Effect of Ascorbic Acid in the Treatment of Tetanus 197
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Murder by Poison in Scotland During the Nineteenth and Early Twentieth Centuries
Merry, Karen Jane (2010) Murder by poison in Scotland during the nineteenth and early twentieth centuries. PhD thesis. http://theses.gla.ac.uk/2225/ Copyright and moral rights for this thesis are retained by the author A copy can be downloaded for personal non-commercial research or study, without prior permission or charge This thesis cannot be reproduced or quoted extensively from without first obtaining permission in writing from the Author The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the Author When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given Glasgow Theses Service http://theses.gla.ac.uk/ [email protected] Murder by Poison in Scotland During the Nineteenth and Early Twentieth Centuries Karen Jane Merry Submitted for the Degree of Doctor of Philosophy School of Law Department of Forensic Medicine Faculty of Law, Business and Social Science Faculty of Medicine © Karen Jane Merry July 2010 ABSTRACT This thesis examines the history of murder by poison in Scotland during the nineteenth and early twentieth centuries, in the context of the development of the law in relation to the sale and regulation of poisons, and the growth of medical jurisprudence and chemical testing for poisons. The enquiry focuses on six commonly used poisons. Each chapter is followed by a table of cases and appendices on the relative scientific tests and post-mortem appearances. The various difficulties in testing for these poisons in murder and attempted murder cases during the period are discussed and the verdicts reached by juries in poisoning trials considered. -

Signs and Symptoms of Pesticide Poisoning
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Historical Materials from University of Nebraska-Lincoln Extension Extension 1997 EC97-2505 Signs and Symptoms of Pesticide Poisoning Larry D. Schulze University of Nebraska - Lincoln, [email protected] Clyde Ogg University of Nebraska - Lincoln, [email protected] Edward F. Vitzthum University of Nebraska - Lincoln, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/extensionhist Part of the Agriculture Commons, and the Curriculum and Instruction Commons Schulze, Larry D.; Ogg, Clyde; and Vitzthum, Edward F., "EC97-2505 Signs and Symptoms of Pesticide Poisoning" (1997). Historical Materials from University of Nebraska-Lincoln Extension. 1225. https://digitalcommons.unl.edu/extensionhist/1225 This Article is brought to you for free and open access by the Extension at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Historical Materials from University of Nebraska-Lincoln Extension by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. University of Nebraska Cooperative Extension EC97-2505-A Signs and Symptoms of Pesticide Poisoning Larry D. Schulze, Extension Pesticide Coordinator Clyde L. Ogg, Extension Assistant, Pesticide Training Edward F. Vitzthum, Coordinator, Environmental Programs z Manage Your Risk z Signal Words z Read the pesticide Label z Routes of Exposure z Pesticide Toxicity z Recognizing Signs and Symptoms of Poisoning z Recognizing Common pesticide Poisonings { Organophosphate and Carbamate Insecticides { Organochlorine Insecticides { Synthetic Pyrethroid Insecticides { Plant-derived Insecticides { Inorganic Insecticides { Microbial Insecticides { DEET Repellent { Bipyridyl Herbicides { Chlorophenoxy Herbicides { Arsenical Herbicides { Wood Preservatives { Fumigants { Rodenticides { Fungicides z What To Do When Pesticide Poisoning Occurs z References z Pesticide Safety Telephone Numbers Accidental exposure or overexposure to pesticides can have serious implications. -

Strychnine Poisoning
0++- Poison HOTLINE Partnership between UnityPoint Health and University of Iowa Hospitals and Clinics November 2013 Strychnine Poisoning Strychnine is a chemical naturally found in the seeds of the tree Strychnos nux- vomica. It is mainly used as a pesticide to control rats, moles, gophers, and coyotes. Commercial baits are pelleted and often dyed red or green. Strychnine has on rare occasions been found to be mixed with street drugs such as LSD, heroin, and cocaine. Strychnine is a white, odorless, bitter tasting crystalline powder that can be taken by mouth, inhaled or given intravenously. Strychnine is highly toxic and Did you know …… only a small amount is needed to produce severe health effects in people. As little as 30 mg may cause death in an adult. Vaporizing alcohol and “smoking” the vapors (inhaling Strychnine blocks the action of the neurotransmitter glycine which controls how is a more accurate term) is a nerve signals are sent to muscles. Glycine is an inhibitory neurotransmitter and new method for alcohol works like an “off switch” for muscles. When this “off switch” is not working consumption. The alcohol is because it is being blocked by strychnine, muscles throughout the body have poured into a vaporizing severe, painful spasms. While these spasms may look like the patient is having machine or over dry ice and a seizure, it is not a true seizure and there is no post-ictal phase. Repetitive inhaled. The alcohol enters muscle spasms caused by strychnine will lead to fever, muscle break down the lungs where it is rapidly (rhabdomyolysis), severe metabolic acidosis and respiratory failure. -

Dermal Exposure to Strychnine
Journal of Analytical Toxicology, Vol. 25, July/August 2001 [CaseReport Dermal Exposureto Strychnine Richard Greene 1 and Robert MeatheralP,* 1Emergency Department, Grace General Hospital and 2Laboratory Medicine, St. Boniface General Hospital, Winnipeg, Manitoba, Canada Downloaded from https://academic.oup.com/jat/article/25/5/344/778260 by guest on 24 September 2021 t Abstract ] tents into the toilet. She accidently spilled about 1 cupful on the floor, which she wiped up with a cloth soaked in a diluted Javex A non-fatal case of strychnine poisoning through dermal exposure is solution (sodium hypochlorite). Her dermal exposure was limited described. About 24 b after cleaning up a strychnine spill, a 50-year- to her left palm; she washed her hands about 30 rain after old woman presented to the emergency department with classical cleaning up the spill. During the prodromal time period, she signs of strychnine poisoning, consisting of marked pain in the experienced no irritation or dermatitis to the left hand. Except for muscles of her lower limbs, dermal sensitivity, and stiffness in her a tingling sensation in her left hand, she was asymptomatic until jaw. Her treatment was intravenous fluid replacement and about 22:00 h when her arms and legs began to shake, pro- alkalinization in anticipation of potential renal failure due to gressing to spasms. Over the course of the night, the frequency rhabdomyolysis. Her plasma creatine kinase was elevated to 677 and duration of these muscle contractions increased. By U/L with no rise in the heart specific MB fraction. Serum myoglobin morning, the pain was more severe in the muscles of her lower level obtained retrospectively was 195 pg/L. -

Question of the Day Archives: Monday, December 5, 2016 Question: Calcium Oxalate Is a Widespread Toxin Found in Many Species of Plants
Question Of the Day Archives: Monday, December 5, 2016 Question: Calcium oxalate is a widespread toxin found in many species of plants. What is the needle shaped crystal containing calcium oxalate called and what is the compilation of these structures known as? Answer: The needle shaped plant-based crystals containing calcium oxalate are known as raphides. A compilation of raphides forms the structure known as an idioblast. (Lim CS et al. Atlas of select poisonous plants and mushrooms. 2016 Disease-a-Month 62(3):37-66) Friday, December 2, 2016 Question: Which oral chelating agent has been reported to cause transient increases in plasma ALT activity in some patients as well as rare instances of mucocutaneous skin reactions? Answer: Orally administered dimercaptosuccinic acid (DMSA) has been reported to cause transient increases in ALT activity as well as rare instances of mucocutaneous skin reactions. (Bradberry S et al. Use of oral dimercaptosuccinic acid (succimer) in adult patients with inorganic lead poisoning. 2009 Q J Med 102:721-732) Thursday, December 1, 2016 Question: What is Clioquinol and why was it withdrawn from the market during the 1970s? Answer: According to the cited reference, “Between the 1950s and 1970s Clioquinol was used to treat and prevent intestinal parasitic disease [intestinal amebiasis].” “In the early 1970s Clioquinol was withdrawn from the market as an oral agent due to an association with sub-acute myelo-optic neuropathy (SMON) in Japanese patients. SMON is a syndrome that involves sensory and motor disturbances in the lower limbs as well as visual changes that are due to symmetrical demyelination of the lateral and posterior funiculi of the spinal cord, optic nerve, and peripheral nerves. -

Survival After Deliberate Strychnine Self-Poisoning, with Toxicokinetic Data
University of Wollongong Research Online Faculty of Science, Medicine and Health - Papers: part A Faculty of Science, Medicine and Health 2002 Case report: Survival after deliberate strychnine self-poisoning, with toxicokinetic data David Michael Wood Guy’s and St. Thomas’ Hospital Emma Webster Royal Oldham Hospital Daniel Martinez Guy’s and St. Thomas’ Hospital Paul Ivor Dargan Guy’s and St. Thomas’ Hospital Alison L. Jones University of Wollongong, [email protected] Follow this and additional works at: https://ro.uow.edu.au/smhpapers Part of the Medicine and Health Sciences Commons, and the Social and Behavioral Sciences Commons Recommended Citation Wood, David Michael; Webster, Emma; Martinez, Daniel; Dargan, Paul Ivor; and Jones, Alison L., "Case report: Survival after deliberate strychnine self-poisoning, with toxicokinetic data" (2002). Faculty of Science, Medicine and Health - Papers: part A. 1903. https://ro.uow.edu.au/smhpapers/1903 Research Online is the open access institutional repository for the University of Wollongong. For further information contact the UOW Library: [email protected] Case report: Survival after deliberate strychnine self-poisoning, with toxicokinetic data Abstract Introduction Strychnine poisoning is uncommon, and in most severe cases, the patient dies before reaching hospital. The management of strychnine poisoning is well documented, although there are few data on the kinetics of elimination of strychnine after overdose. Case report A 42-year-old man presented shortly after ingestion of an unknown quantity of strychnine powder. After a respiratory arrest, with intensive supportive management requiring admission to an intensive care unit, he survived. Eight serum samples were taken over the first 5 days and analysed subsequently for strychnine concentrations. -
Ingested Lethal Ageni's Strychnine
REVIEW OF CURRENT VERTEBRATE PESTICIDES D. Glen Crabtree Bureau of Sport Fisheries and Wildlife, Wildlife Research Center, B1dg. 45, Denver Federal Center, Denver 25, Colorado. For the purpose of this brief review, EmG>hasis will be placed on development, physical properties, physiological action, experience and limitations of vertebrate pesticides primarily of current opera- tional 1.m;portance in the control of field rodents and predatory animals. INGESTED LETHAL AGENI'S STRYCHNINE (C21H~202) 'Dlis al.kaloid was discovered by Pelletier and Cavento,}/in 1817 as a constituent in the seeds of Strychnos Nux-vomica or Strychnos !gnatii, which were used :for killing dogs, cats and birds in Europe at least as early as J.6ljo • Strychnine (probably the sulfate) appears to have been introduced as a pesticide in the United States about 1847 and became the g/ principal tool of the professional "wolfer" during the years 1800-1885. PHYSICAL PROPERTIES: ~e alkaJ.oid of commerce is a white or greyish white powder prepared from seeds grown in Southern Asia. It is quite stable, almost insoluble in water, but soluble in many organic solvents and to varying degrees in dilute acids With which it forms salts having limited solubility in water. Strychnine and its salts have an exceedingly bitter taste and are not absorbed through the normal intact skin. 327 Both the alkaloid and strychnine sul.fate are widely used today as vertebrate pesticides. In the case of the latter, allowance must be made in preparing l.ethal baits since it contains onl.y 78.04~ strychnine. PHYSIOLOGICAL ACTION: Ingested strychnine is proJJG>tly absorbed, mainly, from the intestinal tract. -
Managing Pesticide Poisoning Risk and Understanding the Signs and Symptoms Clyde L
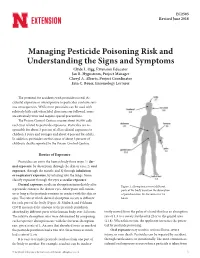
EC2505 Revised June 2018 Managing Pesticide Poisoning Risk and Understanding the Signs and Symptoms Clyde L. Ogg, Extension Educator Jan R. Hygnstrom, Project Manager Cheryl A. Alberts, Project Coordinator Erin C. Bauer, Entomology Lecturer The potential for accidents with pesticides is real. Ac- cidental exposure or overexposure to pesticides can have seri- ous consequences. While most pesticides can be used with relatively little risk when label directions are followed, some are extremely toxic and require special precautions. The Poison Control Centers receive about 90,000 calls each year related to pesticide exposures. Pesticides are re- sponsible for about 3 percent of all accidental exposures to children 5 years and younger and about 4 percent for adults. In addition, pesticides are the cause of about 3 percent of children’s deaths reported to the Poison Control Centers. Routes of Exposure Pesticides can enter the human body three ways: 1) der- mal exposure, by absorption through the skin or eyes; 2) oral exposure, through the mouth; and 3) through inhalation or respiratory exposure, by inhaling into the lungs. Some classify exposure through the eyes as ocular exposure. Dermal exposure results in absorption immediately after Figure 1. Absorption rates of different a pesticide contacts the skin or eyes. Absorption will contin- parts of the body based on the absorption ue as long as the pesticide remains in contact with the skin or of parathion into the forearm over 24 eyes. The rate at which dermal absorption occurs is different hours. for each part of the body (Figure 1). Maiback and Feldman (1974) measured the amount of the pesticide parathion absorbed by different parts of the human body over 24 hours. -

Pick Your Poison
The Chemist Journal of the American Institute of Chemists Pick Your Poison Erika Leah Harmon Pratte, Sabrina Bryant, Cynthia Handley and Margot Hall* Department of Medical Laboratory Science-University of Southern Mississippi | Hattiesburg, MS 39406 (*E-mail: [email protected]) Abstract: During the 16th to the 18th centuries, the royal courts were renowned for their dangers, intrigues and deceptions. There were constant threats to the throne and there are entire libraries dedicated to the lengths a royal family would undergo in order to ensure that their offspring would either inherit the throne or to ensure they themselves would keep the throne. One way that royalty could ensure that their family line stayed in the ruling position was simple … remove the threat. This time in history is filled with tales of this royal having that royal poisoned, this mistress having that wife killed and so forth. The list is endless. Though there were many routes the royals utilized to exterminate their competition, some fairly inventive, this paper will focus on the more mysterious aspect utilized: poisoning. This topic was inspired by certain special ladies of the royal court such as Catherine de’ Medici, the Marquise de Brinvillers and Catherine Deshayes, or as she was later called “La Voisine” (Hooper, 2006). This paper will focus on a select few of the plant derived poisons. Some of these poisons need to be introduced into the body via the skin while others can simply be ingested or inhaled. While there are some poisons that simply irritate the skin this paper focuses on poisons with serious enough side effects to end the life of an enemy. -

Handbook of Common Poisonings in Children. INSTITUTION Food and Drug Administration (DREW), Washington, D.C
O DOCUMENT BESUME ED 144 708 PS 099 577 $ ...,, / 1.- . ,TITLE - Handbook of CommOn Poisonings in Children. INSTITUTION Food and Drug Administration (DREW), Washington, D.C. " fEPORT NO , HEW-FDA-707004 pus DATE /6, ' NOTE -114p. ,.. 1 AyAILABLEFRO!! Superintendent of Documents, U.S. Government Printing ..... Office, Washington, D.C. 20402 (Stock No. 017-C12-0024074, $1.50) . EDRS PRICE NF -$0.83 HC-$6.01. Pins Postage. DESCRtPTORS Accident Prevention;*Children;Emergency'SqUad Personnel; *Governm'ent Publications; icGuidaS; Hospital Pe onnel; Pharmacists;- Physicians;_ *Reference Bo ks IDENTtFIERS, *Poisoning ABSTRACT This handbook for physicians, emergency room. personhel and pharmacists lists- the manufacturer, descriptiOn, / toxiaity, symptoms and findings, treatment, and references.for-73 . / poison substances considered by the Subcommittee on 1Ccidental 1 Poisoning of the American-Academi% of'Pediatrics to be most significant in terms of accidental poisoning of.ehildFen.' (BF) 1 *****************************f**************,************************** * .DOcuments acquirNd by ERIC inclUde many inforMal unpublished *. * materials not available from other-sources. ERIC makes every effort * * to obtain the'best copy available. Nevertheless, items of marginal * * reproducibility are often encountered and this affects the quality * *sof the 'microfiche and hardcopy reproddctions ERIC makes available * via the ERIC Document (reproduction Service (EDRS) .EDRS is not . * * responsible for the quality bf the original document. Reproductions * . *.supplied by EDRS, are the best that can beemade from the 'original. ******************41********r****************************************** U.S. DEPARTtAENT OF HEALTH, EDUCATION, AND WELFARE Public vice/Fo©d and Drug Administration 5600Fi Rockville, Maryland 20857 HEW (FDA) 16-7004 , , , Handbook of # ,. Common Poisonings in Children 1976,. 0 r FDA 4,1 . For we by the 044rorinlyndsrot el Deoumenes. -

Strychnos Nux- Vomica, a Tree Native to Tropical Asia and North Australia, and in Strychnosignatii and Strychnos Tiente, Trees Native to South Asia
STRYCHNINE Department of Clinical Toxicology Loghman Poison Center Mitra Rahimi MD Strychnine alkaloid can be found naturally in Strychnos nux- vomica, a tree native to tropical Asia and North Australia, and in Strychnosignatii and Strychnos tiente, trees native to South Asia. HISTORY Strychnine was first introduced as a rodenticide in 1540, and in subsequent centuries was used medically as a cardiac, respiratory, and digestive stimulant," as an analeptic," and as an antidote to barbiturate and opioid overdoses." Nonketotic hyperglycemia. sleep apnea, "and snake bites" were also once considered indications for strychnine use. It is an odorless and colorless crystalline powder that has a bitter taste when dissolved in water. In addition to the naturally occurring alkaloidal form, strychnine is available from commercial sources in its salt form, usually as nitrate, sulfate, or phosphate. Currently, strychnine is used mainly as a pesticide and rodenticide (for moles, gophers, and pigeons)," and a research tool for the study of glycine receptors, Most commercially available strychnine-containing products contain about 0.25% to 0.5% strychnine by weight." Strychnine poisoning has resulted from deliberate exposure with suicidal and homicidal intent, from unintentional poisoning by a Chinese herbal medicine (Maqianzi)," a Cambodian traditional remedy (slang nut)and adulteration of street drugs. The bitter taste and lethality of strychnine allow it to be substituted for heroin" and cocaine,There are also reports of strychnine poisoning from adulterated amphetamines," ecstasy ( [MDMAJ),Spanish fly," and from the ingestion of gopher bait. TOXICOKINETICS Standard references list the lethal dose of strychnine as approximately . However, mortality resulting from doses as low as 5 to 10 mg and, alternatively, survival following ingestions of 1 to 15 g of strychnine are reported Protein binding is minimal and strychnine is rapidly distributed to peripheral tissues' with a large volume of distribution (13 L/kg). -

Poisonous and Injurious Plants of the United States: a Bibliography
Humboldt State University Digital Commons @ Humboldt State University Botanical Studies Open Educational Resources and Data 5-2020 Poisonous and Injurious Plants of the United States: A Bibliography James P. Smith Jr Humboldt State University, [email protected] Follow this and additional works at: https://digitalcommons.humboldt.edu/botany_jps Part of the Botany Commons Recommended Citation Smith, James P. Jr, "Poisonous and Injurious Plants of the United States: A Bibliography" (2020). Botanical Studies. 67. https://digitalcommons.humboldt.edu/botany_jps/67 This Poisonous Plants is brought to you for free and open access by the Open Educational Resources and Data at Digital Commons @ Humboldt State University. It has been accepted for inclusion in Botanical Studies by an authorized administrator of Digital Commons @ Humboldt State University. For more information, please contact [email protected]. POISONOUS & INJURIOUS PLANTS OF THE UNITED STATES: A BIBLIOGRAPHY James P. Smith, Jr. Professor Emeritus of Botany Department of Biological Sciences Humboldt State University Arcata, California 23 May 2020 TABLE OF CONTENTS 1 • Introduction. 1 2 • General References . 2 3 • Symptoms & Sites . 8 4 • Poisonous Principles (Toxins). 12 5 • Food & Beverage Plants . 17 6 • Plants of Home & Garden . 19 7 • Medicinal Plants . 20 8 • Plants Poisonous to Pets & Horses . 21 9 • Purposeful Uses of Poisonous Plants Arrow and Dart Poisons. 22 Fish Poisons (Piscicides) . 23 Insecticides . 24 Rat Poisons (Raticides) . 25 Snail Poisons (Molluscides) . 25 10 • Plants by Major Group and Family Lycophytes . 26 Ferns. 26 Gymnosperms . 28 Flowering Plants . 30 11 • Plants by Region & State. 82 12 • Plants by Common & Scientific Names . 88 13 • Plants by Genus and Family .