Bay *Tsewultun Health Centre, Duncan *Quatsino Indian Band, Coal Harbour Nanaimo North Island, Port Hardy Port Alberni *Gwa’Sala-‘Nakwaxda’xw Family Services, Pt. Hardy *Nuu-chah-nulth Tribal Council, Port Alberni* Klemtu Health Clinic, Port Hardy *Nuu-chah-nulth Tribal Council, Tofino *Kwakiutl Indian Band, Port Hardy Oceanside, Qualicum Beach Comox Valley, Courtenay Campbell River Pages 9-12 INTERIOR REGION Princeton *First Nations Friendship Centre Nicola Valley, Merritt Kelowna *Nzen’man’ Child & Family, Lytton *KiLowNa Friendship Society, Kelowna Lillooet South Okanagan, Penticton; Oliver Kamloops *Lower Similkameen Indian Band, Keremeos Clearwater Boundary, Grand Forks South Cariboo, 100 Mile House West Kootenay, Castlegar Williams Lake Creston *Bella Coola East Kootenay, Cranbrook; Invermere Salmon Arm Golden *Splatstin, Enderby Revelstoke Vernon Pages 13-14 NORTH REGION Quesnel Golden Kitimat Robson*Splatsin, Valley Enderby Prince RupertRevelstoke Prince George Queen Charlotte Islands Vanderhoof Mackenzie *Tl’azt’en Nation, Tachie South Peace, Dawson Creek Burns Lake Fort St. -

Uvic Thesis Template
Ts’a7inwa (gooseneck barnacles) as a proxy for archaeological efforts to understand shellfish as food in Nuu-chah-nulth territories by Meaghan Efford Bachelor of Arts (Honours), University of Victoria, 2016 A Thesis Submitted in Partial Fulfillment of the Requirements for the Degree of MASTER OF ARTS in the Department of Anthropology © Meaghan Efford, 2019 University of Victoria All rights reserved. This thesis may not be reproduced in whole or in part, by photocopy or other means, without the permission of the author. We acknowledge with respect the Lekwungen peoples on whose traditional territory the university stands and the Songhees, Esquimalt and WSÁNEĆ peoples whose historical relationships with the land continue to this day. ii Supervisory Committee Ts’a7inwa (gooseneck barnacles) as a proxy for archaeological efforts to understand shellfish as food in Nuu-chah-nulth territories by Meaghan Efford Bachelor of Arts (Honours), University of Victoria, 2016 Supervisory Committee Dr. Iain McKechnie, Supervisor Department of Anthropology Dr. Quentin Mackie, Departmental Member Department of Anthropology iii Abstract Supervisory Committee Dr. Iain McKechnie, Supervisor Department of Anthropology Dr. Quentin Mackie, Departmental Member Department of Anthropology This thesis examines the comparative abundance of shellfish from archaeological assemblages on the west coast of Vancouver Island in Nuu- chah-nulth territories. Eighteen sites spanning the Nuu-chah-nulth region emphasize the diversity in invertebrate foods that have been consumed 5000-150 years ago: Yaksis Cave, Loon Cave, and Hesquiat Village at Hesquiat Harbour; Chesterman Beach; Spring Cove; Ts’ishaa, Ch’ituukwachisht (North and South), Tl’ihuuw’a, Shiwitis, Huumuuwaa, Maktl7ii, Huts’atswilh, Kakmakimilh, Kiix7iin, and Huu7ii. -

Strathcona Park Trails Guide Special
STRATHCONA PARK TRAILS GUIDE SPECIAL Hiking Guide NootkaWILDWILD Island ISLEISLE Canada’sCanada’s WestWest CoastCoast AdventureAdventure MagazineMagazine ININ THETHE WAKEWAKE OFOF CAPTAINCAPTAIN VANCOUVERVANCOUVER A CLIMBER’S LIFELIFE CAVINGCAVING ININ THAILANDTHAILAND 3Chancesto WIN Apairoftickets to FREE ISSUE #12 AUGUST-SEPTEMBER, 2000 see page 26 for details www.wildislemagazine.bc.ca HIKE NOOTKA ISLAND The Resort at Cape Mudge Quadra Island BEACHFRONT CABIN . Only Getaway .95* September 16 - 30, 2000 $119 * based on quad occupancy 2 Bedroom With Jacuzzi Bathtub Gas Fireplace Kitchenette Us! 1-800-665-7745 [email protected] Tel: (250) 285-2042 Fax: (250) 285-2532 CCONTENTONTENTSS Cover: Curtis Lyon, South Ridge of Victoria Peak. Photo: Philip Stone BC Parks View Point p9 Volunteering in Paradise Gabe Jutras, Kwisatz Haderach 5.11d, Crest Creek Photo: Josie Boulding Linvin’ the Dream p10 Contents: The life of the Surfer at Long Beach. unsponsored climber Photo: Corrie Wright Strathcona Park p13 An overview of the hiking trails in BC’s oldest park Thai Caves p17 Islanders Abroad Underground adventure in Thailand Mt Colonel Foster p19 Guide to Vancouver Island’s alpine climbing mecca Benighted on Mt Klitsa p21 A lesson earned and a lesson learned In the Wake of Vancouver p22 The explorations of Cpt Vancouver on BC’s west coast. Happenings p26 Coming events on the west coast 3Chancesto WIN Apairoftickets to see page 26 for details west coast adventure magazine • www.wildislemagazine.bc.ca • CENTRE PULLOUT - NOOTKA ISLAND - HIKING -

Pre-Hospital Triage and Transport Guidelines for Adult and Pediatric Major Trauma in British Columbia
2019 PROVINCIAL GUIDELINE Pre-hospital Triage and Transport Guidelines for Adult and Pediatric Major Trauma in British Columbia Trauma Services BC A service of the Provincial Health Services Authority Contents Foreword ..........................................................................................................................................................................................3 Introduction ....................................................................................................................................................................................4 Adult and Pediatric Pre-hospital Trauma Triage Guidelines – Principles .........................................................................5 Step One – Physiological ................................................................................................................................................... 6 Step Two – Anatomical ........................................................................................................................................................7 Step Three – Mechanism ................................................................................................................................................... 8 Step Four – Special Considerations .................................................................................................................................. 8 Pre-hospital Trauma Triage Standard – British Columbia .....................................................................................................9 -
![Management Plan for the Olympia Oyster (Ostrea Conchaphila) in Canada [PROPOSED]](https://docslib.b-cdn.net/cover/4890/management-plan-for-the-olympia-oyster-ostrea-conchaphila-in-canada-proposed-494890.webp)
Management Plan for the Olympia Oyster (Ostrea Conchaphila) in Canada [PROPOSED]
PROPOSED SPECIES AT RISK ACT Management Plan Series Management Plan for the Olympia Oyster (Ostrea conchaphila) in Canada Olympia Oyster May 2009 About the Species at Risk Act Management Plan Series What is the Species at Risk Act (SARA)? SARA is the Act developed by the federal government as a key contribution to the common national effort to protect and conserve species at risk in Canada. SARA came into force in 2003, and one of its purposes is “to manage species of special concern to prevent them from becoming endangered or threatened.” What is a species of special concern? Under SARA, a species of special concern is a wildlife species that could become threatened or endangered because of a combination of biological characteristics and identified threats. Species of special concern are included in the SARA List of Wildlife Species at Risk. What is a management plan? Under SARA, a management plan is an action-oriented planning document that identifies the conservation activities and land use measures needed to ensure, at a minimum, that a species of special concern does not become threatened or endangered. For many species, the ultimate aim of the management plan will be to alleviate human threats and remove the species from the List of Wildlife Species at Risk. The plan sets goals and objectives, identifies threats, and indicates the main areas of activities to be undertaken to address those threats. Management plan development is mandated under Sections 65–72 of SARA (http://www.sararegistry.gc.ca/approach/act/default_e.cfm). A management plan has to be developed within three years after the species is added to the List of Wildlife Species at Risk. -

Retail Availabilities Onni Group
DECEMBER 2018 RETAIL AVAILABILITIES ONNI GROUP [email protected] | 604.602.7711 | ONNI.COM | 1 RICHMOND, BC IMPERIAL LANDING Address : Bayview Street Company : Onni Group Contact : Hilary Turnbull Phone : 604.602.7711 BUILDING FEATURES • High exposure retail landmark in Steveston Village • Close proximity to Fisherman’s Wharf • Approximately 30 minute drive to Downtown Vancouver AVAILABILITY BUILDING 1 - 6,974 SF - Available immediately BUILDING 3 - 1,789 SF - Available immediately BUILDING 2 - 16,143 SF - Available immediately BUILDING 4 - 6,027 SF - Available immediately PORT MOODY, BC SUTER BROOK VILLAGE Address : 220 Brew Street Company : Onni Group Contact : Hilary Turnbull Phone : 604.602.7711 BUILDING FEATURES • Ground floor retail opportunity • Walking distance from the Evergreen SkyTrain Line • Join Thrifty’s, TD, Vancity, Starbucks, and BC LDB • Approximately 30 minutes from Downtown Vancouver AVAILABILITY Up to 22,600 SF of retail - LEASED 792 SF of ground floor retail space - Available March 1, 2019 COQUITLAM, BC BROOKMERE Address : 528 North Road Company : Onni Group Contact : Hilary Turnbull Phone : 604.602.7711 BUILDING FEATURES • New construction • Ground floor retail • Transit - oriented, at Lougheed Town Centre SkyTrain Station • Occupancy approximately Q2 2019 • Unit equipped for full service restaurant AVAILABILITY CRU #1 - 2,552 SF - Available Q1 2019 - LAST UNIT! CRU #2 - 1,380 SF - Under Contract 2 | ONNI RETAIL AVAILABLE PROPERTIES | DECEMBER 2018 | 300 - 550 ROBSON STREET, VANCOUVER, BC V6B 2B7 BURNABY, BC 3355 -

Sailing Directions (Enroute)
PUB. 154 SAILING DIRECTIONS (ENROUTE) ★ BRITISH COLUMBIA ★ Prepared and published by the NATIONAL GEOSPATIAL-INTELLIGENCE AGENCY Bethesda, Maryland © COPYRIGHT 2007 BY THE UNITED STATES GOVERNMENT NO COPYRIGHT CLAIMED UNDER TITLE 17 U.S.C. 2007 TENTH EDITION For sale by the Superintendent of Documents, U.S. Government Printing Office Internet: http://bookstore.gpo.gov Phone: toll free (866) 512-1800; DC area (202) 512-1800 Fax: (202) 512-2250 Mail Stop: SSOP, Washington, DC 20402-0001 Preface 0.0 Pub. 154, Sailing Directions (Enroute) British Columbia, 0.0NGA Maritime Domain Website Tenth Edition, 2007, is issued for use in conjunction with Pub. http://www.nga.mil/portal/site/maritime 120, Sailing Directions (Planning Guide) Pacific Ocean and 0.0 Southeast Asia. Companion volumes are Pubs. 153, 155, 157, 0.0 Courses.—Courses are true, and are expressed in the same 158, and 159. manner as bearings. The directives “steer” and “make good” a 0.0 Digital Nautical Chart 26 provides electronic chart coverage course mean, without exception, to proceed from a point of for the area covered by this publication. origin along a track having the identical meridianal angle as the 0.0 This publication has been corrected to 21 July 2007, includ- designated course. Vessels following the directives must allow ing Notice to Mariners No. 29 of 2007. for every influence tending to cause deviation from such track, and navigate so that the designated course is continuously Explanatory Remarks being made good. 0.0 Currents.—Current directions are the true directions toward 0.0 Sailing Directions are published by the National Geospatial- which currents set. -

Reduced Annualreport1972.Pdf
PROVINCE OF BRITISH COLUMBIA DEPARTMENT OF RECREATION AND CONSERVATION HON. ROBERT A. WILLIAMS, Minister LLOYD BROOKS, Deputy Minister REPORT OF THE Department of Recreation and Conservation containing the reports of the GENERAL ADMINISTRATION, FISH AND WILDLIFE BRANCH, PROVINCIAL PARKS BRANCH, BRITISH COLUMBIA PROVINCIAL MUSEUM, AND COMMERCIAL FISHERIES BRANCH Year Ended December 31 1972 Printed by K. M. MACDONALD, Printer to tbe Queen's Most Excellent Majesty in right of the Province of British Columbia. 1973 \ VICTORIA, B.C., February, 1973 To Colonel the Honourable JOHN R. NICHOLSON, P.C., O.B.E., Q.C., LLD., Lieutenant-Governor of the Province of British Columbia. MAY IT PLEASE YOUR HONOUR: Herewith I beg respectfully to submit the Annual Report of the Department of Recreation and Conservation for the year ended December 31, 1972. ROBERT A. WILLIAMS Minister of Recreation and Conservation 1_) VICTORIA, B.C., February, 1973 The Honourable Robert A. Williams, Minister of Recreation and Conservation. SIR: I have the honour to submit the Annual Report of the Department of Recreation and Conservation for the year ended December 31, 1972. LLOYD BROOKS Deputy Minister of Recreation and Conservation CONTENTS PAGE Introduction by the Deputy Minister of Recreation and Conservation_____________ 7 General Administration_________________________________________________ __ ___________ _____ 9 Fish and Wildlife Branch____________ ___________________ ________________________ _____________________ 13 Provincial Parks Branch________ ______________________________________________ -

Vital Signs Report
CLAYOQUOT SOUND BIOSPHERE REGION’S 2018 Welcome to the Clayoquot Sound Biosphere Region’s Vital Signs® 2018 Table of Contents From the Vital Signs Research Team About Vital Signs 2 “We hope the 2018 Vital Signs report ¸ Grounded in the Nuu-chah-nulth (nuucaanuł) ¸ ˇ informs and inspires dialogue and principle of hišukniš cawaak, everything is one, Vital Our Region 3 collaboration to further our collective Signs 2018 can help us to understand the complex Cycle of Poverty efforts to build healthy communities and changing systems in which we live and the necessary pathways we need to navigate in order to in Our Region: and achieve sustainable development.” Inspiring Action support sustainable ecosystems and¸ communities. One of these pathways is nuucaanułˇ language for Change 4 Tammy Dorward and Catherine Thicke revitalization. This year, we’ve worked with a regional Co-chairs, Board of Directors Environment 5-6 committee of elders¸ and language keepers to incor- Clayoquot Biosphere Trust porate nuucaanułˇ throughout the report. Climate Change Impacts 7-8 We’ve collected a range of local data to highlight pri- ority areas for community-wide action and listened People & Work 9 From our Executive Director closely to community concerns. We’ve heard that Income Inequality 10 I am pleased to present our 2018 Vital Signs report. our young people are struggling with mental health Vital Signs is a valuable tool for understanding our issues and that they lack youth programs. Families Housing 11 progress toward achieving all aspects of sustainabili- are challenged with rising housing costs and the ty—cultural, social, economic, and environmental. -

DMO= Destination Marketing Organisation)
BACKGROUNDER A Destination BC Co-op Marketing Partnerships Program 2017/18 Participating Communities (*DMO= Destination Marketing Organisation) Consortium Region Approved DBC Funding Gold Rush Circle Route (CRD Electoral Area C, CRD Electoral Area F, District of Wells, Cariboo Chilcotin $16,000 Likely & District Chamber of Commerce, Coast Barkerville Historic Town) Great Bear Project (Tourism Prince Rupert, Bella Coola Valley Tourism, West Chilcotin Cariboo Chilcotin $68,800 Tourism Association) Coast Cariboo Calling (City of Williams Lake, City of Quesnel, Cariboo Regional District, 100 Mile Cariboo Chilcotin $18,936 House, Williams Lake Indian Band, X’atsull Coast (Soda Creek) Indian Band) Gold Rush Trail (Barkerville, Wells, Quesnel, Xat’sull, Williams Lake, Cariboo Regional Cariboo Chilcotin $40,000 District (multiple electoral areas), 100 Mile Coast and Vancouver, House, Clinton, Lillooet, Bridge River Valley Coast and Mountains (SLRD Area A), Yale, Hope, Abbotsford, New Westminster) MyKootenays (Tourism Fernie, Cranbrook Tourism, Tourism Kimberley, Invermere Kootenay Rockies $20,000 Panorama DMO, Tourism Radium, Regional District of East Kootenay, Elk Valley Cultural Consortium (Arts Council, Museum, Heritage Sites, Fernie & Sparwood Chambers, District of Elkford) Columbia Valley (Invermere Panorama DMO, Fairmont Business Association, Tourism Kootenay Rockies $85,000 Radium Hot Springs Columbia Valley Golf Association, Copper Point Resort, Fairmont Creek Property Rentals, Bighorn Meadows Resort, The Residences at Fairmont Ridge)