Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Tangled! Congolese Provincial Elites in a Web of Patronage
Researching livelihoods and services affected by conflict Tangled! Congolese provincial elites in a web of patronage Working paper 64 Lisa Jené and Pierre Englebert January 2019 Written by Lisa Jené and Pierre Englebert SLRC publications present information, analysis and key policy recommendations on issues relating to livelihoods, basic services and social protection in conflict-affected situations. This and other SLRC publications are available from www.securelivelihoods.org. Funded by UK aid from the UK Government, Irish Aid and the EC. Disclaimer: The views presented in this publication are those of the author(s) and do not necessarily reflect the UK Government’s official policies or represent the views of Irish Aid, the EC, SLRC or our partners. ©SLRC 2018. Readers are encouraged to quote or reproduce material from SLRC for their own publications. As copyright holder SLRC requests due acknowledgement. Secure Livelihoods Research Consortium Overseas Development Institute (ODI) 203 Blackfriars Road London SE1 8NJ United Kingdom T +44 (0)20 3817 0031 F +44 (0)20 7922 0399 E [email protected] www.securelivelihoods.org @SLRCtweet Cover photo: Provincial Assembly, Lualaba. Lisa Jené, 2018 (CC BY-NC-ND 2.0). B About us The Secure Livelihoods Research Consortium (SLRC) is a global research programme exploring basic services, livelihoods and social protection in fragile and conflict-affected situations. Funded by UK Aid from the UK Government’s Department for International Development (DFID), with complementary funding from Irish Aid and the European Commission (EC), SLRC was established in 2011 with the aim of strengthening the evidence base and informing policy and practice around livelihoods and services in conflict. -

WEEKLY BULLETIN on OUTBREAKS and OTHER EMERGENCIES Week 38: 15 - 21 September 2018 Data As Reported by 17:00; 21 September 2018
WEEKLY BULLETIN ON OUTBREAKS AND OTHER EMERGENCIES Week 38: 15 - 21 September 2018 Data as reported by 17:00; 21 September 2018 REGIONAL OFFICE FOR Africa WHO Health Emergencies Programme 2 52 43 11 New events Ongoing events Outbreaks Humanitarian crises Algeria 217 2 1 220 0 Mali 224 35 3 403 67 Niger 2 734 78 Sierra léone Chad 2 337 18 2 0 1 643 11 Guinea 3 062 Nigeria South Sudan 507 142 Liberia 2 837 51 36 0 Central African Ethiopia 127 0 2 663 1 49 13 Cameroon Republic 132 0 4 139 116 40 1 13 529 100 310 27 3 669 16 Democratic Republic Uganda Kenya 7 2 Sao Tome of Congo 1 0 Congo 95 11 Legend & Principe 23 8 5 0 381 1 1 0 147 99 Measles Humanitarian crisis 18 780 623 2 883 23 979 273 Seychelles Necrotising cellulitis/fasciitis Tanzania Monkeypox 22 22 2 829 57 5 813 0 Acute watery diarrhoea Lassa fever 37 0 3 739 68 Cholera Yellow fever Rift Valley fever Dengue fever Angola Typhoid fever Hepatitis E 954 19 1 Zambia Ebola virus disease 2 663 1 Plague Rabies Guinea Worm Zimbabwe Namibia Madagascar Mauritius Severe Acute Malnutrition cVDPV 1 983 8 5 891 38 899 3 Crimean-Congo haemorrhagic fever 15 5 Floods 2 554 24 Cases Countries reported in the document N Deaths Non WHO African Region WHO Member States with no ongoing events W E S Graded events † 2 6 5 Grade 3 events Grade 2 events Grade 1 events 32 22 20 41 Ungraded events ProtractedProtracted 3 3 events events Protracted 2 events ProtractedProtracted 1 1 events event 1 Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview Contents This Weekly Bulletin focuses on selected acute public health emergencies occurring in the WHO African Region. -

DRC Humanitarian Situation Report
DRC Humanitarian Situation Report July, 2018 SITUATION IN NUMBERS Highlights 4.49 million Internally Displaced - On 24 July 2018, the Ministry of Health officially declared the end of Persons (IDPs) (OCHA, April 2018) the Ebola epidemic outbreak in the province of Equator. UNICEF’s response on the Ebola outbreak can be found on Ebola’s latest 7,900,000 children in need of situation report and situation reports since the beginning of the humanitarian assistance (OCHA, Jan.2018) outbreak. - On 01 August 2018, the Ministry of Public Health in the DRC 2,000,000 children are suffering from declared an Ebola outbreak in the province of North Kivu. No Sever Acute malnutrition (DRC Cluster epidemiological link has been identified between the Equator and Nutrition, May 2018) North Kivu outbreak. UNICEF’s response on the North Kivu Ebola outbreak can be found on weekly basis on Ebola’s latest situation 15,158 cases of cholera reported since report January 2018 (Ministry of Health, July 2018) - During the month of July, 122,241 persons were provided with essential household items and shelter materials, through the Rapid Response to Population Movement (RRMP) mechanism UNICEF Appeal 2018 US$ 268 million UNICEF’s Response with Partners 32% of required funds available Funding status 2018* UNICEF Sector/Cluster UNICEF Total Cluster Total Target Results* Target Results* Funds Nutrition : # of children with SAM received 1,140,000 88,521 1,306,000 129,351 admitted for therapeutic care 21% $56M Health : # of children in humanitarian situations 979,784 652,396 -

African Development Bank Group Democratic Republic of Congo Support Project for Alternative Welfare of Children and Young People
AFRICAN DEVELOPMENT BANK GROUP DEMOCRATIC REPUBLIC OF CONGO SUPPORT PROJECT FOR ALTERNATIVE WELFARE OF CHILDREN AND YOUNG PEOPLE INVOLVED IN THE COBALT SUPPLY CHAIN (PABEA-COBALT) APPRAISAL REPORT Authoriezd Authorized Public Disclosure Authorized Disclosure Public Authorized Translated Document RDGC/AHHD March 2019 TABLE OF CONTENTS Project Information Sheet ii Currency Equivalents iv Acronyms and Abbreviations iv Executive Summary v Results-Based Logical Framework vi Implementation Schedule vii I – Strategic Thrust and Objectives 1 1.1 Project Linkages with Country Objectives and Bank Strategy 1 1.2 Rationale for Bank Intervention 2 1.3 Aid Coordination 2 II – Project Description 4 2.1 Description of Components 4 2.2 Technical Solutions Retained and Alternatives Explored 5 2.3 Project Type 6 2.4 Project Cost and Financing Arrangements 6 2.5 Project Areas and Beneficiaries 7 2.6 Participatory Approach for Project Identification, Design and Implementation 8 2.7 Bank Group Experience and Lessons Reflected in Project Design 9 2.8 Key Performance Indicators 10 III – Project Feasibility 11 3.1 Economic and Financial Performance 11 3.2 Environmental Impact, Climate Change, Gender and Social 12 IV – Project Implementation 14 4.1 Implementation Arrangements 14 4.2 Monitoring 17 4.3 Fragility-Governance-Resilience 17 4.4 Sustainability 17 4.5 Risk Management 18 4.6 Knowledge Building 18 4.7 Project Implementation Schedule 19 V - Legal Framework 19 5.1 Legal Instrument 19 5.2 Conditions for Bank Intervention 19 5.3 Compliance with Bank Policies 20 VI - Recommendation 20 Appendix I. Note on the Consideration of Fragility Factors in the Project Appendix II. -
Pdf | 194.53 Kb
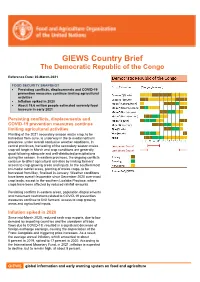
GIEWS Country Brief The Democratic Republic of the Congo Reference Date: 02-March-2021 FOOD SECURITY SNAPSHOT • Persisting conflicts, displacements and COVID-19 prevention measures continue limiting agricultural activities • Inflation spiked in 2020 • About 19.6 million people estimated severely food insecure in early 2021 Persisting conflicts, displacements and COVID-19 prevention measures continue limiting agricultural activities Planting of the 2021 secondary season maize crop, to be harvested from June, is underway in the bi-modal northern provinces, under overall conducive weather conditions. In central provinces, harvesting of the secondary season maize crop will begin in March and crop conditions are generally good following adequate and well-distributed precipitations during the season. In eastern provinces, the ongoing conflicts continue to affect agricultural activities by limiting farmers’ access to crop-growing areas and inputs. In the southernmost uni-modal rainfall areas, planting of maize crops, to be harvested from May, finalized in January. Weather conditions have been overall favourable since December 2020 over most crop lands, except in the southern Lualaba Province, where crops have been affected by reduced rainfall amounts. Persisting conflicts in eastern areas, population displacements and movement restrictions related to COVID-19 prevention measures continue to limit farmers’ access to crop growing areas and agricultural inputs. Inflation spiked in 2020 Since mid-March 2020, reduced cash crop exports, due to low demand by importing countries and the slowdown of trade flows due to COVID-19, resulted in a significant decrease of foreign exchange earnings, causing the depreciation of the Franc Congolais and triggering price increases. As a result, the average annual inflation, which amounted to about 5 percent in 2019, spiked to 17 percent in 2020. -

January 2019.Pdf
DRC Humanitarian Situation Report Photo: UNICEF DRC Tremeau January 2019 SITUATION IN NUMBERS Highlights 1,260,000*Internally Displaced Persons • UNICEF’s response to the North Kivu and Ituri Ebola (IDPs) (HPR 2019) * Estimate for 2019 outbreak can be found on a biweekly basis in the Ebola specific situation reports: 7,500,000 children in need of https://www.unicef.org/appeals/drc_sitreps.html humanitarian assistance (OCHA, HRP 2019) • Kasai and Kwango: hundreds of Congolese nationals continue to return to DRC from Angola on a daily basis. 1,400,000 children are suffering from Severe Acute malnutrition (DRC Nutrition • Voluntary surrender of more than 500 militia members in Cluster, January 2019) Kasai and Kasai provinces, among those 60 children, after the announcement of the final presidential election results. 3,451 cases of cholera reported in January 2019 (Ministry of Health) • Cholera has been declared as epidemic by the Ministry of Health in Haut Katanga province (944 cases; 26 deaths in 6,839 suspect cases of measles reported in January 2019). January (Ministry of Health) UNICEF Appeal 2019 UNICEF’s Response with Partners US$ 326 Million 1% of required funds available UNICEF Sector/Cluster 2019 DRC HAC UNICEF Total Cluster Total FUNDING STATUS Target Results* Target Results* Funds Carry- Nutrition: # of children with Received Over SAM admitted for therapeutic 911,907 120** 986,708 120** $1.2M $43.8M care Health: # of children in 0% humanitarian situations 1,028,959 623,582 14% vaccinated against measles WASH: # of natural disaster -

Humanitarian Situation Report
DRC Humanitarian Situation Report Photo: UNICEF DRC Naftalin April 2019 SITUATION IN NUMBERS Highlights 1,260,000*Internally Displaced Persons (IDPs) (HPR 2019) * Estimate for 2019 • As part of World Vaccination month, 4,244 children (6months- 14years) were vaccinated against measles through the RRMP 7,500,000 children in need of humanitarian mechanism assistance (OCHA, HRP 2019) 1,400,000 children are suffering from Severe • During the month of April, 46,275 persons were provided with Acute malnutrition (DRC Nutrition Cluster, January essential household items, and shelter materials 2019) • Ebola outbreak: as of 14 April 2019, 1,264 total cases of Ebola, 9,606 cases of cholera reported since January 1,198 confirmed cases and 748 deaths linked to Ebola have been 2019 (Ministry of Health) recorded in the provinces of North Kivu and Ituri. 76,107 suspect cases of measles reported since January (Ministry of Health) UNICEF Appeal 2019 US$ 326 Million UNICEF’s Response with Partners 22% of required funds available UNICEF Sector/Cluster 2019 DRC HAC FUNDING STATUS* UNICEF Total Cluster Total Funds received Target Results* Target Results* current year: $27.7M Nutrition: # of children with SAM 911,907 15,573 986,708 15,573 Carry- admitted for therapeutic care forward Health: # of children in amount humanitarian situations 1,028,959 628,896 $43.8M vaccinated against measles WASH: # of natural disaster and 2019 funding conflict-affected people with 1,277,848 307,273 2,232,120 466,231 requirements: access to water, hygiene and sanitation basic services -

USAID Integrated Health Program
USAID INT EGRATED HEALTH PROGRAM Fiscal Year 2019 Quarterly Report 2 (January 1 through March 31, 2019) Submitted May 15, 2019 Approved July 29, 2019 DISCLAIMER: This report is made possible by the support of the American People through the United States Agency for International Development (USAID). The authors’ views expressed in this publication do not necessarily reflect the views of USAID or the United States Government. Recommended Citation: USAID Integrated Health Program. “USAID Integrated Health Program: Fiscal Year 2019 Quarterly Report 2.” Prepared by Abt Associates, Rockville, Maryland, May 15, 2019. Submitted to: Richard Matendo, Contracting Officer’s Representative, Maternal and Child Health Program Specialist, Health Office, USAID/Democratic Republic of the Congo (DRC), (+243 81 555 4514), Kinshasa, DRC. Cover Photo: Credit: Jason Coetzee, Matchboxology for USAID Integrated Health Program (IHP) During a community discussion to elicit inputs for USAID IHP’s human- centered design approach, a young mother from Kasaï-Oriental shares the daily challenges of keeping her children healthy in the context of many other daily household stresses. Abt Associates Inc. 1 6130 Executive Boulevard 1 Rockville, Maryland 20814 1 T. 301.347.5000 1 www.abtassociates.com With: International Rescue Committee (IRC) Pathfinder International BlueSquare Training Resources Group (TRG) Mobile Accord/Geopoll i+Solutions Viamo Matchboxology USAID INTEGRATED HEALTH PROGRAM Fiscal Year 2019 Quarterly Report 2 (January 1 through March 31, 2019) Contract No.: 72066018C00001 DISCLAIMER: This report is made possible by the support of the American People through the United States Agency for International Development (USAID). The authors’ views expressed in this publication do not necessarily reflect the views of USAID or the United States Government. -

Where Does State Capacity Come From? Conjectures from DRC’S New Provinces
Researching livelihoods and services affected by conflict Where does state capacity come from? Conjectures from DRC’s new provinces Working paper 65 Alma Alicia Bezares Calderón and Pierre Englebert February 2019 Written by Alma Alicia Bezares Calderón Pierre Englebert SLRC publications present information, analysis and key policy recommendations on issues relating to livelihoods, basic services and social protection in conflict affected situations. This and other SLRC publications are available from www.securelivelihoods.org. Funded by UK aid from the UK Government, Irish Aid and the EC. Disclaimer: The views presented in this publication are those of the author(s) and do not necessarily reflect the UK Government’s official policies or represent the views of Irish Aid, the EC, SLRC or our partners. ©SLRC 2019. Readers are encouraged to quote or reproduce material from SLRC for their own publications. As copyright holder SLRC requests due acknowledgement. Secure Livelihoods Research Consortium Overseas Development Institute (ODI) 203 Blackfriars Road London SE1 8NJ United Kingdom T +44 (0)20 3817 0031 F +44 (0)20 7922 0399 E [email protected] www.securelivelihoods.org @SLRCtweet Cover photo: New road in Loudima–Dolisie, DRC. jbdodane/Flickr. B About us The Secure Livelihoods Research Consortium (SLRC) is a global research programme exploring basic services, and social protection in fragile and conflict-affected situations. Funded by UK Aid from the UK Government (DFID), with complementary funding from Irish Aid and the European Commission (EC), SLRC was established in 2011 with the aim of strengthening the evidence base and informing policy and practice around livelihoods and services in conflict. -

Social Impacts of Artisanal Cobalt Mining in Katanga, Democratic Republic of Congo
Social impacts of artisanal cobalt mining in Katanga, Democratic Republic of Congo Freiburg, November, 2011 Authors: Öko-Institut e.V. Freiburg Head Office Nicolas Tsurukawa P.O. Box 17 71 79017 Freiburg, Germany Street Address Siddharth Prakash Merzhauser Str. 173 79100 Freiburg Andreas Manhart Phone +49 (0) 761 – 4 52 95-0 Fax +49 (0) 761 – 4 52 95-288 Darmstadt Office Rheinstr. 95 64295 Darmstadt, Germany Phone +49 (0) 6151 – 81 91-0 Fax +49 (0) 6151 – 81 91-133 Berlin Office Schicklerstr. 5-7 10179 Berlin, Germany Phone +49 (0) 30 – 40 50 85-0 Fax +49 (0) 30 – 40 50 85-388 Social impacts of artisanal cobalt mining in Katanga, Democratic Republic of Congo Table of contents List of tables V List of figures V Acknowledgements VIII List of acronyms and abbreviations VIII Executive summary 1 1 Introduction 5 2 Background information 6 2.1 The global cobalt market 6 2.1.1 Demand 6 2.1.2 Production 6 2.1.3 Reserves 8 2.1.4 Prices and market trends 9 2.2 The Congolese context 10 2.2.1 Geology and geography of Cobalt in the Copperbelt 10 2.2.2 History of mining activities in Katanga 14 3 Methodological approach and objectives 17 4 Scope of the study 18 4.1 The cobalt supply-chains 18 4.2 Current stakeholders 19 4.2.1 Artisanal miners 19 4.2.2 State-owned companies 21 4.2.3 Private mining companies 22 4.2.4 Traders 23 4.2.5 The State 24 4.2.6 Assaying companies 26 4.2.7 Local Communities 26 III Social impacts of artisanal cobalt mining in Katanga, Democratic Republic of Congo 5 Impact on workers 27 5.1 Safe and healthy working conditions 27 -

General Assembly Distr.: General 2 January 2020
United Nations A/74/617 General Assembly Distr.: General 2 January 2020 Original: English Seventy-fourth session Agenda item 153 Financing of the United Nations Organization Stabilization Mission in the Democratic Republic of the Congo Budget performance of the United Nations Organization Stabilization Mission in the Democratic Republic of the Congo for the period from 1 July 2018 to 30 June 2019 Report of the Secretary-General Contents Page I. Introduction ................................................................... 5 II. Mandate performance ........................................................... 6 A. Overall ................................................................... 6 B. Budget implementation ...................................................... 6 C. Mission support initiatives ................................................... 11 D. Regional mission cooperation ................................................ 13 E. Partnerships and country team coordination ..................................... 13 F. Results-based budgeting frameworks .......................................... 13 III. Resource performance ........................................................... 56 A. Financial resources ......................................................... 56 B. Summary information on redeployments across groups ........................... 57 C. Monthly expenditure pattern ................................................. 57 D. Other revenue and adjustments ............................................... 58 E. Expenditure -

Democratic Republic of the Congo
OPERATIONAL UPDATE Democratic Republic of the Congo 1 – 31 January 2020 In January, 46 new Burundian From 10 to 16 January, UNHCR On 13 January in Rome (Italy), the asylum-seeker households (121 biometrically registered 807 South Sudan Government and persons) were admitted in the newly arrived Central African opposition movements committed to Kavimvira Transit Center in South refugees (249 households) in a “Cessation of Hostilities Kivu Province. With all reception Gboko, Bosobolo Territory, Nord Agreement.” structures being saturated, new Ubangi Province. arrivals were however forced to wait outside. Refugees Burundian refugees Total in DRC Women Men 47,496 24,451 23,045 As of 31 January 2020 ■ An unaccompanied Burundian refugee child living in Lusenda camp, South Kivu Province, was voluntarily repatriated and reunified with his biological grandparents in Burundi, following UNHCR and ICRC’s collaboration. ■ UNHCR, in coordination with CNR, IOM, AIRD and AIDES, prepared for the resettlement of nine Burundian refugees to Canada. The refugees travelled to Kinshasa, capital of the DRC, for medical screenings and to initiate their visa process. Where possible, resettlement is one of the durable solutions for vulnerable refugees and is dependent on the availability of resettlement places. ■ In January, 46 new Burundian asylum-seeker households (121 persons) were admitted in the Kavimvira Transit Center (TC). With all reception structures being saturated, new arrivals were forced to wait outside the TC. Due to road conditions, the transfer of asylum-seekers and refugees to Mulongwe settlement was delayed. To date, 2,389 persons (862 households) are accommodated in Sange Assembly Point, Kavimvira TC, and Mongemonge TC, although the total capacity is 2,100.