Binding to and Antibacterial Effect of Aztreonam, Temocillin, Gentamicin and Tobramycin on Human Faeces
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Consideration of Antibacterial Medicines As Part Of
Consideration of antibacterial medicines as part of the revisions to 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) Section 6.2 Antibacterials including Access, Watch and Reserve Lists of antibiotics This summary has been prepared by the Health Technologies and Pharmaceuticals (HTP) programme at the WHO Regional Office for Europe. It is intended to communicate changes to the 2019 WHO Model List of Essential Medicines for adults (EML) and Model List of Essential Medicines for children (EMLc) to national counterparts involved in the evidence-based selection of medicines for inclusion in national essential medicines lists (NEMLs), lists of medicines for inclusion in reimbursement programs, and medicine formularies for use in primary, secondary and tertiary care. This document does not replace the full report of the WHO Expert Committee on Selection and Use of Essential Medicines (see The selection and use of essential medicines: report of the WHO Expert Committee on Selection and Use of Essential Medicines, 2019 (including the 21st WHO Model List of Essential Medicines and the 7th WHO Model List of Essential Medicines for Children). Geneva: World Health Organization; 2019 (WHO Technical Report Series, No. 1021). Licence: CC BY-NC-SA 3.0 IGO: https://apps.who.int/iris/bitstream/handle/10665/330668/9789241210300-eng.pdf?ua=1) and Corrigenda (March 2020) – TRS1021 (https://www.who.int/medicines/publications/essentialmedicines/TRS1021_corrigenda_March2020. pdf?ua=1). Executive summary of the report: https://apps.who.int/iris/bitstream/handle/10665/325773/WHO- MVP-EMP-IAU-2019.05-eng.pdf?ua=1. -

Antibiotic Temocillin Be A
P0840 Could the ‘old’ antibiotic temocillin be a ‘new’ treatment for acute bacterial cholangitis? A retrospective study of 156 cases Sylvain Chawki1, Marion Duprilot1, Gary Taieb1, Veronique Leflon1, Marie-Hélène Nicolas-Chanoine1, Bruno Fantin1, Victoire De Lastours*1 1 Hôpital Beaujon, Assistance Publique Hôpitaux de Paris, Clichy, France Background: Acute cholangitis is a potentially severe infection requiring rapid active antimicrobial therapy. Thus, emergence of multidrug resistant strains of Enterobacteriaceae is a rising global public-health issue. To spare carbapenems, alternative therapies are needed. Temocillin is a narrow-spectrum betalactam targeting almost specifically Enterobacteriaceae, including most isolates resistant to third generation cephalosporin (3GC) and some carbapenemase-producers. Temocillin biliary concentrations may reach several times the blood concentrations. We assessed whether temocillin may represent an alternative treatment for bacterial cholangitis. Materials/methods: In this retrospective monocentric study, all patients from November 2015 to December 2017 admitted for acute cholangitis with a positive culture (blood or bile) were included. Demographic characteristics, severity, treatment and outcome of each episode were collected. Susceptibility to antibiotics, including temocillin, was determined phenotypically. Episodes of cholangitis were considered susceptible to temocillin if all pathogens found were temocillin-susceptible. Results: 137 patients (77/137 male; 56%; median age 67 [60-75]) who suffered 156 episodes of bacterial cholangitis were included (19 patients had 2 separate episodes during the study period). The median Charlson score was 4 [2-8]; 66/137 (48%) were immunocompromised, 54/137 (39%) had a history episode of acute cholangitis. 118/156 (75.6%) episodes were healthcare-associated, 28/156 (18%) required intensive care and 12 (7.7%) were fatal. -

Chemistry Classification Pharmacokinetics Clinical Uses And
Available online www.jocpr.com Journal of Chemical and Pharmaceutical Research, 2014, 6(11):28-58 ISSN : 0975-7384 Review Article CODEN(USA) : JCPRC5 Chemistry, classification, pharmacokinetics, clinical uses and analysis of beta lactam antibiotics: A review Mamdouh S. Masoud a, Alaa E. Ali b* and Nessma M. Nasr c aChemistry Department, Faculty of Science, Alexandria University, Alexandria, Egypt bChemistry Department, Faculty of Science, Damanhour University, Damanhour, Egypt cStudents’ Hospital, Alexandria University, Alexandria, Egypt _____________________________________________________________________________________________ ABSTRACT This review attempts to pinpoint the importance of betalactam antibiotics, which encompass penicillins, cephalosporins, cephamycins, carbapenems and monobactams from its chemistry, classification, pharmacokinetics, clinical uses and analysis. β- lactam antibiotics have been used for treatment of bacterial infections. Most antibacterials are chemically semisynthetic modifications of various natural compounds and classified on the basis of chemical /biosynthetic origin into natural, semisynthetic, and synthetic. Also, this classification system is based on biological activity; that antibacterials are divided into two broad groups according to their biological effect on microorganisms, bactericidal agents kill bacteria, and bacteriostatic agents slow down bacterial growth. Keywords: Beta lactam Antibiotics, Classification, Pharmacokinetics, Clinical uses, Analysis. _____________________________________________________________________________________________ -

A Thesis Entitled an Oral Dosage Form of Ceftriaxone Sodium Using Enteric
A Thesis entitled An oral dosage form of ceftriaxone sodium using enteric coated sustained release calcium alginate beads by Darshan Lalwani Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Master of Science Degree in Pharmaceutical Sciences with Industrial Pharmacy Option _________________________________________ Jerry Nesamony, Ph.D., Committee Chair _________________________________________ Sai Hanuman Sagar Boddu, Ph.D, Committee Member _________________________________________ Youssef Sari, Ph.D., Committee Member _________________________________________ Patricia R. Komuniecki, PhD, Dean College of Graduate Studies The University of Toledo May 2015 Copyright 2015, Darshan Narendra Lalwani This document is copyrighted material. Under copyright law, no parts of this document may be reproduced without the expressed permission of the author. An Abstract of An oral dosage form of ceftriaxone sodium using enteric coated sustained release calcium alginate beads by Darshan Lalwani Submitted to the Graduate Faculty as partial fulfillment of the requirements for the Master of Science Degree in Pharmaceutical Sciences with Industrial Pharmacy option The University of Toledo May 2015 Purpose: Ceftriaxone (CTZ) is a broad spectrum semisynthetic, third generation cephalosporin antibiotic. It is an acid labile drug belonging to class III of biopharmaceutical classification system (BCS). It can be solvated quickly but suffers from the drawback of poor oral bioavailability owing to its limited permeability through -
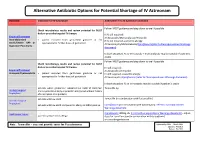
Shortage of Aztreonam Guidance Document.Pdf
Alternative Antibiotic Options for Potential Shortage of IV Aztreonam Guidance Indication for IV Aztreonam Alternative if no IV Aztreonam available Follow IVOST guidance and step down to oral if possible. Check microbiology results and review potential for IVOST daily or prescribe targeted IV therapy If IV still required: Empirical Treatment IV Amoxicillin/Metronidazole/Temocillin Intra-abdominal • patient excluded from gentamicin guidance or not If IV still required + pencillin allergy: sepsis/Severe HAP or appropriate for further doses of gentamicin IV Vancomycin/Metronidazole/Ciprofloxacin(refer to Fluoroquinolones Warnings Aspiration Pneumonia document) In both situations IV co-trimoxazole + metronidazole may be suitable if patient is stable Follow IVOST guidance and step down to oral if possible. Check microbiology results and review potential for IVOST daily or prescribe targeted IV therapy IV still required: Empirical Treatment IV Amoxicillin /Temocillin Urosepsis/Pyelonephritis • patient excluded from gentamicin guidance or not IV still required + pencillin allergy: appropriate for further doses of gentamicin IV Vancomycin /Ciprofloxacin (refer to Fluoroquinolones Warnings document) In both situations IV co-trimoxazole may be suitable if patient is stable patients where gentamicin indicated but eGFR 15-30ml/min Temocillin 1g Urology Surgical and no penicillin allergy or penicillin allergy but without history Prophylaxis of anaphylaxis or angiodema patients with low eGFR Temocillin (in combination with flucloxacillin) Vascular Surgical Prophylaxis patients with low eGFR and penicillin allergy or MRSA positive Ciprofloxacin (in combination with vancomycin): refer to Fluoroquinolones Warnings document Neutropenic Sepsis Ciprofloxacin 400mg tds (refer to Fluoroquinolones Warnings document)– adjust patients with pencillin allergy dose for renal function (in combination with teicoplanin) or consider gentamicin Note: Temocillin – does not provide cover for Pseudomonas Approved by AMG: March 2016 Updated: Feb 2019 Review: Feb 2022 . -

Hap-Vap-Guidelines-2016.Pdf
Clinical Infectious Diseases IDSA GUIDELINE Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society 1,a 2,a 3,4 5 6 7 8 9 Andre C. Kalil, Mark L. Metersky, Michael Klompas, John Muscedere, Daniel A. Sweeney, Lucy B. Palmer, Lena M. Napolitano, Naomi P. O’Grady, Downloaded from https://academic.oup.com/cid/article-abstract/63/5/e61/2237650 by IDSA user on 16 October 2018 John G. Bartlett,10 Jordi Carratalà,11 Ali A. El Solh,12 Santiago Ewig,13 Paul D. Fey,14 Thomas M. File Jr,15 Marcos I. Restrepo,16 Jason A. Roberts,17,18 Grant W. Waterer,19 Peggy Cruse,20 Shandra L. Knight,20 and Jan L. Brozek21 1Department of Internal Medicine, Division of Infectious Diseases, University of Nebraska Medical Center, Omaha; 2Division of Pulmonary and Critical Care Medicine, University of Connecticut School of Medicine, Farmington; 3Brigham and Women’s Hospital and Harvard Medical School, and 4Harvard Pilgrim Health Care Institute, Boston, Massachusetts; 5Department of Medicine, Critical Care Program, Queens University, Kingston, Ontario, Canada; 6Division of Pulmonary, Critical Care and Sleep Medicine, University of California, San Diego; 7Department of Medicine, Division of Pulmonary Critical Care and Sleep Medicine, State University of New York at Stony Brook; 8Department of Surgery, Division of Trauma, Critical Care and Emergency Surgery, University of Michigan, Ann Arbor; 9Department of Critical Care Medicine, National -

2000 Dialysis of Drugs
2000 Dialysis of Drugs PROVIDED AS AN EDUCATIONAL SERVICE BY AMGEN INC. I 2000 DIAL Dialysis of Drugs YSIS OF DRUGS Curtis A. Johnson, PharmD Member, Board of Directors Nephrology Pharmacy Associates Ann Arbor, Michigan and Professor of Pharmacy and Medicine University of Wisconsin-Madison Madison, Wisconsin William D. Simmons, RPh Senior Clinical Pharmacist Department of Pharmacy University of Wisconsin Hospital and Clinics Madison, Wisconsin SEE DISCLAIMER REGARDING USE OF THIS POCKET BOOK DISCLAIMER—These Dialysis of Drugs guidelines are offered as a general summary of information for pharmacists and other medical professionals. Inappropriate administration of drugs may involve serious medical risks to the patient which can only be identified by medical professionals. Depending on the circumstances, the risks can be serious and can include severe injury, including death. These guidelines cannot identify medical risks specific to an individual patient or recommend patient treatment. These guidelines are not to be used as a substitute for professional training. The absence of typographical errors is not guaranteed. Use of these guidelines indicates acknowledgement that neither Nephrology Pharmacy Associates, Inc. nor Amgen Inc. will be responsible for any loss or injury, including death, sustained in connection with or as a result of the use of these guidelines. Readers should consult the complete information available in the package insert for each agent indicated before prescribing medications. Guides such as this one can only draw from information available as of the date of publication. Neither Nephrology Pharmacy Associates, Inc. nor Amgen Inc. is under any obligation to update information contained herein. Future medical advances or product information may affect or change the information provided. -

Temocillin Disodium PRODUCT DATA SHEET Issue Date 01/06/2020
Temocillin Disodium PRODUCT DATA SHEET issue date 01/06/2020 Product Name: Temocillin Disodium Product Number: T130 CAS Number: 61545-06-0 Molecular Formula: C16H18N2Na2O7S2 Molecular Weight: 458.42 Form: Powder Appearance: white or almost white powder Source: semi-synthetic Description: Temocillin Disodium is the salt of Temocillin a semisynthetic, βlactamase resistant carboxypenicillin antimicrobial used as an alternative to carbapenems that is primarily used for Gram-negative bacteria. Mechanism of Action: Like other βlactams, Temocillin Disodium interferes with penicillin binding protein (PBP) activity involved in the final phase of peptidoglycan synthesis. PBB catalyzes the pentaglycine crosslink between alanine and lysine. Without a pentaglycine crosslink, the integrity of the cell wall is compromised which leads to cell lysis and death. Temocillin is resistant to most βlactamases, but resistance is commonly due to cells containing plasmidencoded β lactamases. Spectrum: Temocillin is active against several multi-resistant Gram-negative species including Salmonella typhimurium, E. coli, Haemophilus influenzae and others. In contrast, Gram-positive bacteria, bacteria with altered penicillin- binding proteins, and Pseudomonas aeruginosa are not susceptible to temocillin. Microbiology Applications Temocillin is commonly used in clinical in vitro microbiological antimicrobial susceptibility tests (panels, discs, and MIC strips) against Gram-negative microbial isolates. Medical microbiologists use this information to recommend antibiotic treatment options. Representative MIC ranges include: E. coli 1.00 µg/mL 64.00 µg/mL H. influenzae βlactamase negative: 0.25 0.50 µg/ml H. influenzae βlactamase positive: 0.50 1.00 µg/ml S. aureus >128.00 µg/ml For a list of MIC values, click here. -

Antibiotics Against Multidrug-Resistant Gram-Negative Bacteria
Journal of Clinical Medicine Review An Update on Eight “New” Antibiotics against Multidrug-Resistant Gram-Negative Bacteria Erlangga Yusuf * , Hannelore I. Bax, Nelianne J. Verkaik and Mireille van Westreenen Department of Medical Microbiology and Infectious Diseases, Erasmus University Medical Center, 3015 GD Rotterdam, The Netherlands; [email protected] (H.I.B.); [email protected] (N.J.V.); [email protected] (M.v.W.) * Correspondence: [email protected] Abstract: Infections in the ICU are often caused by Gram-negative bacteria. When these microorgan- isms are resistant to third-generation cephalosporines (due to extended-spectrum (ESBL) or AmpC beta-lactamases) or to carbapenems (for example carbapenem producing Enterobacteriales (CPE)), the treatment options become limited. In the last six years, fortunately, there have been new an- tibiotics approved by the U.S. Food and Drug Administration (FDA) with predominant activities against Gram-negative bacteria. We aimed to review these antibiotics: plazomicin, eravacycline, temocillin, cefiderocol, ceftazidime/avibactam, ceftolozane/tazobactam, meropenem/vaborbactam, and imipenem/relebactam. Temocillin is an antibiotic that was only approved in Belgium and the UK several decades ago. We reviewed the in vitro activities of these new antibiotics, especially against ESBL and CPE microorganisms, potential side effects, and clinical studies in complicated urinary tract infections (cUTI), intra-abdominal infections (cIAI), and hospital-acquired pneumonia/ventilator- associatedpneumonia (HAP/VAP). All of these new antibiotics are active against ESBL, and almost all of them are active against CPE caused by KPC beta-lactamase, but only some of them are active against CPE due to MBL or OXA beta-lactamases. -

Critically Important Antimicrobials for Human Medicine – 5Th Revision. Geneva
WHO Advisory Group on Integrated Surveillance of Antimicrobial Resistance (AGISAR) Critically Important Antimicrobials for Human Medicine 5th Revision 2016 Ranking of medically important antimicrobials for risk management of antimicrobial resistance due to non-human use Critically important antimicrobials for human medicine – 5th rev. ISBN 978-92-4-151222-0 © World Health Organization 2017, Updated in June 2017 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial- ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/ igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. Critically important antimicrobials for human medicine – 5th rev. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO. -

Microguidance (Hospital Adult) When Male and Female Are Stated Within This Policy, It Refers to Sex Assigned at Birth
MicroGuidance (Hospital Adult) When male and female are stated within this policy, it refers to sex assigned at birth Antibiotic ‘rules’ of thumb are broad generalisations which can be used before sensitivity results are available. There are always exceptions & patterns are less predictable now than ever before. Practice points Before you call MICRObiology Rules of ‘thumb’: see note above for advice please have the Sensitivity testing of the causative organism is Gram negative ‘coliforms’ (eg E coli, Klebsiella, Enterobacter, Proteus) & important for deep or invasive infections and/or those following details to hand: Pseudomonas aeruginosa are usually sensitive to gentamicin. Amoxicillin only not responding to treatment. Please send relevant Main complaint & history; current & recent covers 47% of E coli: when you stop gentamicin you might not have good coliform samples – especially blood cultures wherever cover. Check sensitivities possible BEFORE antibiotics are given. antibiotic history Initial assessment & Investigations; radiology, Co-trimoxazole covers about 65% of E coli Extended Spectrum Beta Lactamases (ESBL) are resistant to most penicillins Check to see if the patient has a previous positive samples to determine infection focus ALERT organism like an ESBL, MRSA, CPE etc. (including co-amoxiclav, piperacillin-tazobactam & aztreonam) RP This may influence your initial empiric treatment C , WCC; results & trends Temocillin, pivmecillinam (& meropenem) have cover for ESBLs Renal function; allergy Temocillin & ertapenem do -

Optimisation of Therapy in Gram-Negative Infections
The new antibiotics: useful improvement of our current armamentarium ... but can we pay for them? Paul M. Tulkens, MD, PhD Françoise Van Bambeke, PharmD, PhD Pharmacologie cellulaire et moléculaire Louvain Drug Research Institute, Université catholique de Louvain, Brussels, Belgium http://www.facm.ucl.ac.be Facultad de Medicina Medellin, Colombia, 1 December 2015 1/12/2015 Medellin - Universidad de Antioquia 1 Disclosures and slides availability • Research grants – Theravance, Astellas, Targanta, Cerexa/Forest, AstraZeneca, Bayer, GSK, Trius, Rib-X, Eumedica, Debiopharm – Belgian Science Foundation (F.R.S.-FNRS), Ministry of Health (SPF), Walloon and Brussels Regions, European Union (FP7 programme) • Speaking fees – Bayer, GSK, Sanofi, Johnson & Johnson, OM-Pharma • Decision-making and consultation bodies – European Committee for Antimicrobial Susceptibility Testing [EUCAST] (General Assembly and steering committee (2010-2012)) – European Medicines Agency (external ad-hoc expert) – US National Institutes of Health (grant reviewing) – Drive-AB [Driving reinvestment in R&D and responsible use for antibiotics] (governance) Slides: http://www.facm.ucl.ac.be Lectures 1/12/2015 Medellin - Universidad de Antioquia 2 Belgium 1/12/2015 Medellin - Universidad de Antioquia 3 What do we do? • Teaching of Pharmacology and • improved schedules of aminoglycosides and Pharmacotherapy β-lactams • Post-graduate training on Drug • assessment of novel antibiotics Development • beta-lactams (e.g., ceftaroline…) • Launching of Clinical Pharmacy in Europe