H1 Antihistamines Current Status and Future Directions F
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

XYZAL (Levocetirizine Dihydrochloride)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Patients with end-stage renal impairment at less than 10 mL/min These highlights do not include all the information needed to use XYZAL creatinine clearance or patients undergoing hemodialysis (2.3, 4) safely and effectively. See full prescribing information for XYZAL. • Children 6 to 11 years of age with renal impairment (2.3, 4) ® XYZAL (levocetirizine dihydrochloride) ------------------------WARNINGS AND PRECAUTIONS----------------------- 5 mg tablets 2.5 mg/5 mL (0.5 mg/mL) oral solution • Avoid engaging in hazardous occupations requiring complete mental Initial U.S. Approval: 1995 alertness such as driving or operating machinery when taking XYZAL (5.1). ---------------------------RECENT MAJOR CHANGES--------------------------- • Avoid concurrent use of alcohol or other central nervous system Dosage and Administration (2) 01/2008 depressants with XYZAL (5.1). Dosage and Administration, Adults & Children 12 Years & Older (2.1) 01/2008 ------------------------------ADVERSE REACTIONS------------------------------ Dosage and Administration, Children 6 to 11 Years (2.2) 01/2008 The most common adverse reactions (rate ≥2% and > placebo) were ---------------------------INDICATIONS AND USAGE---------------------------- somnolence, nasopharyngitis, fatigue, dry mouth, and pharyngitis in subjects XYZAL is a histamine H1-receptor antagonist indicated for: 12 years of age and older, and pyrexia, somnolence, cough, and epistaxis in • The relief of symptoms associated with seasonal and perennial allergic -

New York State Medicaid Drug Utilization Review Board Meeting Agenda
New York State Medicaid Drug Utilization Review Board Meeting Agenda The Drug Utilization Review (DUR) Board will meet on April 27, 2016, from 9:00 a.m. to 4:00 p.m., Meeting Room 6, Concourse, Empire State Plaza, Albany, New York Agenda Items A. Preferred Drug Program (PDP) The DUR Board will review therapeutic classes listed below, as they pertain to the PDP. The DUR Board will review clinical and financial information, to recommend preferred and non-preferred drugs. For therapeutic classes currently subject to the PDP^, the DUR Board will only consider clinical information which is new since the previous review of the therapeutic class and then consider financial information. New clinical information may include a new drug or drug product information, new indications, new safety information or new published clinical trials (comparative evidence is preferred, or placebo controlled when no head-to-head trials are available). Information in abstract form alone, posters, or unpublished data are poor quality evidence for the purpose of re-review and submission is discouraged. Those wishing to submit new clinical information must do so in an electronic format by April 12, 2016 or the Board may not have ample time to review the information. ^ The current preferred and non-preferred status of drugs subject to the Preferred Drug List (PDL) may be viewed at https://newyork.fhsc.com/downloads/providers/NYRx_PDP_PDL.pdf 1. Non-Steroidal Anti-Inflammatory Drugs (NSAIDS) – Prescription (Previous review date: April 22, 2015) Anaprox DS (naproxen -
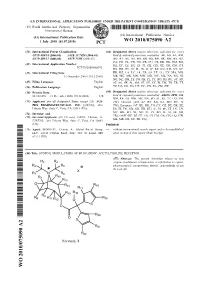
Wo 2010/075090 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 1 July 2010 (01.07.2010) WO 2010/075090 A2 (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C07D 409/14 (2006.01) A61K 31/7028 (2006.01) kind of national protection available): AE, AG, AL, AM, C07D 409/12 (2006.01) A61P 11/06 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/US2009/068073 HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 15 December 2009 (15.12.2009) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, (26) Publication Language: English TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/122,478 15 December 2008 (15.12.2008) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, (71) Applicant (for all designated States except US): AUS- ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, PEX PHARMACEUTICALS, INC. -

Ophthalmic Antihistamines
Ophthalmics for Allergic Conjunctivitis Review 04/12/2011 Copyright © 2004 - 2011 by Provider Synergies, L.L.C. All rights reserved. Printed in the United States of America. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage and retrieval system without the express written consent of Provider Synergies, L.L.C. All requests for permission should be mailed to: Attention: Copyright Administrator Intellectual Property Department Provider Synergies, L.L.C. 10101 Alliance Rd, Ste 201 Cincinnati, Ohio 45242 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, -

Medication Instructions for Allergy Patients
MEDICATION INSTRUCTIONS FOR ALLERGY PATIENTS Drugs which contain antihistamine or have antihistaminic effects can result in negative reactions to skin testing. As a result, it may not be possible to properly interpret skin test results, and testing may have to be repeated at a later date. While this list is extensive, it is NOT all inclusive (particularly of the various brand names). Discontinue ALL antihistamines including the following medications seven (7) days prior to skin testing (unless longer time specified): Antihistamines – Generic name (Brand name(s)): Cetirizine (Zyrtec, Zyrtec-D) Hydroxyzine (Vistaril, Atarax) Desloratadine (Clarinex) Levocetirizine (Xyzal) Fexofenadine (Allegra, Allegra-D) Loratadine (Claritin, Claritin-D, Alavert) Diphenhydramine (Aleve PM, Benadryl, Bayer P.M., Benylin, Contac P.M., Doans P.M, Excedrin PM, Legatrin P.M.. Nytol, Tylenol Nighttime, Unisom, Zzzquil) Chlorpheniramine (Aller-Chlor, Allerest, Alka Seltzer Plus, Chlor-Trimeton, Comtrex, Contac, Co-Pyronil, Coricidin, CTM, Deconamine, Dristan, Dura-tap, Naldecon, Ornade Spansules, Rondec, Sinutab, Teldrin, Triaminic, Triaminicin, Tylenol Allergy) Azatadine (Optimine, Trinalin) Doxylamine (Nyquil) Brompheniramine (Bromfed, Dimetane, Dimetapp) Meclizine (Antivert) Carbinoxamine (Clistin, Rondec) Pheniramine Clemastine (Tavist) Phenyltoloxamine (Nadecon) Cyclizine (Marezine) Promethazine (Phenergan) Cyprohepatidine (Periactin) (9 days) Pyrilamine (Mepyramine) Dexbrompheniramine (Drixoral) Quinacrine (Atabrine) Dexchlorpheniramine (Extendryl, Polaramine) -

MEDICATIONS to AVOID PRIOR to ALLERGY SKIN TESTING Allergy
MEDICATIONS TO AVOID PRIOR TO ALLERGY SKIN TESTING Allergy testing requires the ‘histamine response’ in order to be accurate and reliable. There are many types of antihistamines. Antihistamines are found in many different medicines, either as a single drug or mixed with a combination of chemicals. Please review all medicines you take (including Over-The-Counter) in order to make your allergy testing appointment most efficient and accurate. Generic names are in all lower case, trade names Capitalized. Oral antihistamines to be stopped 3 (THREE) days prior to your appointment: - brompheniramine (Actifed, Atrohist, Dimetapp, Drixoral) - cetirizine (Zyrtec, Zyrtec D) - chlopheniramine (Chlortrimeton, Deconamine, Kronofed A, Novafed A, Rynatan, Tussinex) - clemastine (Tavist, Antihist) - cyproheptadine (Periactin) - diphenhydramine (Benadryl, Allernix, Nytol) - doxylamine (Bendectin, Nyquil) - hydroxyzine (Atarax, Marax, Vistaril) - levocetirizine (Xyzal) - promethazine (Phenergan) Oral antihistamines to be stopped 7 (SEVEN) days prior to your appointment: - desloratadine (Clarinex) - fexofenadine (Allegra, Allegra D) - loratadine (Claritin, Claritin D, Alavert) Nose spray and eye drop antihistamines to stop 5 (FIVE) days prior to your appointment: - azelastine (Astelin, Astepro, Dymista, Optivar) - bepotastine (Bepreve) - ketotifen (Zaditor, Alaway) - olapatadine (Pataday, Patanase) - pheniramine (Visine A, Naphcon A) – OK to stop for 2 days Antacid medications (different type of antihistamine) to stop 3 (THREE) days prior to your appointment: - cimetidine (Tagamet) - famotidine (Pepcid) - ranitidine (Zantac) Note: Antihistamines are found in many over the counter medications, including Tylenol Allergy, Actifed Cold and Allergy, Alka-Seltzer Plus Cold with Cough Formula, and many others. Make sure you read and check the ingredients carefully and stop those containing antihistamines at least 3 (THREE) days prior to the appointment. -

Nasal Delivery of Aqueous Corticosteroid Solutions Nasale Abgabe Von Wässrigen Corticosteroidlösungen Administration Nasale De Solutions Aqueuses De Corticostéroïdes
(19) TZZ _¥__T (11) EP 2 173 169 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A01N 43/04 (2006.01) A61K 31/715 (2006.01) 21.05.2014 Bulletin 2014/21 (86) International application number: (21) Application number: 08781216.0 PCT/US2008/068872 (22) Date of filing: 30.06.2008 (87) International publication number: WO 2009/003199 (31.12.2008 Gazette 2009/01) (54) NASAL DELIVERY OF AQUEOUS CORTICOSTEROID SOLUTIONS NASALE ABGABE VON WÄSSRIGEN CORTICOSTEROIDLÖSUNGEN ADMINISTRATION NASALE DE SOLUTIONS AQUEUSES DE CORTICOSTÉROÏDES (84) Designated Contracting States: • ZIMMERER, Rupert, O. AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Lawrence, KS 66047 (US) HR HU IE IS IT LI LT LU LV MC MT NL NO PL PT • SIEBERT, John, M. RO SE SI SK TR Olathe, KS 66061-7470 (US) (30) Priority: 28.06.2007 PCT/US2007/072387 (74) Representative: Dörries, Hans Ulrich et al 29.06.2007 PCT/US2007/072442 df-mp Dörries Frank-Molnia & Pohlman Patentanwälte Rechtsanwälte PartG mbB (43) Date of publication of application: Theatinerstrasse 16 14.04.2010 Bulletin 2010/15 80333 München (DE) (73) Proprietor: CyDex Pharmaceuticals, Inc. (56) References cited: Lenexa, KS 66214 (US) WO-A1-2005/065649 US-A1- 2006 194 840 US-A1- 2007 020 299 US-A1- 2007 020 330 (72) Inventors: • PIPKIN, James, D. Lawrence, KS 66049 (US) Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -
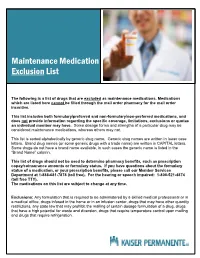
Mail Order Maintenance Medication Exclusion List
Maintenance Medication Exclusion List The following is a list of drugs that are excluded as maintenance medications. Medications which are listed here cannot be filled through the mail order pharmacy for the mail order incentive. This list includes both formulary/preferred and non-formulary/non-preferred medications, and does not provide information regarding the specific coverage, limitations, exclusions or quotas an individual member may have. Some dosage forms and strengths of a particular drug may be considered maintenance medications, whereas others may not. This list is sorted alphabetically by generic drug name. Generic drug names are written in lower case letters. Brand drug names (or some generic drugs with a trade name) are written in CAPITAL letters. Some drugs do not have a brand name available, in such cases the generic name is listed in the “Brand Name” column. This list of drugs should not be used to determine pharmacy benefits, such as prescription copay/coinsurance amounts or formulary status. If you have questions about the formulary status of a medication, or your prescription benefits, please call our Member Services Department at 1-888-681-7878 (toll free). For the hearing or speech impaired: 1-800-521-4874 (toll free TTY). The medications on this list are subject to change at any time. Exclusions: Any formulation that is required to be administered by a skilled medical professional or in a medical office, drugs infused in the home or in an infusion center, drugs that may have other quantity restrictions, any state law that may prohibit the mailing of certain dosage formulation of a drug, drugs that have a high potential for waste and diversion, drugs that require temperature control upon mailing and drugs that require refrigeration. -
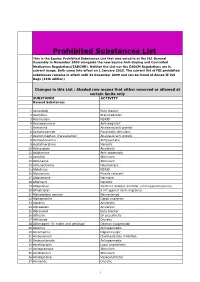
Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

Epinastine Hcl Ophthalmic Solution) 0.05% Sterile
NDA 21-565/S-005 Page 2 ELESTAT™ (epinastine HCl ophthalmic solution) 0.05% Sterile DESCRIPTION ELESTAT™ (epinastine HCl ophthalmic solution) 0.05% is a clear, colorless, sterile isotonic solution containing epinastine HCl, an antihistamine and an inhibitor of histamine release from the mast cell for topical administration to the eyes. Epinastine HCl is represented by the following structural formula: C16H15N3 • HCl Mol. Wt. 285.78 Chemical Name: 3-Amino-9, 13b-dihydro-1H-dibenz[c,f]imidazo[1,5-a]azepine hydrochloride Each mL contains: Active: Epinastine HCl 0.05% (0.5 mg/mL) equivalent to epinastine 0.044% (0.44mg/mL); Preservative: Benzalkonium chloride 0.01%; Inactives: Edetate disodium; purified water; sodium chloride; sodium phosphate, monobasic; and sodium hydroxide and/or hydrochloric acid (to adjust the pH). ELESTAT™ has a pH of approximately 7 and an osmolality range of 250 to 310 mOsm/kg. CLINICAL PHARMACOLOGY Epinastine is a topically active, direct H1-receptor antagonist and an inhibitor of the release of histamine from the mast cell. Epinastine is selective for the histamine H1-receptor and has affinity for the histamine H2 receptor. Epinastine also possesses affinity for the α1-, α2-, and 5-HT2 –receptors. Epinastine does not penetrate the blood/brain barrier and, therefore, is not expected to induce side effects of the central nervous system. Fourteen subjects, with allergic conjunctivitis, received one drop of ELESTAT™ in each eye twice daily for seven days. On day seven average maximum epinastine plasma concentrations of 0.04 ± 0.014 ng/ml were reached after about two hours indicating low systemic exposure. -

Antihistamines in the Treatment of Chronic Urticaria I Jáuregui,1 M Ferrer,2 J Montoro,3 I Dávila,4 J Bartra,5 a Del Cuvillo,6 J Mullol,7 J Sastre,8 a Valero5
Antihistamines in the treatment of chronic urticaria I Jáuregui,1 M Ferrer,2 J Montoro,3 I Dávila,4 J Bartra,5 A del Cuvillo,6 J Mullol,7 J Sastre,8 A Valero5 1 Service of Allergy, Hospital de Basurto, Bilbao, Spain 2 Department of Allergology, Clínica Universitaria de Navarra, Pamplona, Spain 3 Allergy Unit, Hospital La Plana, Villarreal (Castellón), Spain 4 Service of Immunoallergy, Hospital Clínico, Salamanca, Spain 5 Allergy Unit, Service of Pneumology and Respiratory Allergy, Hospital Clínic (ICT), Barcelona, Spain 6 Clínica Dr. Lobatón, Cádiz, Spain 7 Rhinology Unit, ENT Service (ICEMEQ), Hospital Clínic, Barcelona, Spain 8 Service of Allergy, Fundación Jiménez Díaz, Madrid, Spain ■ Summary Chronic urticaria is highly prevalent in the general population, and while there are multiple treatments for the disorder, the results obtained are not completely satisfactory. The second-generation H1 antihistamines remain the symptomatic treatment option of choice. Depending on the different pharmacokinetics and H1 receptor affi nity of each drug substance, different concentrations in skin can be expected, together with different effi cacy in relation to the histamine-induced wheal inhibition test - though this does not necessarily have repercussions upon clinical response. The antiinfl ammatory properties of the H1 antihistamines could be of relevance in chronic urticaria, though it is not clear to what degree they infl uence the fi nal therapeutic result. Before moving on to another therapeutic level, the advisability of antihistamine dose escalation should be considered, involving increments even above those approved in the Summary of Product Characteristics. Physical urticaria, when manifesting isolatedly, tends to respond well to H1 antihistamines, with the exception of genuine solar urticaria and delayed pressure urticaria. -

Trends in Prescription Medication Use Among Children and Adolescents— United States, 1999-2014
Supplementary Online Content Hales CM, Kit BK, Gu Q, Ogden CL. Trends in prescription medication use among children and adolescents— United States, 1999-2014. JAMA. doi:10.1001/jama.2018.5690 eTable. Classification of Prescription Medications Reported by NHANES Participants Aged 0-19 Years From 1999- 2000 to 2013-2014 by Therapeutic Class This supplementary material was provided by the authors to give readers additional informtion about their work. © 2018 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/27/2021 eTable. Classification of Prescription Medications Reported by NHANES Participants Aged 0-19 Years From 1999- 2000 to 2013-2014 by Therapeutic Class Therapeutic classes are based on the Lexicon Plus prescription medication database and only those classes reported in the manuscript are listed. ADHD Medications Antiadrenergic Agents, Centrally Acting Clonidine Guanfacine CNS Stimulants Amphetamines Amphetamine Amphetamine; Dextroamphetamine Dextroamphetamine Lisdexamfetamine Methylphenidate or Dexmethylphenidate Dexmethylphenidate Methylphenidate Other CNS Stimulant Pemoline Selective Norepinephrine Reuptake Inhibitor Atomoxetine Antibiotics Cephalosporins Cefadroxil Cephalexin Cefaclor Cefprozil Cefuroxime Loracarbef Cefdinir Cefditoren Cefixime Cefpodoxime Ceftibuten Ceftriaxone Glycopeptide Antibiotics Vancomycin H. Pylori Eradication Agents Amoxicillin; Clarithromycin; Lansoprazole Lincomycin Derivatives Clindamycin Macrolide Derivatives Telithromycin Azithromycin Clarithromycin