Successful Surgical Coding and Compliance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Adverse Effects of Mouth Breathing
AGD - Academy of General Denstry hp://www.agd.org/publicaons/arcles/?ArtID=6850 Mouth breathing: Adverse effects on facial growth, health, Contact Us academics, and behavior Send to a Friend By Yosh Jefferson, DMD, MAGD Send to Printer Featured in General Dentistry , January/February 2010 Pg. 18-25 Close Window Posted on Friday, January 08, 2010 The vast majority of health care professionals are unaware of the negative impact of upper airway obstruction (mouth breathing) on normal facial growth and physiologic health. Children whose mouth breathing is untreated may develop long, narrow faces, narrow mouths, high palatal vaults, dental malocclusion, gummy smiles, and many other unattractive facial features, such as skeletal Class II or Class III facial profiles. These children do not sleep well at night due to obstructed airways; this lack of sleep can adversely affect their growth and academic performance. Many of these children are misdiagnosed with attention deficit disorder (ADD) and hyperactivity. It is important for the entire health care community (including general and pediatric dentists) to screen and diagnose for mouth breathing in adults and in children as young as 5 years of age. If mouth breathing is treated early, its negative effect on facial and dental development and the medical and social problems associated with it can be reduced or averted. Received: February 11, 2009 Accepted: May 5, 2009 The importance of facial appearances in contemporary society is undeniable. Many studies have shown that individuals with attractive facial features are more readily accepted than those with unattractive facial features, providing them with significant advantages. 1-6 However, many health care professionals (as well as the public) feel that individual facial features are the result of genetics and therefore cannot be altered or changed—in other words, the genotype ultimately controls the phenotype. -

Association Between Oral Habits, Mouth Breathing And
Association between oral habits, mouth breathing E.G. Paolantonio, N. Ludovici, and malocclusion in Italian S. Saccomanno, G. La Torre*, C. Grippaudo preschoolers Dental and Maxillofacial Institute, Head and Neck Department, Fondazione Policlinico Gemelli IRCCS, Catholic University of Sacred Heart, Rome, Italy *Department of Public Health and Infectious Diseases, Sapienza University of Rome, Italy e-mail: [email protected] DOI 10.23804/ejpd.2019.20.03.07 Abstract Introduction Etiopathogenesis of malocclusion involves not only genetic Aim This cross-sectional study was carried out to evaluate but also environmental factors, since craniofacial development the prevalence of malocclusion and associated factors in is stimulated by functional activities such as breathing, preschoolers with the aim of assessing the existence of an chewing, sucking and swallowing [Salone et al., 2013]. association between bad habits and mouth breathing with Non-nutritive sucking habits and mouth breathing are the the most severe malocclusions. most significant environmental risk factors for malocclusion Materials and methods A sample of 1616 children aged [Grippaudo et al., 2016; Gòis et al., 2008; Primoži et al., 2013], 3–6 years was visited by applying the Baby ROMA index, an as they can interfere with occlusion and normal craniofacial orthodontic treatment need index for preschool age. The development. Infants have an inherent, biological drive following were searched: the prevalence of malocclusion, for sucking, that can be satisfied through nutritive sucking, the association of bad habits and mouth breathing with including breast- and bottle-feeding, or through non-nutritive malocclusion, how often are found in association and how sucking on objects such as digits, pacifiers, or toys that may this association is statistically significant. -

Orofacial Myology Is a Specialized Professional Discipline That Evaluates and Treats a Variety Of
What is Orofacial Myology? Orofacial myology is a specialized professional discipline that evaluates and treats a variety of oral and facial (orofacial) muscles, (myo-) postural and functional disorders and oral habits that may disrupt normal dental development and also create cosmetic problems. The principles involved with the evaluation and treatment of orofacial Myofunctional disorders are based upon dental science tenets; however, orofacial Myofunctional therapy is not dental treatment. Myofunctional therapy can be basically described as correcting an oro-facial muscular unbalance, including correction of the position of the tongue at rest and during swallowing. Specific treatments involve establishing and stabilizing normal rest position of the tongue and lips, eliminating deviate (abnormal) oral habits and correcting swallowing patterns when tongue thrusting is involved. Improvements in appearance are observed during and following therapy. What are Myofunctional disorders and how are they corrected? An oral Myofunctional disorder includes a variety of oral habits, postures and functional activities that may open the normal dental bite or may lead to deformation of the dental arches. • Thumb and finger sucking • an open-mouth posture with lips apart • a forward rest posture of the tongue • Tongue thrusting during speaking and swallowing Above mentioned oral habits characterize Myofunctional disorders. Such disorders can lead to a disruption of normal dental development in both children and adults. The consequence of postural and functional variations involving the lips and tongue are associated with dental malocclusion, cosmetic problems, and deformities in the growth of the dental arches. How Prevalent Are Orofacial Myofunctional Disorders (OMD)? Research examining various populations found 38% have orofacial Myofunctional disorders and, as mentioned above, an incidence of 81% has been found in children exhibiting speech/articulation problems. -

Guidelines Proposal for Clinical Recognition of Mouth Breathing Children
original article Guidelines proposal for clinical recognition of mouth breathing children Maria Christina Thomé Pacheco1, Camila Ferreira Casagrande2, Lícia Pacheco Teixeira3, Nathalia Silveira Finck4, Maria Teresa Martins de Araújo5 DOI: http://dx.doi.org/10.1590/2176-9451.20.4.039-044.oar Introduction: Mouth breathing (MB) is an etiological factor for sleep-disordered breathing (SDB) during childhood. The habit of breathing through the mouth may be perpetuated even after airway clearance. Both habit and obstruction may cause facial muscle imbalance and craniofacial changes. Objective: The aim of this paper is to propose and test guidelines for clinical recognition of MB and some predisposing factors for SDB in children. Methods: Semi-structured interviews were conducted with 110 orthodontists regarding their procedures for clinical evaluation of MB and their knowledge about SDB during childhood. Thereafter, based on their answers, guidelines were developed and tested in 687 children aged between 6 and 12 years old and attending elementary schools. Results: There was no standardization for clinical recognition of MB among orthodontists. The most common procedures performed were inefficient to rec- ognize differences between MB by habit or obstruction. Conclusions: The guidelines proposed herein facilitate clinical recognition of MB, help clinicians to differentiate between habit and obstruction, suggest the most appropriate treatment for each case, and avoid maintenance of mouth breathing patterns during adulthood. Keywords: Mouth breathing. Airway obstruction. Craniofacial abnormalities. Introdução: a respiração bucal (RB) é um fator etiológico para os distúrbios respiratórios do sono (DRS) na infância. O hábito de respirar pela boca pode ser perpetuado mesmo depois da desobstrução das vias aéreas. -

Assessment of Orofacial Myofunctional Profiles of Undergraduate Students in the United States
University of Mississippi eGrove Honors College (Sally McDonnell Barksdale Honors Theses Honors College) Spring 5-9-2020 Assessment of Orofacial Myofunctional Profiles of Undergraduate Students in the United States Rachel Yockey Follow this and additional works at: https://egrove.olemiss.edu/hon_thesis Part of the Communication Sciences and Disorders Commons Recommended Citation Yockey, Rachel, "Assessment of Orofacial Myofunctional Profiles of Undergraduate Students in the United States" (2020). Honors Theses. 1406. https://egrove.olemiss.edu/hon_thesis/1406 This Undergraduate Thesis is brought to you for free and open access by the Honors College (Sally McDonnell Barksdale Honors College) at eGrove. It has been accepted for inclusion in Honors Theses by an authorized administrator of eGrove. For more information, please contact [email protected]. ASSESSMENT OF OROFACIAL MYOFUNCTIONAL PROFILES OF UNDERGRADUATE STUDENTS IN THE UNITED STATES by Rachel A. Yockey A thesis submitted to the faculty of The University of Mississippi in partial fulfillment of the requirements of the Sally McDonnell Barksdale Honors College. Oxford May 2020 Approved by _________________________________ Advisor: Dr. Myriam Kornisch _________________________________ Reader: Dr. Toshikazu Ikuta _________________________________ Reader: Dr. Hyejin Park 2 © 2020 Rachel A. Yockey ALL RIGHTS RESERVED 3 ACKNOWLEDGEMENTS First, I would like to express my deepest gratitude to my advisor, Dr. Myriam Kornisch, for her continuous support throughout this process. It has been an honor to work with you and I could not have done it without your guidance. Thank you for always believing in me. To my readers, Dr. Toshikazu Ikuta and Dr. Hyejin Park, I want to thank you for your valued input and time. -
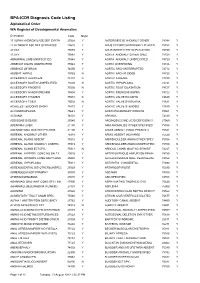
BPA-ICD9 Diagnosis Code Listing Alphabetical Order WA Register of Developmental Anomalies
BPA-ICD9 Diagnosis Code Listing Alphabetical Order WA Register of Developmental Anomalies Description Code Major 17 ALPHA HYDROXYLASE DEF SYNTH25524 Y ANTERIOR EYE ANOMALY OTHER74348 Y 21 HYDROXYLASE DEF SYNTHESIS25520 Y ANUS ECTOPIC/ANTERIORLY PLACED75153 Y 47,XXX 75885 Y ANUS/INTEST/CYST DUPLICATION75150 Y 47,XYY 75884 Y AORTA ANOMALY OTHER SPEC74728 Y ABNORMAL LIMB UNSPECIFIED75548 Y AORTA ANOMALY UNSPECIFIED74729 Y ABSENCE DIGITS UNSPECIFIED75544 Y AORTA OVERRIDING 74726 Y ABSENCE OF BRAIN 74000 Y AORTIC ARCH INTERRUPTED 74712 Y ABSENT NIPPLE 75763 N AORTIC ARCH R SIDED 74723 Y ACCESSORY AURICLE/S 74410 N AORTIC ATRESIA 74720 Y ACCESSORY DIGIT/S UNSPECIFIED75509 N AORTIC HYPOPLASIA 74721 Y ACCESSORY FINGER/S 75500 N AORTIC ROOT DILATATION 74727 Y ACCESSORY HAND/FOREARM 75504 Y AORTIC STENOSIS SUPRA 74722 Y ACCESSORY THUMB/S 75501 N AORTIC VALVE BICUSPID 74640 Y ACCESSORY TOE/S 75502 N AORTIC VALVE DYSPLASIA 74631 Y ACHILLES TENDON/S SHORT 75472 Y AORTIC VALVE STENOSIS 74630 Y ACHONDROPLASIA 75643 Y AORTOPULMONARY WINDOW 74501 Y ACRANIA 74001 Y APHAKIA 74330 Y ADDISONS DISEASE 25540 Y ARGINOSUCCINIC ACID DEFICIENCY27060 Y ADENOMA LIVER 21150 Y ARM ANOMALIES OTHER SPECIFIED75556 Y ADENOMYOMA GASTRIC PYLORIS21100 Y ARM/S ABSENT (HAND PRESENT)75521 Y ADRENAL ANOMALY OTHER 75918 Y ARM/S ABSENT (NO HAND) 75520 Y ADRENAL GLAND ABSENT 75910 Y ARM/SHOULDER ANOM OTHER SPEC75558 Y ADRENAL GLAND ANOMALY UNSPEC75919 Y ARM/SHOULDER ANOM UNSPECIFIED75559 N ADRENAL GLAND ECTOPIC 75913 N ARNOLD CHIARI MALF NO SPIN BIF74227 Y ADRENAL HYPERPL CONG NO -

Common Icd-10 Dental Codes
COMMON ICD-10 DENTAL CODES SERVICE PROVIDERS SHOULD BE AWARE THAT AN ICD-10 CODE IS A DIAGNOSTIC CODE. i.e. A CODE GIVING THE REASON FOR A PROCEDURE; SO THERE MIGHT BE MORE THAN ONE ICD-10 CODE FOR A PARTICULAR PROCEDURE CODE AND THE SERVICE PROVIDER NEEDS TO SELECT WHICHEVER IS THE MOST APPROPRIATE. ICD10 Code ICD-10 DESCRIPTOR FROM WHO (complete) OWN REFERENCE / INTERPRETATION/ CIRCUM- STANCES IN WHICH THESE ICD-10 CODES MAY BE USED TIP:If you are viewing this electronically, in order to locate any word in the document, click CONTROL-F and type in word you are looking for. K00 Disorders of tooth development and eruption Not a valid code. Heading only. K00.0 Anodontia Congenitally missing teeth - complete or partial K00.1 Supernumerary teeth Mesiodens K00.2 Abnormalities of tooth size and form Macr/micro-dontia, dens in dente, cocrescence,fusion, gemination, peg K00.3 Mottled teeth Fluorosis K00.4 Disturbances in tooth formation Enamel hypoplasia, dilaceration, Turner K00.5 Hereditary disturbances in tooth structure, not elsewhere classified Amylo/dentino-genisis imperfecta K00.6 Disturbances in tooth eruption Natal/neonatal teeth, retained deciduous tooth, premature, late K00.7 Teething syndrome Teething K00.8 Other disorders of tooth development Colour changes due to blood incompatability, biliary, porphyria, tetyracycline K00.9 Disorders of tooth development, unspecified K01 Embedded and impacted teeth Not a valid code. Heading only. K01.0 Embedded teeth Distinguish from impacted tooth K01.1 Impacted teeth Impacted tooth (in contact with another tooth) K02 Dental caries Not a valid code. Heading only. -

The SLP's Role in Orofacial Myofunctional Disorders
NJSHA Private What is an Orofacial Practice Committee Myofunctional Disorder? (OMD) The SLP’s Role in Orofacial Myofunctional According to the American Speech-Language- Disorders Hearing Association (ASHA), OMDs are patterns involving oral and orofacial musculature that interfere with normal growth, development, or function of SLPS CAN ASSIST WITH OMDS References orofacial structures, or call attention to themselves (Mason, n.d.A). OMDs can be found in children, American Speech-Language-Hearing Association. (n.d.). Orofacial Myofunctional Disorders. (Practice Portal). Retrieved adolescents and adults. OMDs can co-occur with a 1/15/20 from https://www.asha.org/Practice-Portal/Clinical- variety of speech and swallowing disorders. Topics/Orofacial-Myofunctional-Disorders/. Signs and symptoms include but are not limited to: American Speech-Language-Hearing Association. (2016a). • Articulation problems Code of ethics [Ethics]. Available from: • Dental abnormalities https://www.asha.org/Code-of-Ethics/ • Lip-tie American Speech-Language-Hearing Association. (2016b). • Mouth breathing Scope of practice in speech-language pathology [Scope of • Open mouth posture Practice]. Available from https://www.asha.org/policy/sp2016- • Picky eating habits 00343/. • Problems with chewing and swallowing Master reference list IAOM: • Sleep issues • Teeth grinding http://oralmotorinstitute.org/resources/Orofacial- • Thumb sucking Myofunctional-Disorders-RefList.pdf • Tongue thrusting • Tongue-tie (ankyloglossia) New Jersey Speech-Language-Hearing Association Causes of OMDs • Airway obstructions (deviated septum, large 174 Nassau Street, Suite 337 adenoids) Princeton, NJ 08542 • Craniofacial abnormalities • Improper use of pacifiers (past 12 months) and sippy cups 888-906-5742 • fax 888-729-3489 • Neurological deficits • Oral habits such as thumb sucking [email protected] • www.njsha.org • Structural anomalies What is the SLP’s role in OMD? Assessment and treatment of OMDs are within the SLP’s scope of practice according to ASHA and New Jersey state licensure. -
AOMT-Brochure.Pdf
Orofacial Myofunctional Therapy is an interdisciplinary practice that works with the muscles of the lips, tongue, cheeks and face and their related functions (such as breathing, sucking, chewing, swallowing, and some aspects of speech). It acts in the prevention, evaluation, diagnosis and treatment of people who may have these functions compromised or altered. It can also act in improving facial aesthetics. In this area, the Specialist in Orofacial Myofunctional Therapy can work in partnership with other professionals such as dentists, doctors, physical therapists, occupational therapists, nutritionists, nurses and psychologists. As an emerging field, questions are quite common when we talk about Orofacial Myofunctional Therapy. Below are some answers of frequently asked questions. ON THE FOLLOWING PAGES, WE HAVE COMPILED THE MOST IMPORTANT QUESTIONS AND ANSWERS THAT PEOPLE ASK ABOUT OROFACIAL MYOFUNCTIONAL THERAPY > WHAT IS OROFACIAL MYOFUNCTIONAL THERAPY (OMT)? Orofacial Myofunctional Therapy is neuro- logical re-education exercises to assist the normalization of the developing, or devel- oped, craniofacial structures and function. It is related to the study, research, preven- tion, evaluation, diagnosis and treatment of functional and structural alterations in the region of the mouth (oro), face (facial) and regions of the neck (oropharyngeal area). WHAT IS THE LINK BETWEEN FEEDING AND WHAT ARE THE MAIN PROBLEMS RELATED SPEECH? TO OROFACIAL MYOFUNCTIONAL DISOR- Feeding a child stimulates the orofacial DERS (OMDS)? muscles and this promotes the growth of The main problems related to OMDs are the face. In the same way, proper suction alterations in breathing, sucking, chewing, and chewing prevents dental alterations swallowing and speech, as well the position and difficulties when structures such as the of the lips, tongue (including what is known lips and tongue are moving. -
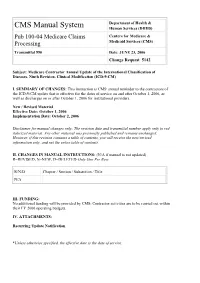
Pub 100-04 Medicare Claims Processing
Department of Health & CMS Manual System Human Services (DHHS) Pub 100-04 Medicare Claims Centers for Medicare & Processing Medicaid Services (CMS) Transmittal 990 Date: JUNE 23, 2006 Change Request 5142 Subject: Medicare Contractor Annual Update of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) I. SUMMARY OF CHANGES: This instruction is CMS' annual reminder to the contractors of the ICD-9-CM update that is effective for the dates of service on and after October 1, 2006, as well as discharges on or after October 1, 2006 for institutional providers. New / Revised Material Effective Date: October 1, 2006 Implementation Date: October 2, 2006 Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents. II. CHANGES IN MANUAL INSTRUCTIONS: (N/A if manual is not updated) R=REVISED, N=NEW, D=DELETED-Only One Per Row. R/N/D Chapter / Section / Subsection / Title N/A III. FUNDING: No additional funding will be provided by CMS; Contractor activities are to be carried out within their FY 2006 operating budgets. IV. ATTACHMENTS: Recurring Update Notification *Unless otherwise specified, the effective date is the date of service. Attachment – Recurring Update Notification Pub. 100-04 Transmittal: 990 Date: June 23, 2006 Change Request 5142 SUBJECT: Medicare Contractor Annual Update of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) I. -

Association Between Oral Habits, Mouth Breathing and Malocclusion
Association between oral habits, mouth breathing E.G. Paolantonio, N. Ludovici, and malocclusion in Italian S. Saccomanno, G. La Torre*, C. Grippaudo preschoolers Dental and Maxillofacial Institute, Head and Neck Department, Fondazione Policlinico Gemelli IRCCS, Catholic University of Sacred Heart, Rome, Italy *Department of Public Health and Infectious Diseases, Sapienza University of Rome, Italy e-mail: [email protected] DOI 10.23804/ejpd.2019.20.03.07 Abstract Introduction Etiopathogenesis of malocclusion involves not only genetic Aim This cross-sectional study was carried out to evaluate but also environmental factors, since craniofacial development the prevalence of malocclusion and associated factors in is stimulated by functional activities such as breathing, preschoolers with the aim of assessing the existence of an chewing, sucking and swallowing [Salone et al., 2013]. association between bad habits and mouth breathing with Non-nutritive sucking habits and mouth breathing are the the most severe malocclusions. most significant environmental risk factors for malocclusion Materials and methods A sample of 1616 children aged [Grippaudo et al., 2016; Gòis et al., 2008; Primožič et al., 2013], 3–6 years was visited by applying the Baby ROMA index, an as they can interfere with occlusion and normal craniofacial orthodontic treatment need index for preschool age. The development. Infants have an inherent, biological drive following were searched: the prevalence of malocclusion, for sucking, that can be satisfied through nutritive sucking, the association of bad habits and mouth breathing with including breast- and bottle-feeding, or through non-nutritive malocclusion, how often are found in association and how sucking on objects such as digits, pacifiers, or toys that may this association is statistically significant. -

EUROCAT Syndrome Guide
JRC - Central Registry european surveillance of congenital anomalies EUROCAT Syndrome Guide Definition and Coding of Syndromes Version July 2017 Revised in 2016 by Ingeborg Barisic, approved by the Coding & Classification Committee in 2017: Ester Garne, Diana Wellesley, David Tucker, Jorieke Bergman and Ingeborg Barisic Revised 2008 by Ingeborg Barisic, Helen Dolk and Ester Garne and discussed and approved by the Coding & Classification Committee 2008: Elisa Calzolari, Diana Wellesley, David Tucker, Ingeborg Barisic, Ester Garne The list of syndromes contained in the previous EUROCAT “Guide to the Coding of Eponyms and Syndromes” (Josephine Weatherall, 1979) was revised by Ingeborg Barisic, Helen Dolk, Ester Garne, Claude Stoll and Diana Wellesley at a meeting in London in November 2003. Approved by the members EUROCAT Coding & Classification Committee 2004: Ingeborg Barisic, Elisa Calzolari, Ester Garne, Annukka Ritvanen, Claude Stoll, Diana Wellesley 1 TABLE OF CONTENTS Introduction and Definitions 6 Coding Notes and Explanation of Guide 10 List of conditions to be coded in the syndrome field 13 List of conditions which should not be coded as syndromes 14 Syndromes – monogenic or unknown etiology Aarskog syndrome 18 Acrocephalopolysyndactyly (all types) 19 Alagille syndrome 20 Alport syndrome 21 Angelman syndrome 22 Aniridia-Wilms tumor syndrome, WAGR 23 Apert syndrome 24 Bardet-Biedl syndrome 25 Beckwith-Wiedemann syndrome (EMG syndrome) 26 Blepharophimosis-ptosis syndrome 28 Branchiootorenal syndrome (Melnick-Fraser syndrome) 29 CHARGE