The Treatment of Drinking Problems a Guide for the Helping Professions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

THOMAS TROTTER Biography
Download as a Word doc THOMAS TROTTER Biography Thomas Trotter is one of Britain’s most widely admired musicians. The excellence of his musicianship is reflected internationally in his musical partnerships. He performs as soloist with, amongst many others, the conductors Sir Simon Rattle, Bernard Haitink, Riccardo Chailly and Sir Charles Mackerras. He has performed in Berlin’s “Philharmonie”, the “Gewandhaus” in Leipzig, the “Concertgebouw” in Amsterdam, the “Musikverein” and the “Konzerthaus” in Vienna and London’s Royal Festival Hall. He has played inaugural concerts in places such as Princeton University Chapel USA, Auckland Town Hall in New Zealand, the Royal Albert Hall London, and Moscow's International Performing Arts Centre. He won the Royal Philharmonic Society award for Best Instrumentalist in 2002, and in 2012 he was named International Performer of the Year by the New York Chapter of the American Guild of Organists. In 2016 he was awarded the Gold Medal of the Royal College of Organists for his achievements in organ playing. Thomas Trotter was appointed Birmingham City Organist in 1983 in succession to Sir George Thalben-Ball, and he is also Organist at St Margaret’s Church, Westminster Abbey and Visiting Fellow in Organ Studies at the Royal Northern College of Music. Earlier in his career he was organ scholar at King’s College, Cambridge, winning the First Prize at the St Albans International Organ Competition in his final year. He received an Honorary Doctorate from Birmingham City University in 2003 and from Birmingham University in 2006. Alongside his regular recitals in Birmingham, Thomas Trotter tours on four continents and plays at many international festivals such as Bath, Salzburg, and the BBC Proms. -

Chronology of the Addiction Recovery Advocacy Movement
Chronology of the Addiction Recovery Advocacy Movement Pat Taylor, Tom Hill and William White We’ve described the rich history of people in recovery, family members, friends and allies coming together to support recovery by highlighting key moments from the 1700s leading up to the present day. Please join us in acknowledging the shoulders we stand on and in forging a movement that embraces recovery as a civil right for all Americans and people all across the world. Earlier Organizing Efforts 1730s- 1830s Abstinence-based, Native American religious and cultural revitalization movements mark the first recovery focused advocacy efforts in North America. 1799 Prophet-led Recovery Movements: Handsome Lake (1799), Shawnee Prophet (Tenskwatawa, 1805), Kickapoo Prophet (Kennekuk, 1830s) 1840s The Washingtonian movement marks the first Euro-American movement organized by and for those recovering from alcoholism—a movement that involved a public pledge of sobriety and public acknowledgement of one’s recovery status. 1840s Conflict within Washingtonian societies rises over the question of legal prohibition of the sale of alcohol and the role of religion in recovery; recovering alcoholics go underground in following decades within fraternal temperance societies and ribbon reform clubs. 1845 Frederick Douglass acknowledges past intemperance, signs temperance pledge and becomes central figure in “Colored Temperance Movement”—framing sobriety as essential for full achievement of citizenship. 1895 Keeley League members (patient alumni association of the Keeley Institutes—a national network of addiction cure institutes) march on the Pennsylvania capital in support of a Keeley Law that would provide state funds for people who could not afford the Keeley cure. -

Choral Secular Music Through the Ages
Choral Secular Music through the ages The Naxos catalogue for secular choral music is such a rich collection of treasures, it almost defi es description. All periods are represented, from Adam de la Halle’s medieval romp Le Jeu de Robin et Marion, the earliest known opera, to the extraordinary fusion of ethnic and avant-garde styles in Leonardo Balada’s María Sabina. Core repertoire includes cantatas by J.S. Bach, Beethoven’s glorious Symphony No. 9, and a “must have” (Classic FM) version of Carl Orff’s famous Carmina Burana conducted by Marin Alsop. You can explore national styles and traditions from the British clarity of Elgar, Finzi, Britten and Tippett, to the stateside eloquence of Eric Whitacre’s “superb” (Gramophone) choral program, William Bolcom’s ‘Best Classical Album’ Grammy award winning William Blake songs, and Samuel Barber’s much loved choral music. Staggering emotional range extends from the anguish and passion in Gesualdo’s and Monteverdi’s Madrigals, through the stern intensity of Shostakovich’s Execution of Stepan Razin to the riot of color and wit which is Maurice Saylor’s The Hunting of the Snark. Grand narratives such as Handel’s Hercules and Martinů’s Epic of Gilgamesh can be found alongside tender miniatures by Schubert and Webern. The Naxos promise of uncompromising standards of quality at affordable prices is upheld both in performances and recordings. You will fi nd leading soloists and choirs conducted by familiar names such as Antoni Wit, Gerard Schwarz, Leonard Slatkin and Robert Craft. There is also a vast resource of collections available, from Elizabethan, Renaissance and Flemish songs and French chansons to American choral works, music for children, Red Army Choruses, singing nuns, and Broadway favorites – indeed, something for everyone. -
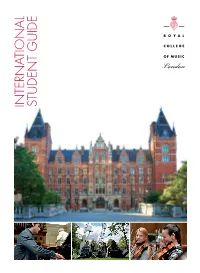
RCM International Student Guide.Pdf
INTERNATIONAL STUDENT GUIDE TOP WITH MORE THAN CONSERVATOIRE FOR 800 PERFORMING ARTS STUDENTS IN THE UK, SECOND IN FROM MORE THAN EUROPE AND JOINT THIRD IN THE WORLD QS WORLD UNIVERSITY RANKINGS 2016 60 COUNTRIES THE RCM IS AN INTERNATIONAL LOCATED OPPOSITE THE COMMUNITY ROYAL IN THE HEART OF LONDON ALBERT HALL HOME TO THE ANNUAL TOP UK SPECIALIST INSTITUTION BBC PROMS FESTIVAL FOR MUSIC COMPLETE UNIVERSITY GUIDE 2017 100% OF SURVEY RESPONDENTS IN OVER OF EMPLOYMENT OR 40% FURTHER STUDY STUDENTS BENEFIT FROM SIX MONTHS AFTER GRADUATION FOR SCHOLARSHIPS THREE CONSECUTIVE YEARS HIGHER EDUCATION STATISTICS AGENCY SURVEY CONCERTS AND MASTERCLASSES TOP LONDON WATCHED IN CONSERVATOIRE COUNTRIES FOR WORLD-LEADING WORLDWIDE IN 2014 75 RESEARCH VIA THE RCM’s RESEARCH EXCELLENCE FRAMEWORK YOUTUBE CHANNEL 2 ROYAL COLLEGE OF MUSIC / WWW.RCM.AC.UK WELCOME The Royal College of Music is one of the world’s greatest conservatoires, training gifted musicians from all over the globe for a range of international careers as performers, conductors and composers. We were proud to be ranked the top conservatoire for performing arts in the UK, second in Europe and joint third in the world in the 2016 QS World University Rankings. The RCM provides a huge Founded in 1882 by the future King Edward VII, number of performance the RCM has trained some of the most important opportunities for its students. figures in British and international music life. We hold more than 500 Situated opposite the Royal Albert Hall, our events a year in our building and location are the envy of the world. -

Temperance," in American History Through Literature, 1820- 1870
Claybaugh, Amanda. "Temperance," in American History Through Literature, 1820- 1870. Eds. Janet Gabler-Hover and Robert Sattlemeyer. Detroit: Charles Scribner's Sons, 2006, 1152-58. TEMPERANCE The antebellum period was famously a time of social reform Reformers agitated for the abolition of slavery and the expansion of women's rights, but they also renovated prisons and poorhouses and instituted mental asylums and schools for the deaf and the blind. They passed out religious tracts and insisted that the Sabbath be observed. They improved sewers and drains, inspected the homes of the poor, and cam- paigned against the death penalty and for world peace. They lived in communes, rejected fashion in favor of rational dress, and took all sorts of water cures. But above all else, they advocated temperance reform. Antebellum temperance reform was the largest mass . movement in United States history—and certainly one i of the most influential. Temperance reform unfolded in five sometimes ; ovei l a p p i n g phases: (1) the licensing movement of the , eighteenth century, (2) the moderationist societies of the early nineteenth century, (3) the temperance soci- f eties of the early to mid-nineteenth century, (4) the teetotal societies of the mid-nineteenth century, and (5) the prohibitionist movement of the mid-nine- teenth century. The essay that follows will sketch out "•' the history of temperance reform, pausing to consider -, four milestone temperance texts, and will conclude by discussing the effects that temperance reform had on the non-canonical and canonical literary texts of the antebellum period. H I THROUGH LITERATURE, 1820-187 0 A>1 TEMPERANCE THE PREHISTORY OF TEMPERANCE Mather is anticipating the form that temperance activ- REFORM: LICENSING ity would take throughout the eighteenth century, Throughout the seventeenth century and much of the when the so-called licensing movement would seek to eighteenth, drinking was frequent and alcohol was abun- ensure that drinking houses and the drink trade re- dant. -

Choir & Organ Magazine – Major Plans
NEWS & PREVIEWS Major plans announced for RFH organ launch Ensemble, the London Philharmonic Brass Ensemble, Voicelab and the Elysian Singers; in addition to music by Gigout, Bach, Mendelssohn, Dupré, Franck and Liszt, the programme will include the premieres of commissions from Sir John HAYES DAVIDSON NICK ROCHOWSKI DAVIDSON HAYES Tavener and Sir Peter Maxwell Davies. Celebrity recitals will be given by John Scott (21 Mar), Thomas Trotter (24 Mar, with the world premiere of Judith Weir’s The Wild Reeds), Olivier Latry (27 Mar, performing a four-hand arrangement of Stravinsky’s Rite of Spring with his wife Shin-Young Lee) and Bernard Foccroulle (11 April, including Darkness and Light, a collaboration with video and fi lm artist Lynette Wallworth). Special events include Cameron Carpenter (29 Mar) playing Generated image of the restored organ in the an improvised accompaniment to the Royal Festival Hall German Expressionist 1920s horror fi lm The Cabinet of Dr Caligari, and Face to WITH ONE YEAR TO GO before the Pull concert. Ralph himself played in the series Face with Bach – an event devised by visual Out All The Stops Festival – An Organ every year and on one occasion I turned artist and composer Martin Creed. Celebration in March 2014, Choir & pages for him. I remember to this day the A programme of orchestral concerts Organ readers are invited to contribute horrible sensation of walking across the will feature the organ: James O’Donnell to Southbank Centre’s new project to empty stage of the Royal Festival Hall up performs the Poulenc Organ Concerto collect the public’s memories of the organ, to the organ console as a self-conscious and Saint-Saëns’s Symphony no.3 with writes Graeme Kay. -

City of Birmingham Choir Concerts from 1964
City of Birmingham Choir concerts from 1964. Concerts were conducted by Christopher Robinson and took place in Birmingham Town Hall with the CBSO unless otherwise stated. Messiah concerts and Carols for All concerts are listed separately. 1964 Mar 17 Vaughan Williams: Overture ‘The Wasps’ Finzi: Intimations of Immortality Vaughan Williams: Dona Nobis Pacem Elizabeth Simon John Dobson Peter Glossop Christopher Robinson conducts the Choir for the first time Jun 6 Britten: War Requiem Heather Harper Wilfred Brown Thomas Hemsley Performed in St Alban’s Abbey Meredith Davies’ final concert as conductor of the Choir Nov 11 & 12 Britten: War Requiem (Nov 11 in Wolverhampton Civic Hall Nov 12 in Birmingham Town Hall) Jacqueline Delman Kenneth Bowen John Shirley-Quirk Boy Choristers of Worcester Cathedral CBSO concert conducted by Hugo Rignold 1965 Feb 27 Rossini: Petite Messe Solennelle Barbara Elsy Janet Edmunds Gerald English Neil Howlett Colin Sherratt (Piano) Harry Jones (Piano) David Pettit (Organ) Performed in the Priory Church of Leominster Mar 11 Holst: The Planets CBSO concert conducted by Hugo Rignold Mar 18 Beethoven: Choral Symphony Jennifer Vyvyan Norma Proctor William McAlpine Owen Brannigan CBSO concert conducted by Hugo Rignold Mar 30 Elgar: The Dream of Gerontius Marjorie Thomas Alexander Young Roger Stalman May 18 Duruflé: Requiem Poulenc: Organ Concerto Poulenc: Gloria Elizabeth Harwood Sybil Michelow Hervey Alan Roy Massey (Organ) 34 Jun 2 Rossini: Petite Messe Solennelle Elizabeth Newman Miriam Horne Philip Russell Derek -

Review Organist Thomas Trotter in Elegant Recital at St
Review Organist Thomas Trotter in Elegant Recital at St. John's Cathedral (November 19) by Timothy Robson Thomas Trotter, for the past thirty years the Birm- ingham (England) City Organist, appeared at the Cathedral of St. John the Evangelist in Cleveland on Tuesday evening, November 19, for a recital sponsored jointly by St. John's Cathedral, Trinity Episcopal Cathedral and the Cleveland Chapter of the American Guild of Organists. It was an ele- gant and satisfying concert from beginning to end. In the 19th and early 20th centuries, before the in- vention of electronic recording devices, cities in Europe—especially in England—and the United States built large pipe organs in public auditori- ums. These city-funded facilities were for the purposes of the musical education and en- tertainment of the citizens, especially in places where there was no symphony orchestra. The city organist was expected to perform transcriptions of orchestral and chamber works, light and "novelty" music and patriotic marches, as well as literature written for the organ. (Indeed, Cleveland had such an organ and incumbent in the Public Auditorium downtown.) One of the most famous and still thriving public organs in England is the Birmingham Town Hall, built in 1834, where Thomas Trotter performs and records regu- larly. He also gives recitals on the 2001 Klais organ in Birmingham Symphony Hall. This was a model sample of the sorts of programs a good municipal organist might give, performed on the 1948 Holtkamp organ in the rear gallery of the cathedral. The organist is normally hidden from view by the organ pipes, however, the presenters had installed a large projection video screen at the front of the nave that enabled the audience to see the performer. -

Recovery-Related Studies
Addiction Recovery: A Selected Bibliography with an Emphasis on Professional Publications and Scientific Studies (January 2014) William L. White, M.A. ([email protected]) Introduction This topical bibliography is intended as a supplement to a recovery management monograph series developed through the sponsorship of the Center for Substance Abuse Treatment’s Great Lakes Addiction Technology Transfer Center, the Institute for Research Education and Training in Addiction, and the Philadelphia Department of Behavioral Health and Developmental disAbilities. It is hoped this will help interested readers locate classic and important contemporary papers related to the resolution of alcohol and other drug problems. Many key documents related to recovery management and recovery-oriented systems of care are also posted at the following web sites: http://www.dbhids.org/transformation-tools-2/ http://www.attcnetwork.org/find/respubs/index.asp http://www.bhrm.org/ http://www.williamwhitepapers.com/ Toward a Recovery Paradigm Best, D., Groshkova, T. & McTague, P. (2009). The politics of recovery. Druglink, 14- 19. Berridge, V. (2012). The rise, fall, and revival of recovery in drug policy. Lancet, 379, 22-23. Borkman, T. (1976). Experiential knowledge: A new concept for the analysis of self- help groups. Social Service Review, 50, 443-456. Borkman, T. J. (1997). Is recovery planning any different from treatment planning? Journal of Substance Abuse Treatment, 15(1), 37-42. doi:10.1016/S0740- 5472(97)00247-X Center for Substance Abuse Treatment (CSAT). (2007). National Summit on Recovery: Conference report (DHHS Publication No. SMA 07-4276). Rockville, MD: Substance Abuse and Mental Health Services Administration. Clark, W. (2007). -

August 2021 Summer Quarter
PIPEDREAMS Programs, August 2021 Summer Quarter: The following listings detail complete contents for the Aigist 2021 Summer Quarter broadcasts of PIPEDREAMS. The first section includes complete program contents, with repertoire, artist, and recording information. Following that is program information in "short form". For more information, contact your American Public Media station relations representative at 651-290-1225/877- 276-8400 or the PIPEDREAMS Office (651-290-1539), Michael Barone <[email protected]>). For last-minute program changes, watch DACS feeds from APM and check listing details on our PIPEDREAMS website: http://www.pipedreams.org AN IMPORTANT NOTE: It would be prudent to keep a copy of this material on hand, so that you, at the local station level, can field listener queries concerning details of individual program contents. That also keeps YOU in contact with your listeners, and minimizes the traffic at my end. However, whenever in doubt, forward calls to me (Barone). * * * * * * PIPEDREAMS Program No. 2131 (distribution on 8/2/2021) Methuen Memories . selections from the 75th anniversary season of the famous Walcker/Aeolian- [Hour 1] SIR WALTER ALCOCK: Marche Triumphale. HEALEY WILLAN: Andante, Fugue & Chorale –Adam Pajan (r. 6/9/21) HANRE SOL: Solitude (2020). JONATHAN DOVE: The Dancing Pipes (2014) –Michael Hey (r. 5/19/21) DMITRI SHOSTAKOVICH (arr. Joos): Andante, fr Piano Concerto No. 2, Op. 102 –Shaylen Joos, harp. MAURICE DURUFLÉ: Prelude & Fugue on the Name ALAIN, Op. 7 –Marshall Joos (r. 5/10/21) [Hour 2] J. S. BACH: Komm, heiliger Geist, here Gott, BWV 651 –Bridgette Wargovich (r. 5/26/21) SAMUEL BARBER: To Longwood Gardens. -

RCM A4 Word Template (Futura)
PRESS RELEASE Embargoed until 20 November 2017 Embargoed until 20 November 2017 Royal College of Music to unveil new organ custom built by world-renowned Flentrop Orgelbouw Designed to complement the College’s Amaryllis Fleming Concert Hall in design and sound, the organ is an exceptional new facility for RCM students The Royal College of Music (RCM) today announced that its new organ will be unveiled to the public in spring 2018. The organ has been custom built by Flentrop Orgelbouw to service the specific requirements of teaching and performance at the College, which has a prestigious history of organ training and many distinguished organ alumni including Dame Gillian Weir, Ralph Downes, Wayne Marshall, Timothy Wakerell and Nicohlas Danby. The new instrument is part of the RCM’s More Music project, which represents a once-in-a-generation opportunity to transform the College’s facilities. With 34 stops over three manuals and pedals, the RCM’s new organ was designed with an emphasis on beauty of tone and voiced for the particular acoustic of the Amaryllis Fleming Concert Hall. Its aesthetic is in the Dutch and North German traditions. The instrument has a case of Limousin oak, with gilding to echo the decoration of the hall. The keyboard has a suspended mechanical action and the sound is fed by two large V-fold bellows with a relatively low wind pressure to achieve a warm, prominent tone, ideal for the Amaryllis Fleming Concert Hall’s lively acoustic. Organ students at the Royal College of Music currently have access to the conservatoire’s collection of a further six organs, which include three mechanical action instruments, as well as enjoying opportunities to play and learn at numerous locations across London, including the Royal Albert Hall, St George’s Hanover Square and Christ Church Chelsea. -

City of Birmingham Choir Concerts from 2002 Concerts Conducted by Adrian Lucas with the CBSO in Symphony Hall Unless Otherwise Stated
City of Birmingham Choir concerts from 2002 Concerts conducted by Adrian Lucas with the CBSO in Symphony Hall unless otherwise stated. 2002 May 18 Walton: Coronation Te Deum Elgar: Cello Concerto Walton: The Twelve Walton: Belshazzar’s Feast Willard White Paul Watkins (Cello) Walton Centenary Concert Pre-concert talk by Michael Aston Christopher Robinson conducted his farewell concert July 2 Golden Jubilee Concert Walton: Coronation Te Deum Performed with Worcester Cathedral Choristers and the CBSO conducted by Sakari Oramo as part of the Queen’s Golden Jubilee Celebrations A number of other artists and groups took part in the presence of Her Majesty Queen Elizabeth II and The Duke of Edinburgh Nov 2 Mendelssohn: Elijah Sarah Fox Elinor Carter Lynton Atkinson William Clements Six treble choristers from Worcester Cathedral Pre-concert talk by Lyndon Jenkins Adrian Lucas conducts the Choir for the first time Dec 6 & 10 Handel: Messiah Geraldine McGreevy Catherine King Edward Lyon William Clements Dec 15 Carols for All Anna Huntley (soprano) Roy Massey (organ) Cambrian Brass Anna Huntley was the winner of the Singing Challenge 2003 Apr 12 Handel: Dixit Dominus Mozart: Mass in C Minor Ruth Holton Katharine Fuge Emily Bauer-Jones Robert Johnston Robert Rice May 10 Evensong in St John’s College, Cambridge By invitation some members joined the choristers of St John’s Conducted by Christopher Robinson 1 Jun 21 Music for a Summer Evening - Worcester Cathedral Vaughan Williams: Shakespeare Songs and Five Mystical Songs Finzi: Magnificat Britten: